Medical Education: Resident
Category: Abstract Submission
Medical Education 14 - Medical Education: Resident V
281 - Resident driven research program: multiyear impact assessment
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 281
Publication Number: 281.420
Publication Number: 281.420
Adeline T. Yang, University of Texas Southwestern Medical School, Dallas, TX, United States; Pamela J. Okada, University of Texas Southwestern Medical School, Dallas, TX, United States; Mackenzie S. Frost, Childrens Hospital of Philadelphia, Ardmore, PA, United States

Adeline T. Yang, MD
Chief Resident
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Scholarship in residency is an ACGME requirement and AAP Committee on Pediatric Research recommendation, yet barriers persist. Previous work demonstrated our residents and faculty had specific areas of need that, when addressed, could lower the barrier to resident scholarship. There remains substantial opportunity for improvement in pediatric resident research programs and scholarly productivity.
Objective: Analyses from internal studies drove the design of interventions around 1) centralizing resources digitally, 2) curating databases of prior resident works and available faculty projects, 3) establishing research project milestones, 4) creating standardized forms for faculty feedback on resident research proposals, and 5) designing an experiential research curriculum with courses starting at intern orientation (Fig. 1 and 2). We aimed to improve the resident research experience, with additional goals of increasing scholarly quality and productivity.
Design/Methods: Annual voluntary resident surveys were collected electronically. Residents rated tasks on a three-point scale, from “hard” 3 points to “easy” 1 point. Interventions were prioritized based on feedback. The first interventions began in 2020. Additional surveys were sent before and after specific interventions such as workshops and resident-led lectures.
Results: From academic year 2019 through 2022, 195 resident responses were obtained. In 2020 residents reported a 3-6% increase in coordination time - attributable to both preparatory work and the COVID-19 pandemic (Fig. 3). Positive gains were seen in finding points of contact, with a 29% improvement in residents’ perception of this task; residents also reported greater ease finding: mentors (22% improvement), research resources (20%), projects (18%), funding (16%), and clinical faculty with protected research time (12%); as well as gaining face time with mentors (19% improvement), completing pre-research training (17%), and knowing faculty expectations (11%).Conclusion(s): A multifaceted approach providing both scheduled, experiential learning opportunities as well as resources to explore at an individual’s convenience had a positive effect on residents’ perception of scholarly work at our institution within a relatively short time. While this comes at the expense of additional pre-research work (credentialing, proposals, scheduling, workshops), the increased preparedness has led to improvements in finding and working with the right mentors / projects and setting expectations. We hope this will ultimately translate to improved scholarship for both our residents and the academic community.
