Back
Neonatal General
Category: Abstract Submission
Neonatology General 11: Lung
369 - Thoracic fluid content as measured by bioimpedance is not associated with respiratory outcome or death in very preterm infants
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 369
Publication Number: 369.440
Publication Number: 369.440
David B. Healy, University College Cork, Cork, Cork, Ireland; Roberto Chioma, INFANT Research Centre, Cork, Cork, Ireland; John M. O'Toole, University College Cork, Cork, Cork, Ireland; Vicki Livingstone, University College Cork, Cork, Cork, Ireland; Jurate Panaviene, INFANT, UCC, Cork, Cork, Ireland; Eugene Dempsey, University Colleeg Cork, Cork, Cork, Ireland; Christoph E. Schwarz, University of Tübingen, Tübingen, Baden-Wurttemberg, Germany

David Healy, MB, BaO, Bch, BSc (he/him/his)
Research Fellow
University College Cork
Cork, Cork, Ireland
Presenting Author(s)
Background: High thoracic fluid content (TFC), as measured using bioimpedance, has been shown to correlate with respiratory outcomes in critically ill paediatric patients and with respiratory distress in term newborns. However, there is little work done on TFC in preterm infants.
Objective: To investigate whether median TFC measurements across the first 48 hours of life were associated with an adverse outcome (diagnoses of bronchopulmonary dysplasia (BPD) at 36 weeks corrected gestational age or death in the first 2 weeks of life) and to examine if changes in TFC over that time differed by adverse event group.
Design/Methods: This was a post-hoc analysis of a prospective observational study which enrolled infants born less than 32 weeks' gestation age (GA) at a tertiary neonatal unit. Exclusion criteria were major congenital anomalies including congenital heart defects (except patent ductus arteriosus or inter-atrial shunting) and refusal of parental informed consent. TFC values were obtained from continuous electrical cardiometry (ICON, Osypka Medical) starting as soon as possible after birth until 48 hours of life. Logistic regression models were used to investigate the association between median TFC and an adverse outcome and a linear mixed model was used to examine if changes in TFC in the first 48 hours of life differed by adverse outcome group.
Results: Fifty-four preterm infants (median [IQR] GA 29+0 [25+4 - 30+4] weeks + days, birth weight 1000 [748 - 1497] grams) were included in the analysis. Adverse outcome (BPD/death) occurred in 20 infants. Median(IQR) TFC was 26.2(22.7-32.9) for infants with an adverse outcome and 28.8(22.3 - 39.4) for those without an adverse outcome. Median TFC across the first 48 hours of life was not associated with an adverse outcome of BPD/Death (odds ratio(95% CI): 0.95(0.89-1.01), p=0.112; odds ratio adjusted for GA group(95% CI): 0.95(0.89 to 1.02), p=0.193)). There was no significant difference between the groups in TFC trajectory over time (Figure 1).Conclusion(s): TFC measurement in very preterm neonates is not well studied. We found no association between TFC recorded within the first 48 hours and BPD or mortality. TFC may have more utility outside the transitional period, but it does not appear to be clinically relevant in the first 48 hours.
Figure 1. TFC trajectory over time by group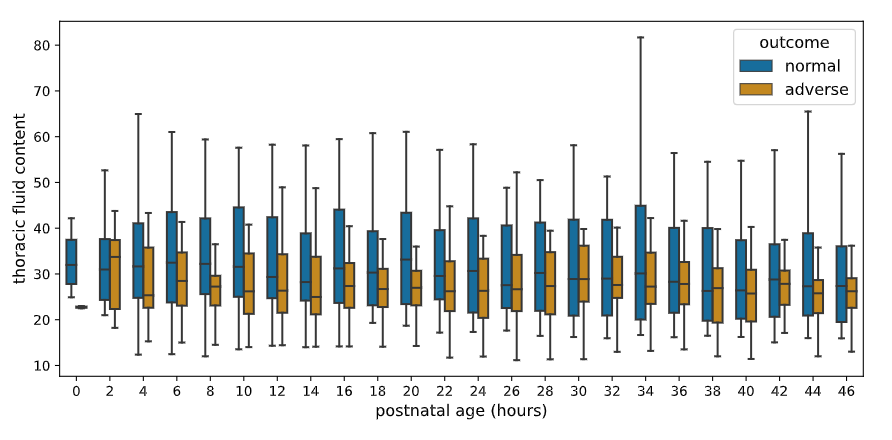 Box plots for median TFC values over 2-hourly windows for the first 48 hours of life and grouped by adverse compared to normal outcome.
