Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement VI
406 - Quality Improvement via Plan-Do-Study-Act Methodology to Reduce Central Line-Associated Bloodstream Infections in the Neonatal Intensive Care Unit
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 406
Publication Number: 406.436
Publication Number: 406.436
Samantha J. King, University of Minnesota Medical School, Richfield, MN, United States; Krystina Kalland, University of Minnesota Medical School, Minneapolis, MN, United States; Soraya Riley, Fairview M Health, St. Paul, MN, United States; Emily Vadner, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Julianne Cramer, MHealth Fairview, Minneapolis, MN, United States; Erin A. Osterholm, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States

Samantha J. King, Medical Student
Medical Student
University of Minnesota Medical School
Richfield, Minnesota, United States
Presenting Author(s)
Background: Central line-associated bloodstream infections (CLABSI) in the Neonatal Intensive Care Unit (NICU) contribute to a high rate of morbidity and mortality. The quality improvement (QI) team at University of Minnesota-Masonic Children’s Hospital (UMMCH) implemented a Plan-Do-Study-Act (PDSA) process improvement methodology as a multi-faceted effort to reduce CLABSI incidence.
Objective: To evaluate the efficacy of process mapping methodologies including CurosTM Caps, venous access device (VAD) algorithms, clean space recommendations and provider educational tools on prevention of neonatal CLABSI through analysis of central line days (CLDs) and overall unit infection rates.
Design/Methods: A multidisciplinary team (advanced practice nursing leaders, nurses, MDs, APPs, QI consultant, and medical students) was assembled to analyze CLABSI incidence and risk factors, brainstorm interventions, and audit results following implementation of PDSAs. Study population included all infants in the UMMCH NICU over a 3 year period (2019-2021) with CLABSI defined per NHSN criteria. Retrospective review of CLABSI rate per 1000 CLDs and overall unit infection rates (CLABSI cases ÷ number of central lines removed), was performed for 18 months prior to PDSA intervention and 16 months following the start of PDSA testing rollout. Pre- and post- PDSA CLABSI results were compared using two sample t-test and chi square to determine statistical significance.
Results: The incidence of CLABSI before PDSA implementation (January 2019 - June 2020) and after PDSA implementation (July 2020 - October 2021) were 3.34% (n = 23/689) and 1.27% (n = 9/706), respectively with statistical significance via chi-square test (p = 0.01). CLABSI rates per 1000 CLDs before PDSA implementation and after PDSA implementation were 2.28 and 1.16, respectively, a 49% decrease in CLABSI rate per 1,000 CLDs. A two sample t-test of CLABSI rates per 1,000 CLDs revealed no statistical significance post-PDSA (p-value 0.10, 95% CI: [-2.33,0.92]) compared to pre-PDSA.Conclusion(s): PDSA interventions produced a statistically significant decrease in CLABSI incidence. PDSA implementation resulted in a clinically evident decrease in CLABSI rates per 1,000 CLDs in the UMMCH NICU, though not statistically significant. Continued quality improvement efforts are aimed at further decreasing risk factors including the time that central lines are in place, decreasing the frequency of line access, and improving the sterility of central lines. These efforts are required to continue improvement of CLABSI rates and decrease morbidity and mortality in the NICU population.