Figure 3:.png) Average scores of residents’ perceptions of conducting research at our institution over time. Tasks rated as “Easy” scored 1.00 and are at the green bullseye; tasks rated as “hard” scored a 3.00 and are at the red perimeter. The yellow line represents the most recent data from academic year 2021-22. CMC: Children's Medical Center. IRB: Institutional Review Board
Average scores of residents’ perceptions of conducting research at our institution over time. Tasks rated as “Easy” scored 1.00 and are at the green bullseye; tasks rated as “hard” scored a 3.00 and are at the red perimeter. The yellow line represents the most recent data from academic year 2021-22. CMC: Children's Medical Center. IRB: Institutional Review Board
Figure 1: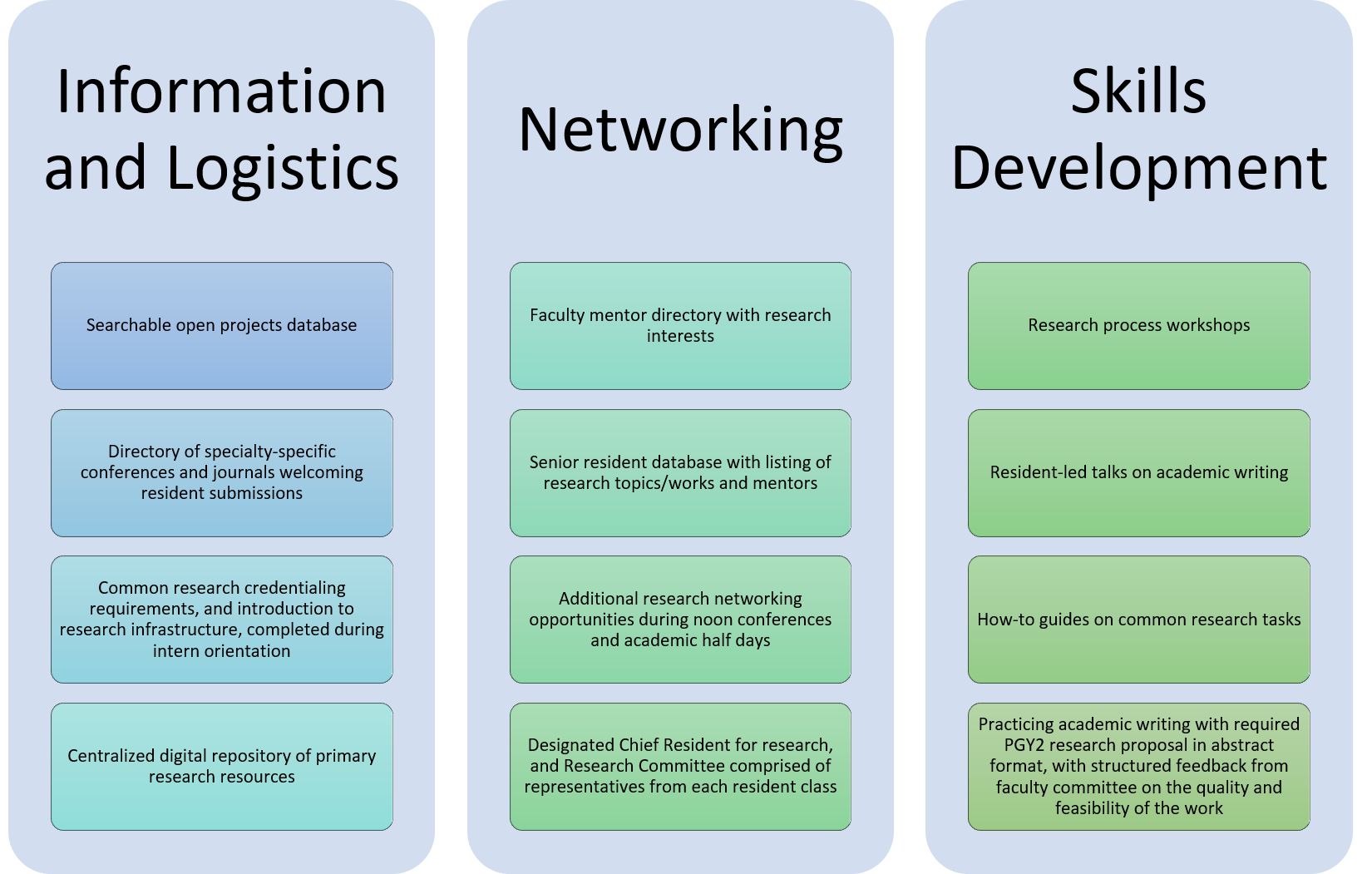 Main types of interventions targeting improvement of the resident research experience, as well as scholarly quality and productivity. PGY2 = postgraduate year two, or second year of residency.
Main types of interventions targeting improvement of the resident research experience, as well as scholarly quality and productivity. PGY2 = postgraduate year two, or second year of residency.
Objective: Analyses from internal studies drove the design of interventions around 1) centralizing resources digitally, 2) curating databases of prior resident works and available faculty projects, 3) establishing research project milestones, 4) creating standardized forms for faculty feedback on resident research proposals, and 5) designing an experiential research curriculum with courses starting at intern orientation (Fig. 1 and 2). We aimed to improve the resident research experience, with additional goals of increasing scholarly quality and productivity.
Design/Methods: Annual voluntary resident surveys were collected electronically. Residents rated tasks on a three-point scale, from “hard” 3 points to “easy” 1 point. Interventions were prioritized based on feedback. The first interventions began in 2020. Additional surveys were sent before and after specific interventions such as workshops and resident-led lectures.
Results: From academic year 2019 through 2022, 195 resident responses were obtained. In 2020 residents reported a 3-6% increase in coordination time - attributable to both preparatory work and the COVID-19 pandemic (Fig. 3). Positive gains were seen in finding points of contact, with a 29% improvement in residents’ perception of this task; residents also reported greater ease finding: mentors (22% improvement), research resources (20%), projects (18%), funding (16%), and clinical faculty with protected research time (12%); as well as gaining face time with mentors (19% improvement), completing pre-research training (17%), and knowing faculty expectations (11%).Conclusion(s): A multifaceted approach providing both scheduled, experiential learning opportunities as well as resources to explore at an individual’s convenience had a positive effect on residents’ perception of scholarly work at our institution within a relatively short time. While this comes at the expense of additional pre-research work (credentialing, proposals, scheduling, workshops), the increased preparedness has led to improvements in finding and working with the right mentors / projects and setting expectations. We hope this will ultimately translate to improved scholarship for both our residents and the academic community.
