Neonatal Pulmonology
Category: Abstract Submission
Neonatal Pulmonology V: Preclinical studies and Clinical Care Issues
480 - Quantitative Magnetic Resonance Imaging (MRI) of the Lung in Infants in the Neonatal Intensive Care Unit (NICU)
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 480
Publication Number: 480.433
Publication Number: 480.433
Lauren Blatt, Weill Cornell Medicine, New York, NY, United States; Jonathan P. Dyke, Weill Cornell Medicine, New York, NY, United States; Arzu Kovanlikaya, Weill Cornell Medicine, New york, NY, United States; Andreas Voskrebenzev, Medical School Hanover, Hannover, Niedersachsen, Germany; Jeffrey Perlman, Weill Cornell Medicine, New York City, NY, United States

Lauren Blatt, MD (she/her/hers)
Assistant Professor of Pediatrics
Weill Cornell Medicine
New York, New York, United States
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) is a common morbidity of preterm birth, affecting approximately 50% of infants born at < 29 weeks gestation. The evolving definition of BPD has largely consisted of the degree of respiratory support and oxygen requirement in preterm infants with no true quantitative measure. New MRI techniques have allowed for the ability to quantitatively assess the lung in infants.
Objective: To evaluate quantitative MR measures of lung function in infants with and without BPD.
Design/Methods: Infants admitted to the NICU and scheduled for a clinically indicated brain MRI were enrolled with Institutional Review Board approval. Parents provided written consent for their infant to undergo a 15-minute lung MRI following the brain MRI without sedation. Quantitative ventilation and perfusion maps were obtained using standard spoiled gradient echo sequence and phase resolved post-processing algorithm. Ventilation defect percentage (VDP) and perfusion defect percentage (QDP) were calculated from ventilation and perfusion maps. BPD was defined according to the 2018 National Institute of Health BPD executive workshop. The strength of associations was assessed using t-tests.
Results: 10 infants (9 preterm, 1 term) have been enrolled in the study to date. Median gestational age (GA) of the study population was 28 5/7 weeks (IQR 26-32 2/7) and median birth weight was 950 grams (IQR 653-1388). MRI was performed at a median corrected GA of 39 6/7 weeks (IQR 38 3/7-42). 5 of the 9 preterm infants had BPD (1 grade I, 3 grade II, and 1 grade III). Quantitative lung assessment was not performed on one preterm patient due to motion artifacts. Clinical characteristics and quantitative MR measures for included infants are shown in Table 1. The mean VDP was significantly higher in preterm infants with grade II/III BPD compared to term or preterm infants with none/grade I BPD (21.3% vs. 4.9%; p=0.009). No significant difference was seen in QDP between groups (4.0% vs. 5.6%; p=0.695). In preterm infants alone, the mean VDP was also significantly higher in preterm infants with grade II/III BPD compared to preterm infants with none/grade I BPD (21.3% vs. 5.4%; p=0.021). There was no significant difference in VDP between preterm infants discharged on home oxygen (n=3) compared to preterm infants discharged without oxygen (18.3% vs. 10.3%; p=0.347).Conclusion(s): VDP may be useful as an adjunctive, quantitative measure of lung function in infants with BPD. Future studies evaluating serial VDP measurements in infants at risk for BPD may be valuable in the characterizing BPD severity and guiding management.
Table 1. Clinical characteristics and quantitative MR measures of lung function for infants.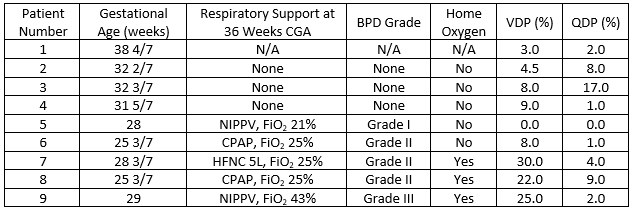 CGA = corrected gestational age, NIPPV = non-invasive positive pressure ventilation, HFNC = high flow nasal cannula, CPAP = continuous positive airway pressure, FiO2= fraction of inspired oxygen
CGA = corrected gestational age, NIPPV = non-invasive positive pressure ventilation, HFNC = high flow nasal cannula, CPAP = continuous positive airway pressure, FiO2= fraction of inspired oxygen
Objective: To evaluate quantitative MR measures of lung function in infants with and without BPD.
Design/Methods: Infants admitted to the NICU and scheduled for a clinically indicated brain MRI were enrolled with Institutional Review Board approval. Parents provided written consent for their infant to undergo a 15-minute lung MRI following the brain MRI without sedation. Quantitative ventilation and perfusion maps were obtained using standard spoiled gradient echo sequence and phase resolved post-processing algorithm. Ventilation defect percentage (VDP) and perfusion defect percentage (QDP) were calculated from ventilation and perfusion maps. BPD was defined according to the 2018 National Institute of Health BPD executive workshop. The strength of associations was assessed using t-tests.
Results: 10 infants (9 preterm, 1 term) have been enrolled in the study to date. Median gestational age (GA) of the study population was 28 5/7 weeks (IQR 26-32 2/7) and median birth weight was 950 grams (IQR 653-1388). MRI was performed at a median corrected GA of 39 6/7 weeks (IQR 38 3/7-42). 5 of the 9 preterm infants had BPD (1 grade I, 3 grade II, and 1 grade III). Quantitative lung assessment was not performed on one preterm patient due to motion artifacts. Clinical characteristics and quantitative MR measures for included infants are shown in Table 1. The mean VDP was significantly higher in preterm infants with grade II/III BPD compared to term or preterm infants with none/grade I BPD (21.3% vs. 4.9%; p=0.009). No significant difference was seen in QDP between groups (4.0% vs. 5.6%; p=0.695). In preterm infants alone, the mean VDP was also significantly higher in preterm infants with grade II/III BPD compared to preterm infants with none/grade I BPD (21.3% vs. 5.4%; p=0.021). There was no significant difference in VDP between preterm infants discharged on home oxygen (n=3) compared to preterm infants discharged without oxygen (18.3% vs. 10.3%; p=0.347).Conclusion(s): VDP may be useful as an adjunctive, quantitative measure of lung function in infants with BPD. Future studies evaluating serial VDP measurements in infants at risk for BPD may be valuable in the characterizing BPD severity and guiding management.
Table 1. Clinical characteristics and quantitative MR measures of lung function for infants.
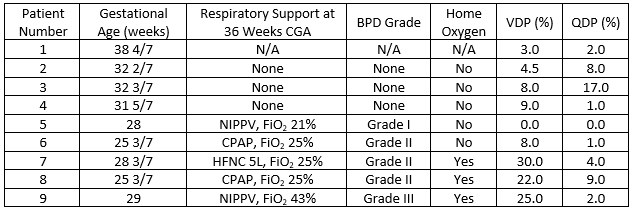 CGA = corrected gestational age, NIPPV = non-invasive positive pressure ventilation, HFNC = high flow nasal cannula, CPAP = continuous positive airway pressure, FiO2= fraction of inspired oxygen
CGA = corrected gestational age, NIPPV = non-invasive positive pressure ventilation, HFNC = high flow nasal cannula, CPAP = continuous positive airway pressure, FiO2= fraction of inspired oxygen