CLABSI Rate per 1000 Central Line Days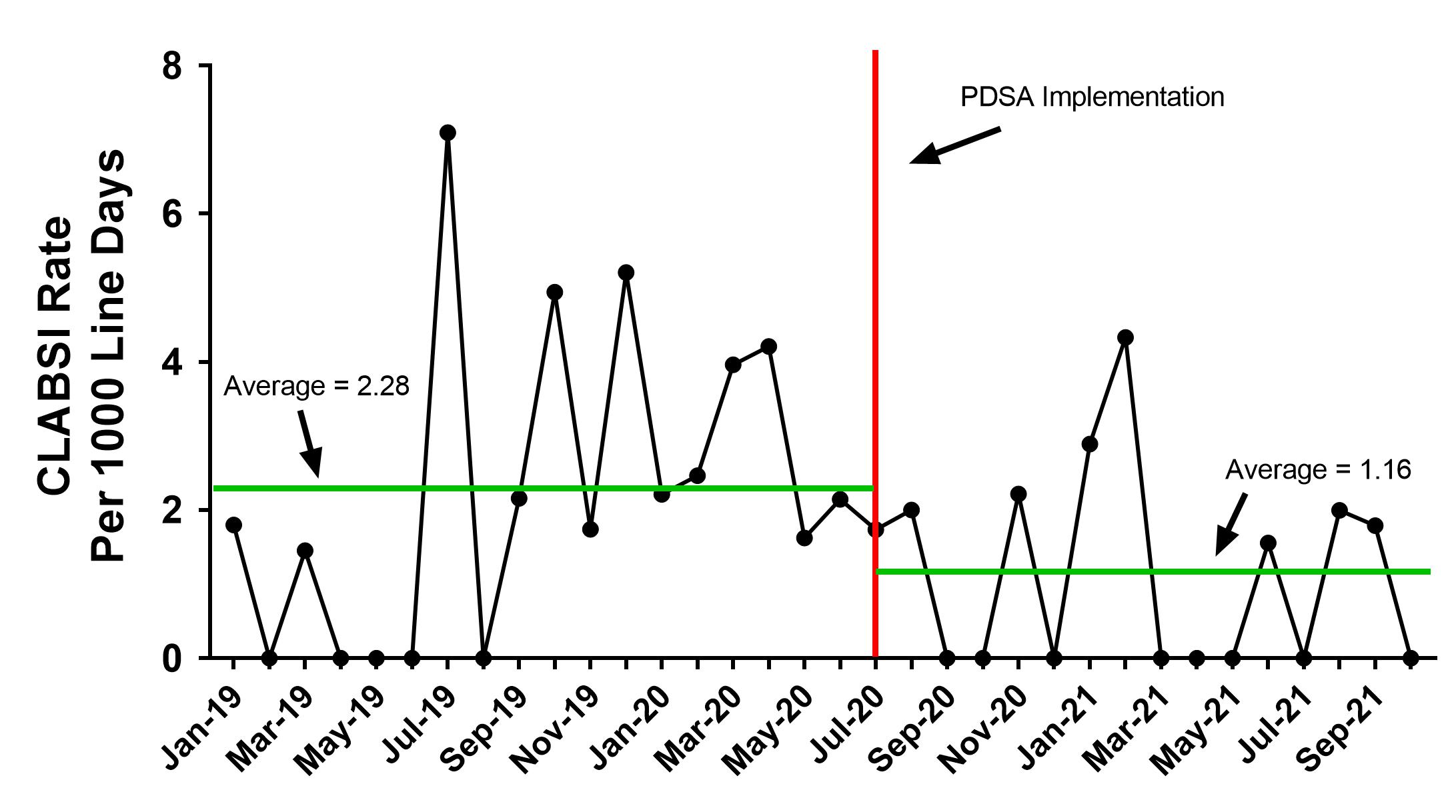 CLABSI rates per 1000 line days pre- and post- PDSA implementation showing a clinically evident decrease in CLABSI rate.
CLABSI rates per 1000 line days pre- and post- PDSA implementation showing a clinically evident decrease in CLABSI rate.
CLABSI Incidence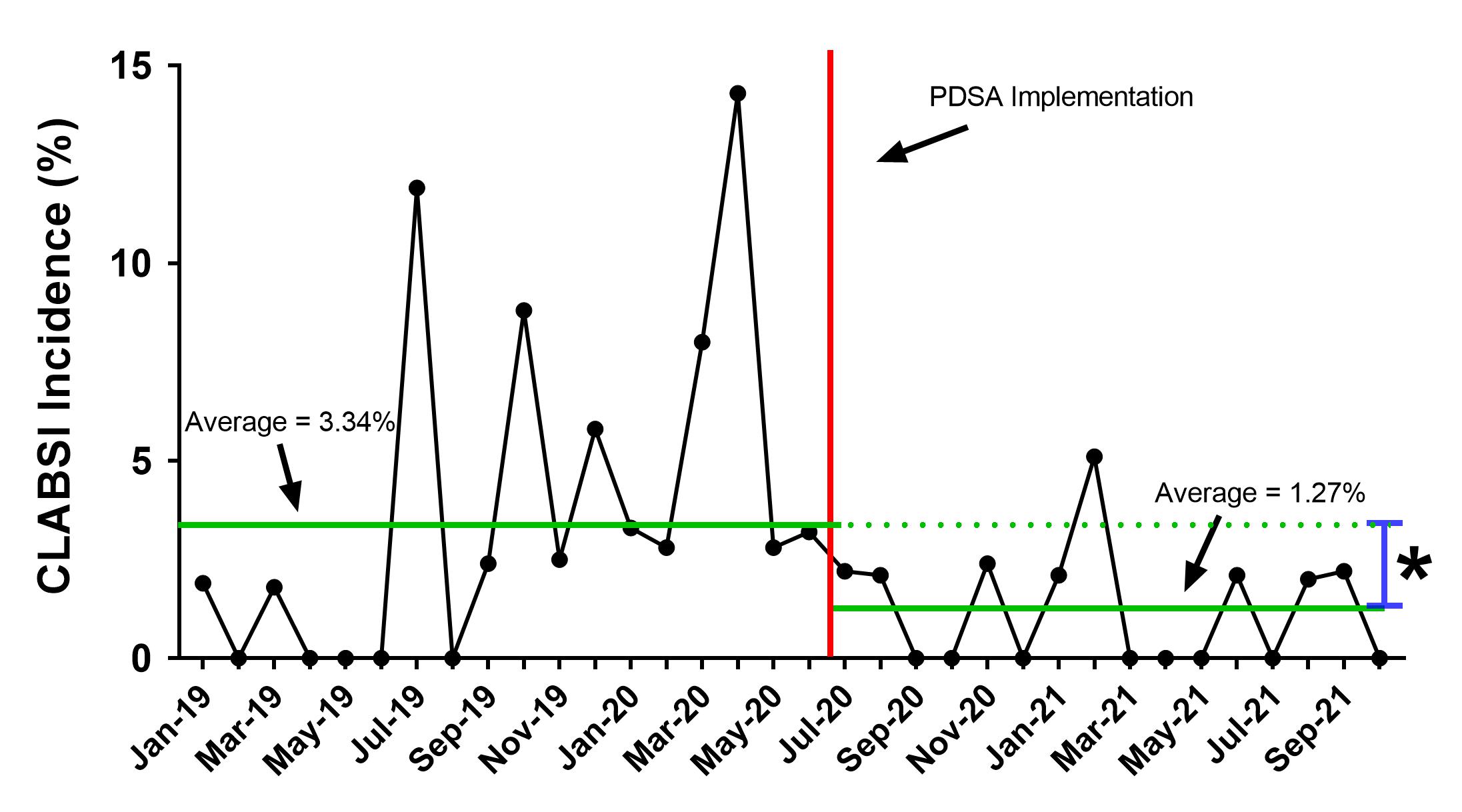 CLABSI incidence pre- and post- PDSA implementation showing a statistically significant decrease in CLABSI rates.
CLABSI incidence pre- and post- PDSA implementation showing a statistically significant decrease in CLABSI rates.
Objective: To evaluate the efficacy of process mapping methodologies including CurosTM Caps, venous access device (VAD) algorithms, clean space recommendations and provider educational tools on prevention of neonatal CLABSI through analysis of central line days (CLDs) and overall unit infection rates.
Design/Methods: A multidisciplinary team (advanced practice nursing leaders, nurses, MDs, APPs, QI consultant, and medical students) was assembled to analyze CLABSI incidence and risk factors, brainstorm interventions, and audit results following implementation of PDSAs. Study population included all infants in the UMMCH NICU over a 3 year period (2019-2021) with CLABSI defined per NHSN criteria. Retrospective review of CLABSI rate per 1000 CLDs and overall unit infection rates (CLABSI cases ÷ number of central lines