Box plots for median TFC values over 2-hourly windows for the first 48 hours of life and grouped by adverse compared to normal outcome.
Objective: To investigate whether median TFC measurements across the first 48 hours of life were associated with an adverse outcome (diagnoses of bronchopulmonary dysplasia (BPD) at 36 weeks corrected gestational age or death in the first 2 weeks of life) and to examine if changes in TFC over that time differed by adverse event group.
Design/Methods: This was a post-hoc analysis of a prospective observational study which enrolled infants born less than 32 weeks' gestation age (GA) at a tertiary neonatal unit. Exclusion criteria were major congenital anomalies including congenital heart defects (except patent ductus arteriosus or inter-atrial shunting) and refusal of parental informed consent. TFC values were obtained from continuous electrical cardiometry (ICON, Osypka Medical) starting as soon as possible after birth until 48 hours of life. Logistic regression models were used to investigate the association between median TFC and an adverse outcome and a linear mixed model was used to examine if changes in TFC in the first 48 hours of life differed by adverse outcome group.
Results: Fifty-four preterm infants (median [IQR] GA 29+0 [25+4 - 30+4] weeks + days, birth weight 1000 [748 - 1497] grams) were included in the analysis. Adverse outcome (BPD/death) occurred in 20 infants. Median(IQR) TFC was 26.2(22.7-32.9) for infants with an adverse outcome and 28.8(22.3 - 39.4) for those without an adverse outcome. Median TFC across the first 48 hours of life was not associated with an adverse outcome of BPD/Death (odds ratio(95% CI): 0.95(0.89-1.01), p=0.112; odds ratio adjusted for GA group(95% CI): 0.95(0.89 to 1.02), p=0.193)). There was no significant difference between the groups in TFC trajectory over time (Figure 1).Conclusion(s): TFC measurement in very preterm neonates is not well studied. We found no association between TFC recorded within the first 48 hours and BPD or mortality. TFC may have more utility outside the transitional period, but it does not appear to be clinically relevant in the first 48 hours.
Figure 1. TFC trajectory over time by group
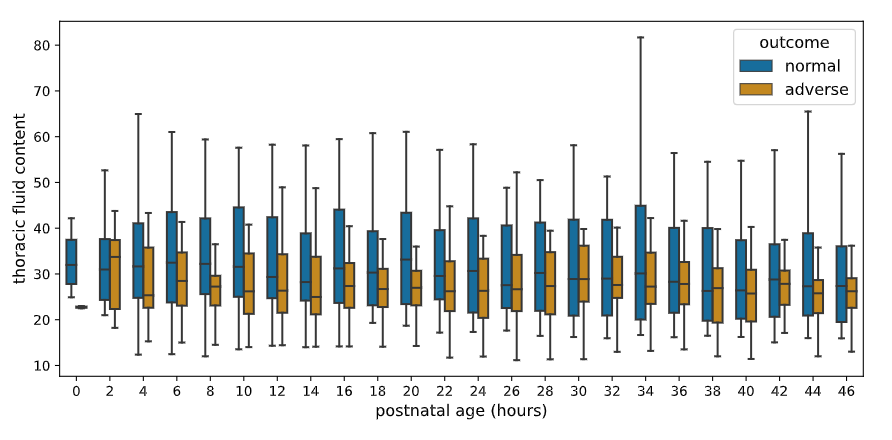 Box plots for median TFC values over 2-hourly windows for the first 48 hours of life and grouped by adverse compared to normal outcome.
Box plots for median TFC values over 2-hourly windows for the first 48 hours of life and grouped by adverse compared to normal outcome.