Back
Neonatal General
Category: Abstract Submission
Neonatology General 11: Lung
366 - Predictors of Home Oxygen Therapy in Very Low Birth Weight Infants
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 366
Publication Number: 366.440
Publication Number: 366.440
Yijun Shao, LAC+USC Medical Center, San Francisco, CA, United States; Alexis Hisey, LAC + USC Medical Center, Los Angeles, CA, United States; Nagapranati S. Nanduri, LAC+USC Medical Center Neonatology, Philadelphia, PA, United States; Kate E. Ramm, LAC+USC Medical Center, Newport Beach, CA, United States; Christiana Marquez, LAC USC Medical Center, Yorba Linda, CA, United States; Rangasamy Ramanathan, Keck School of Medicine of USC, Los Angeles, CA, United States; Manoj Biniwale, USC Keck School of Medicine, Los Angeles, CA, United States
Yijun Shao
Neonatalogy Researcher
LAC+USC Medical Center
San Francisco, California, United States
Presenting Author(s)
Background: Very low birth weight (VLBW) infants with prolonged respiratory morbidities such as bronchopulmonary dysplasia (BPD) may need to be discharged home while receiving oxygen therapy. The risk factors causing prolonged respiratory support vary for these infants.
Objective: The study was performed to characterize factors associated with VLBW infants who require oxygen therapy at discharge.
Design/Methods: Data on all VLBW infants was gathered from the electronic medical record between the years of 2009 and 2021 retrospectively with IRB approval obtained prior. Oxygen therapy was statistically analyzed using SPSS Version 28 statistical software against early neonatal outcomes such as ventilation, intubation, chest compressions, or surfactant, or against common neonatal morbidities, including IVH, BPD, ROP, and patent ductus arteriosus (PDA).
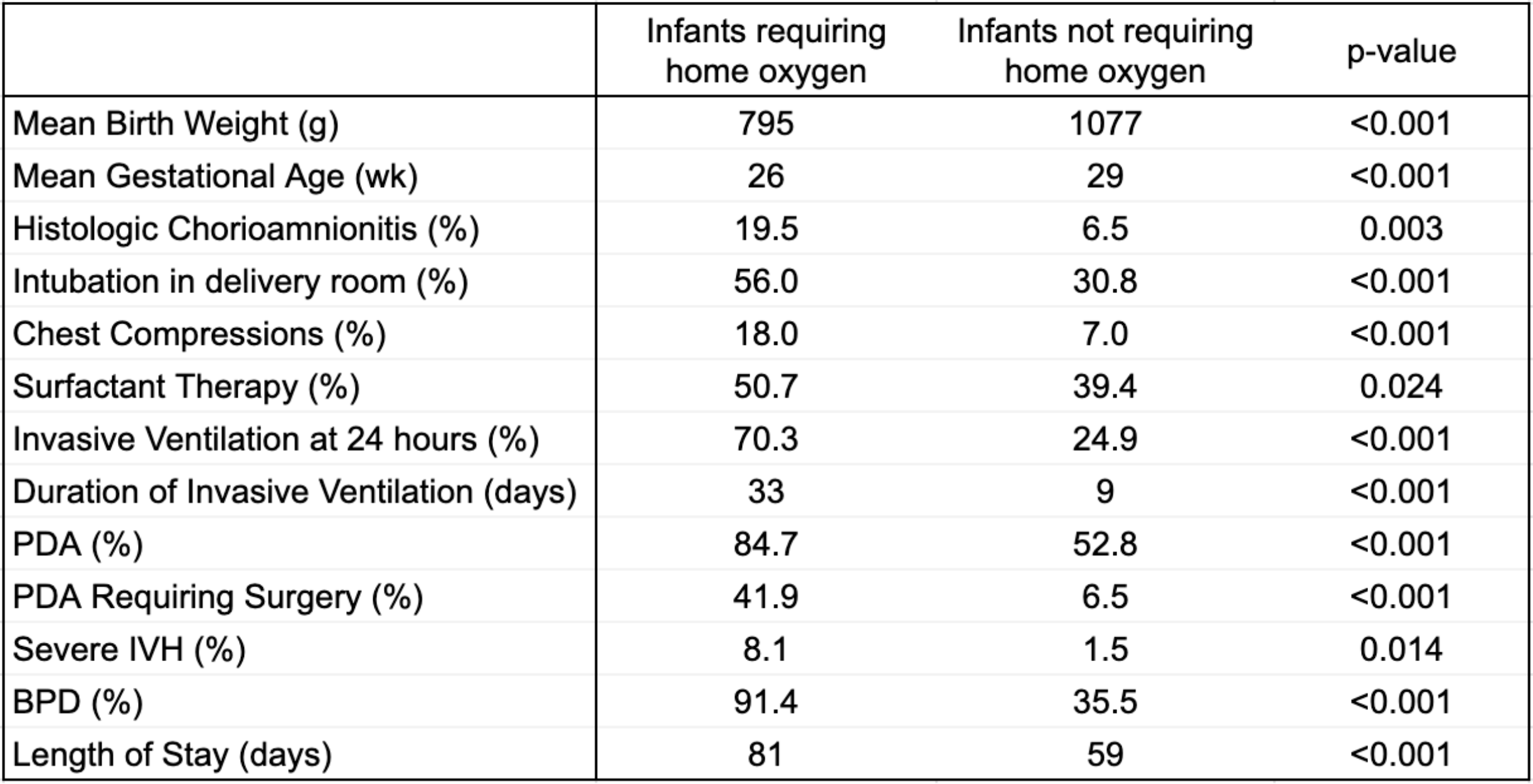