removed), was performed for 18 months prior to PDSA intervention and 16 months following the start of PDSA testing rollout. Pre- and post- PDSA CLABSI results were compared using two sample t-test and chi square to determine statistical significance.
Results: The incidence of CLABSI before PDSA implementation (January 2019 - June 2020) and after PDSA implementation (July 2020 - October 2021) were 3.34% (n = 23/689) and 1.27% (n = 9/706), respectively with statistical significance via chi-square test (p = 0.01). CLABSI rates per 1000 CLDs before PDSA implementation and after PDSA implementation were 2.28 and 1.16, respectively, a 49% decrease in CLABSI rate per 1,000 CLDs. A two sample t-test of CLABSI rates per 1,000 CLDs revealed no statistical significance post-PDSA (p-value 0.10, 95% CI: [-2.33,0.92]) compared to pre-PDSA.Conclusion(s): PDSA interventions produced a statistically significant decrease in CLABSI incidence. PDSA implementation resulted in a clinically evident decrease in CLABSI rates per 1,000 CLDs in the UMMCH NICU, though not statistically significant. Continued quality improvement efforts are aimed at further decreasing risk factors including the time that central lines are in place, decreasing the frequency of line access, and improving the sterility of central lines. These efforts are required to continue improvement of CLABSI rates and decrease morbidity and mortality in the NICU population.
