Hospital Medicine: Newborn Care
Category: Abstract Submission
Hospital Medicine: Clinical - Bronchiolitis/HFNC and Newborn Care
130 - Resource Use and Outcomes of Newborns with Neonatal Abstinence Syndrome with Concomitant Cannabis Exposure
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 130
Publication Number: 130.415
Publication Number: 130.415
Cecilia Ampem-Darko, Tema General Hospital, Ithaca, NY, United States; Ernestina H. Bioh, Ghana Health Service- Western Region, Oakland, CA, United States; RUTH E. TURKSON, Unaffiliated, Lowell, MA, United States; Harshit Doshi, Pediatrix Medical Group of FL, Venice, FL, United States; Narendrasinh Parmar, East Tennessee Children's Hospital, Knoxville, TN, United States; Rhythm Vasudeva, University of Kansas School of Medicine, Wichita, KS, United States; Jacob H. Umscheid, University of Kansas School of Medicine, Wichita, KS, United States; Sahithi Pemmasani, Icahn School of Medicine at Mount Sinai, Elmhurst, NY, United States; Tarang Parekh, George Mason University, Elmhurst, NY, United States; Parth J. Bhatt, United Hospital Center, Bridgeport, WV, United States; Keyur Donda, University of South Florida, Tampa, FL, United States; FREDRICK Dapaah-Siakwan, Valley Children's Hospital, Madera, CA, United States

Cecilia Ampem-Darko, MBChB
n/a
Tema General Hospital
Ithaca, New York, United States
Presenting Author(s)
Background: The use of opioids and cannabis in pregnancy is increasing in the United States (US) in tandem with Neonatal abstinence syndrome (NAS). While the outcomes and resource use for NAS have been extensively studied, population-based estimates of the outcomes and resource use for NAS with concomitant cannabis exposure (NAS-C) are lacking.
Objective: To determine the resource use and outcomes of NAS with concomitant cannabis exposure in the US.
Design/Methods: We performed cross-sectional analysis of newborn hospitalizations with NAS in the 2016 Kids Inpatient Database. International Classification of Diseases (ICD-10) diagnostic code (P96.1) was used to identify NAS hospitalizations. NAS hospitalizations with concomitant cannabis exposure were further identified with ICD-10 code P04.81. Transfers were excluded to avoid double counting. NAS and NAS with cannabis exposure were compared in terms of the following outcomes: prematurity, low birth weight, intrauterine growth restriction, feeding problems, seizures, and resource use. Resource use was defined by length of stay (LOS) and inflation-adjusted hospital cost. Prolonged LOS was defined as LOS >6 days. Categorical and continuous variables were compared using Chi-square test and Wilcoxon rank sum test, respectively. P-value < 0.05 was considered significant.
Results: Among 3.56 million newborn hospitalizations in 2019, 22,202 were diagnosed with NAS (6.2 per 1,000). Of those with NAS, 777 (3.5%) had concomitant cannabis exposure (NAS-C). There were no significant differences between newborns with NAS and NAS-C in terms of sex, racial distribution, insurance status, hospital characteristics, and geographic region (Table 1). When compared to NAS, those with NAS-C were more likely to be preterm (21.1 vs 18.4%; P=0.045), of low birth weight (21.3 vs 15.4%; P< 0.001), growth restricted (29.2 vs 26.4%; P< 0.001), and more likely to have feeding problems (30.4 vs 23.9%; P< 0.001) [Table 2]. The proportion with respiratory complications and seizures was not significantly different between the two groups. The median LOS and the proportion with LOS >6 days were similar between the two groups. The median cost of hospitalization was also not significantly different between the two groups. Conclusion(s): Neonatal hospitalizations NAS-C were more likely to have unfavorable birth outcomes such as preterm birth, low birth weight, intra-uterine growth restriction, and feeding complications compared to those with NAS. Resource use did not vary significantly between these groups. These findings underscore the need to screen and intervene for cannabis among pregnant women.