Results: Of 560 VLBW infants, 144 (25.7%) were discharged home on oxygen. Significant maternal risk factors included histologic chorioamnionitis, intubation, and chest compressions at delivery. These infants had lower gestational age as well as lower birth weight. These infants were more likely to require surfactant, invasive ventilation at 24 hours, and receive additional ventilatory support including high-frequency oscillatory ventilation or jet ventilation (Table 1). Infants who were discharged with home oxygen therapy were significantly more likely to have BPD and hemodynamically significant patent ductus arteriosus (PDA) requiring surgery. Associated comorbidities included retinopathy of prematurity (ROP) requiring treatment, severe intraventricular hemorrhage (IVH), and increased length of stay in NICU (Table 1). Regression analysis revealed lower birth weight, longer duration of invasive ventilation, PDA requiring surgical intervention, and BPD to be the most significant predictors.Conclusion(s): The need for high-frequency ventilation such as jet and oscillatory ventilation is associated with home oxygen need at discharge. Additionally, VLBW infants who required home oxygen therapy were more likely to have needed invasive ventilation, intubation and chest compressions in the delivery room, and surfactant therapy. They were also more likely to have common neonatal morbidities such as BPD, severe IVH, severe ROP, and PDA.
Significant neonatal factors predicting home oxygen therapy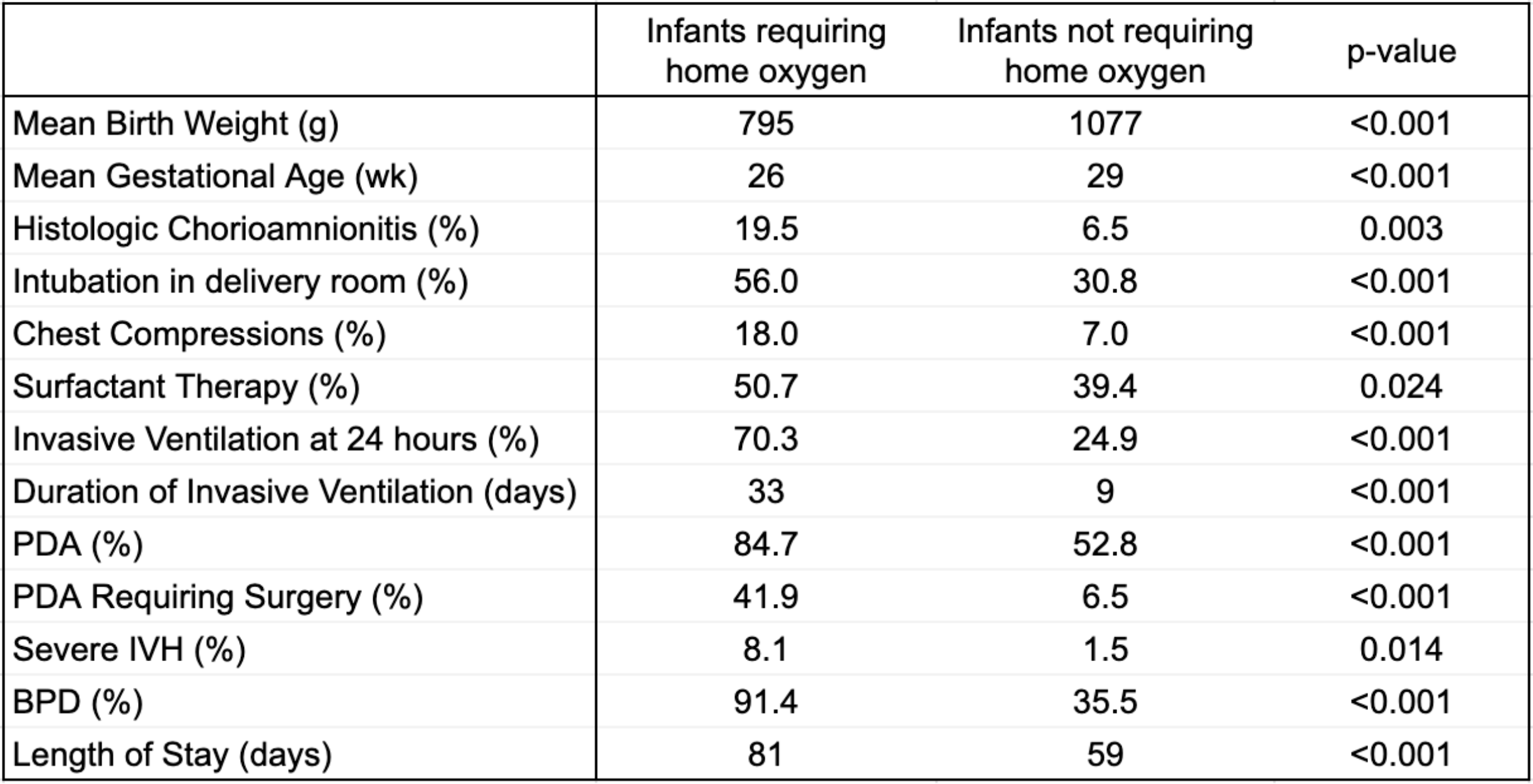
Objective: The study was performed to characterize factors associated with VLBW infants who require oxygen therapy at discharge.