CLABSI Rate per 1000 Central Line Days
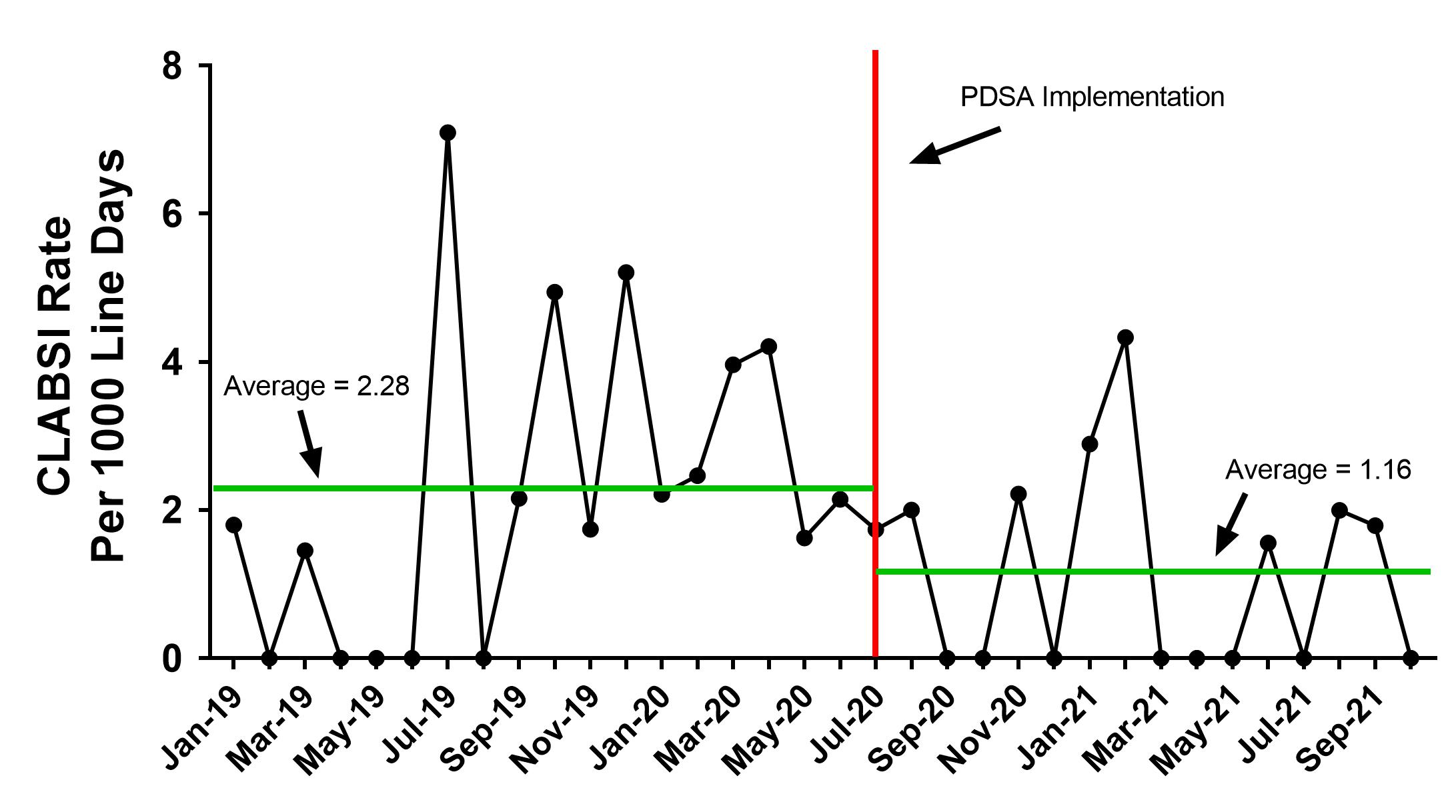 CLABSI rates per 1000 line days pre- and post- PDSA implementation showing a clinically evident decrease in CLABSI rate.