Table 1: Comparison of the demographic and hospital characteristics of NAS hospitalizations with and without concomitant cannabis exposure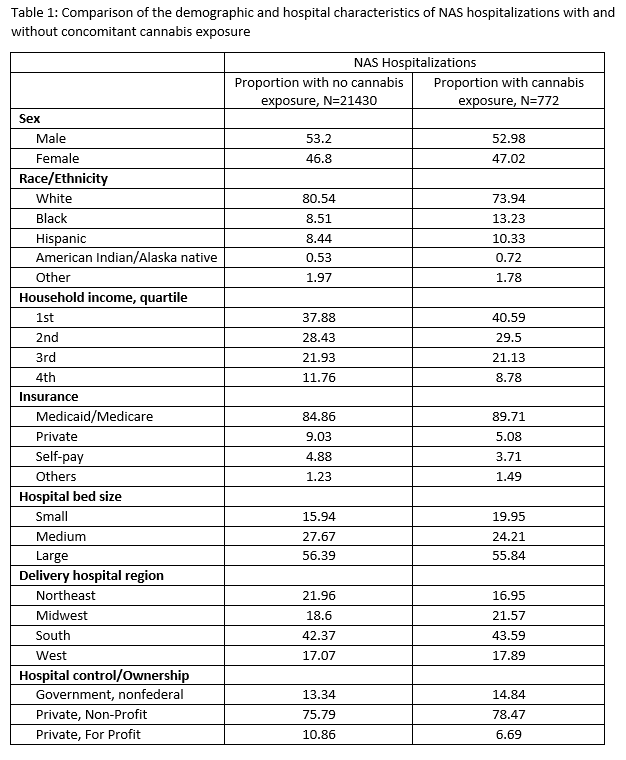
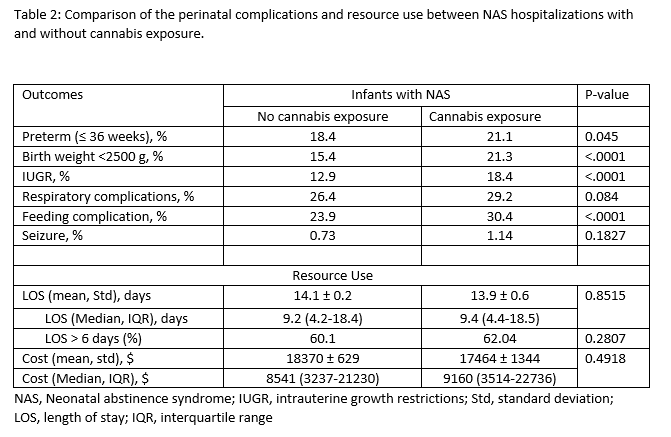
Table 2: Comparison of the perinatal complications and resource use between NAS hospitalizations with and without cannabis exposure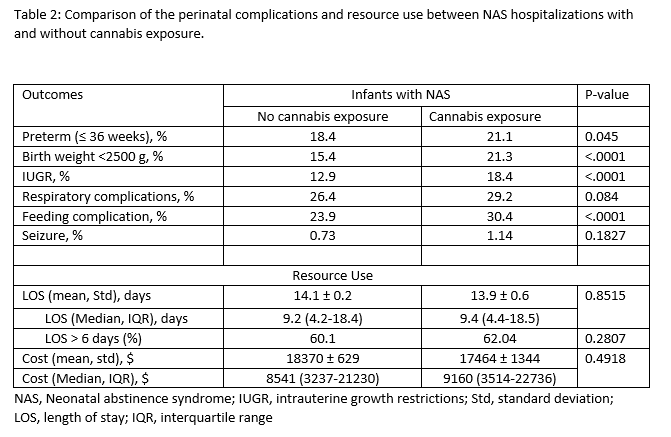
Objective: To determine the resource use and outcomes of NAS with concomitant cannabis exposure in the US.