Figure 3:
.png) Average scores of residents’ perceptions of conducting research at our institution over time. Tasks rated as “Easy” scored 1.00 and are at the green bullseye; tasks rated as “hard” scored a 3.00 and are at the red perimeter. The yellow line represents the most recent data from academic year 2021-22. CMC: Children's Medical Center. IRB: Institutional Review Board
Average scores of residents’ perceptions of conducting research at our institution over time. Tasks rated as “Easy” scored 1.00 and are at the green bullseye; tasks rated as “hard” scored a 3.00 and are at the red perimeter. The yellow line represents the most recent data from academic year 2021-22. CMC: Children's Medical Center. IRB: Institutional Review BoardFigure 1:
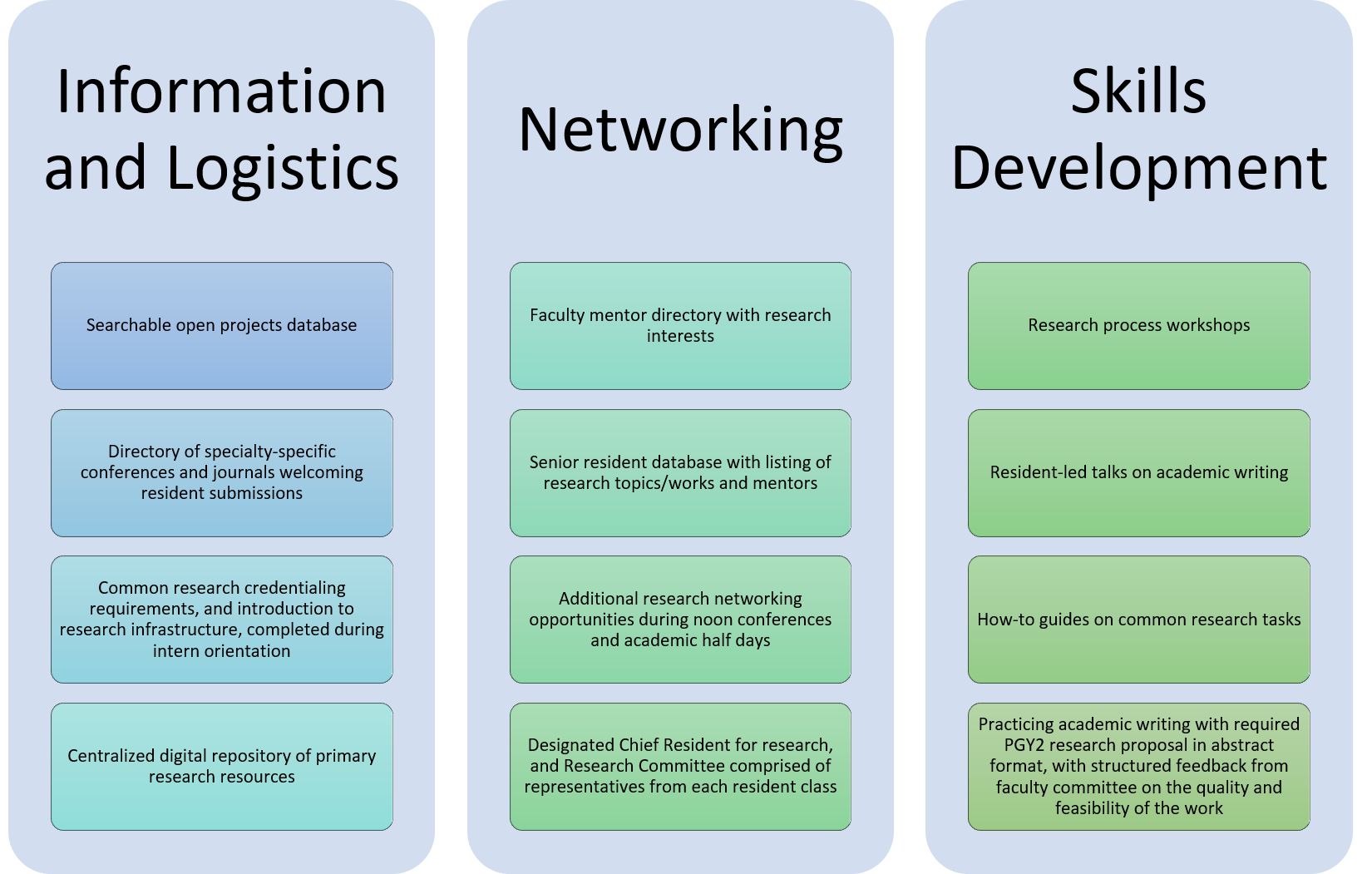 Main types of interventions targeting improvement of the resident research experience, as well as scholarly quality and productivity. PGY2 = postgraduate year two, or second year of residency.
Main types of interventions targeting improvement of the resident research experience, as well as scholarly quality and productivity. PGY2 = postgraduate year two, or second year of residency.