Design/Methods: Data on all VLBW infants was gathered from the electronic medical record between the years of 2009 and 2021 retrospectively with IRB approval obtained prior. Oxygen therapy was statistically analyzed using SPSS Version 28 statistical software against early neonatal outcomes such as ventilation, intubation, chest compressions, or surfactant, or against common neonatal morbidities, including IVH, BPD, ROP, and patent ductus arteriosus (PDA).
Results: Of 560 VLBW infants, 144 (25.7%) were discharged home on oxygen. Significant maternal risk factors included histologic chorioamnionitis, intubation, and chest compressions at delivery. These infants had lower gestational age as well as lower birth weight. These infants were more likely to require surfactant, invasive ventilation at 24 hours, and receive additional ventilatory support including high-frequency oscillatory ventilation or jet ventilation (Table 1). Infants who were discharged with home oxygen therapy were significantly more likely to have BPD and hemodynamically significant patent ductus arteriosus (PDA) requiring surgery. Associated comorbidities included retinopathy of prematurity (ROP) requiring treatment, severe intraventricular hemorrhage (IVH), and increased length of stay in NICU (Table 1). Regression analysis revealed lower birth weight, longer duration of invasive ventilation, PDA requiring surgical intervention, and BPD to be the most significant predictors.Conclusion(s): The need for high-frequency ventilation such as jet and oscillatory ventilation is associated with home oxygen need at discharge. Additionally, VLBW infants who required home oxygen therapy were more likely to have needed invasive ventilation, intubation and chest compressions in the delivery room, and surfactant therapy. They were also more likely to have common neonatal morbidities such as BPD, severe IVH, severe ROP, and PDA.
Significant neonatal factors predicting home oxygen therapy