Design/Methods: We performed cross-sectional analysis of newborn hospitalizations with NAS in the 2016 Kids Inpatient Database. International Classification of Diseases (ICD-10) diagnostic code (P96.1) was used to identify NAS hospitalizations. NAS hospitalizations with concomitant cannabis exposure were further identified with ICD-10 code P04.81. Transfers were excluded to avoid double counting. NAS and NAS with cannabis exposure were compared in terms of the following outcomes: prematurity, low birth weight, intrauterine growth restriction, feeding problems, seizures, and resource use. Resource use was defined by length of stay (LOS) and inflation-adjusted hospital cost. Prolonged LOS was defined as LOS >6 days. Categorical and continuous variables were compared using Chi-square test and Wilcoxon rank sum test, respectively. P-value < 0.05 was considered significant.
Results: Among 3.56 million newborn hospitalizations in 2019, 22,202 were diagnosed with NAS (6.2 per 1,000). Of those with NAS, 777 (3.5%) had concomitant cannabis exposure (NAS-C). There were no significant differences between newborns with NAS and NAS-C in terms of sex, racial distribution, insurance status, hospital characteristics, and geographic region (Table 1). When compared to NAS, those with NAS-C were more likely to be preterm (21.1 vs 18.4%; P=0.045), of low birth weight (21.3 vs 15.4%; P< 0.001), growth restricted (29.2 vs 26.4%; P< 0.001), and more likely to have feeding problems (30.4 vs 23.9%; P< 0.001) [Table 2]. The proportion with respiratory complications and seizures was not significantly different between the two groups. The median LOS and the proportion with LOS >6 days were similar between the two groups. The median cost of hospitalization was also not significantly different between the two groups. Conclusion(s): Neonatal hospitalizations NAS-C were more likely to have unfavorable birth outcomes such as preterm birth, low birth weight, intra-uterine growth restriction, and feeding complications compared to those with NAS. Resource use did not vary significantly between these groups. These findings underscore the need to screen and intervene for cannabis among pregnant women.
Table 1: Comparison of the demographic and hospital characteristics of NAS hospitalizations with and without concomitant cannabis exposure
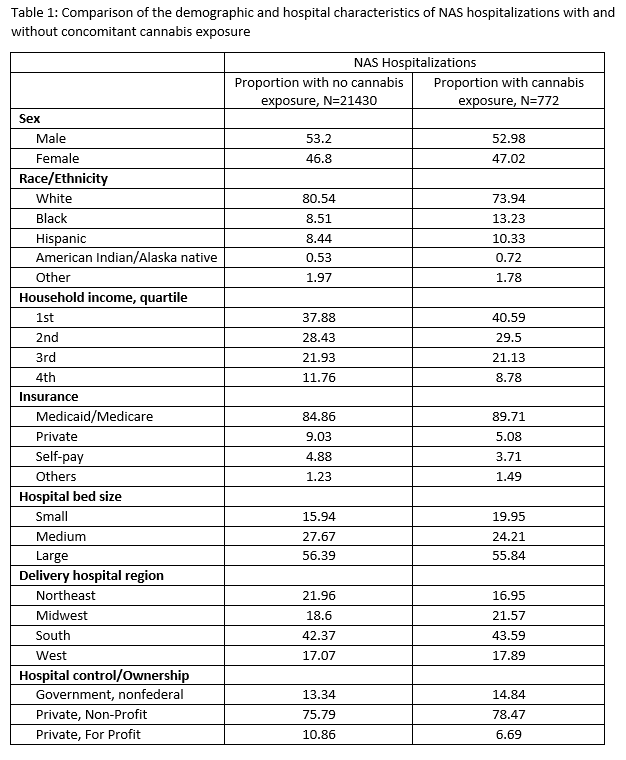
Table 2: Comparison of the perinatal complications and resource use between NAS hospitalizations with and without cannabis exposure