CLABSI rates per 1000 line days pre- and post- PDSA implementation showing a clinically evident decrease in CLABSI rate.CLABSI Incidence
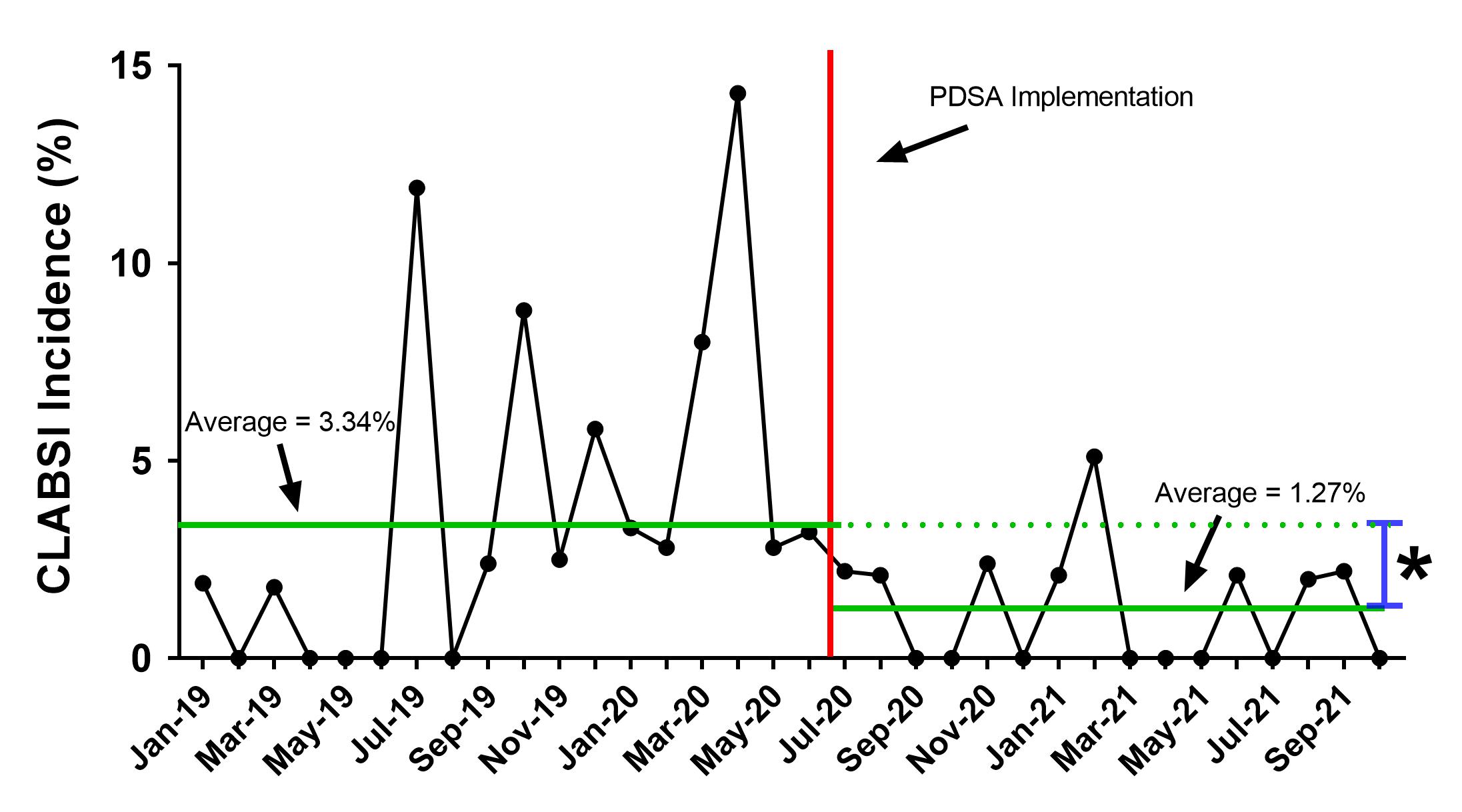 CLABSI incidence pre- and post- PDSA implementation showing a statistically significant decrease in CLABSI rates.
CLABSI incidence pre- and post- PDSA implementation showing a statistically significant decrease in CLABSI rates.