Neonatal Pulmonology
Category: Abstract Submission
Neonatal Pulmonology III: Molecular Markers and Clinical Prediction Models/Outcomes
455 - Respiratory Patient-Reported Outcomes Correlate with 1-Year Healthcare Utilization for Infants with Bronchopulmonary Dysplasia
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 455
Publication Number: 455.431
Publication Number: 455.431
William J. Scott, Medical College of Wisconsin, Wauwatosa, WI, United States; Kathryn E. Berlin, Medical College of Wisconsin Affiliated Hospitals, MILWAUKEE, WI, United States; Sara Dawson, Medical College of Wisconsin, Milwaukee, WI, United States; Joanne M. Lagatta, Medical College of Wisconsin, Milwaukee, WI, United States

William J. Scott, MD
Pediatric Resident
Medical College of Wisconsin
Wauwatosa, Wisconsin, United States
Presenting Author(s)
Background: There is a paucity of information about using parent-proxy patient-reported outcomes (PROs) to understand respiratory symptoms of infants with bronchopulmonary dysplasia (BPD) after neonatal intensive care unit (NICU) discharge (DC). Clinical studies of preterm infants have reported 1-year respiratory PROs; however, these questions were developed for pediatric asthma and have not been validated in infants with BPD.
Objective: To determine if 1-year respiratory PROs in infants with BPD correlated with NICU illness factors and post-DC respiratory healthcare utilization.
Design/Methods: A Prospective observational single-center cohort of preterm infants born < 32 weeks gestational age with BPD and their parents. Infants with congenital anomalies, tracheostomy, or surgical comorbidities were excluded. NICU illness factors and healthcare utilization were collected via chart review; parent questionnaires of demographics and PROs were completed by phone or electronically. Respiratory PROs at 1 year included 4 questions about physician-diagnosed wheezing or asthma, trouble breathing, trouble sleeping due to breathing, and use of extra respiratory medications. PROs were compared to NICU illness factors and 1-year respiratory healthcare utilization including respiratory readmissions, emergency room visits, home oxygen through 1 year, or use of systemic corticosteroids. Multivariable logistic regression adjusted the association between PROs and respiratory healthcare utilization for significant NICU illness factors.
Results: Of 145 parent-infant dyads, respiratory PROs were completed for 111 infants (77%). Respiratory symptoms at 1 year were reported by 38 (34%); 1-year respiratory healthcare utilization was reported by 47 (42%). PROs were associated with NICU illness factors, including lower birthweight, postnatal systemic steroid use, and corrected gestational age (CGA) at DC (Table 1). PROs were also associated with 1-year respiratory healthcare utilization, before and after adjusting for NICU illness factors (Table 2). Of note, 11 (29%) of those parents reporting respiratory symptoms had no acute respiratory healthcare utilization.Conclusion(s): Respiratory PROs in infants with BPD correlate with 1-year healthcare utilization, which suggests that these questions may be useful targets for further validation to improve outpatient follow-up of infants with BPD. Further work is needed to understand respiratory symptoms in patients not presenting for acute healthcare utilization.
Table 1. NICU illness factors associated with respiratory PROs.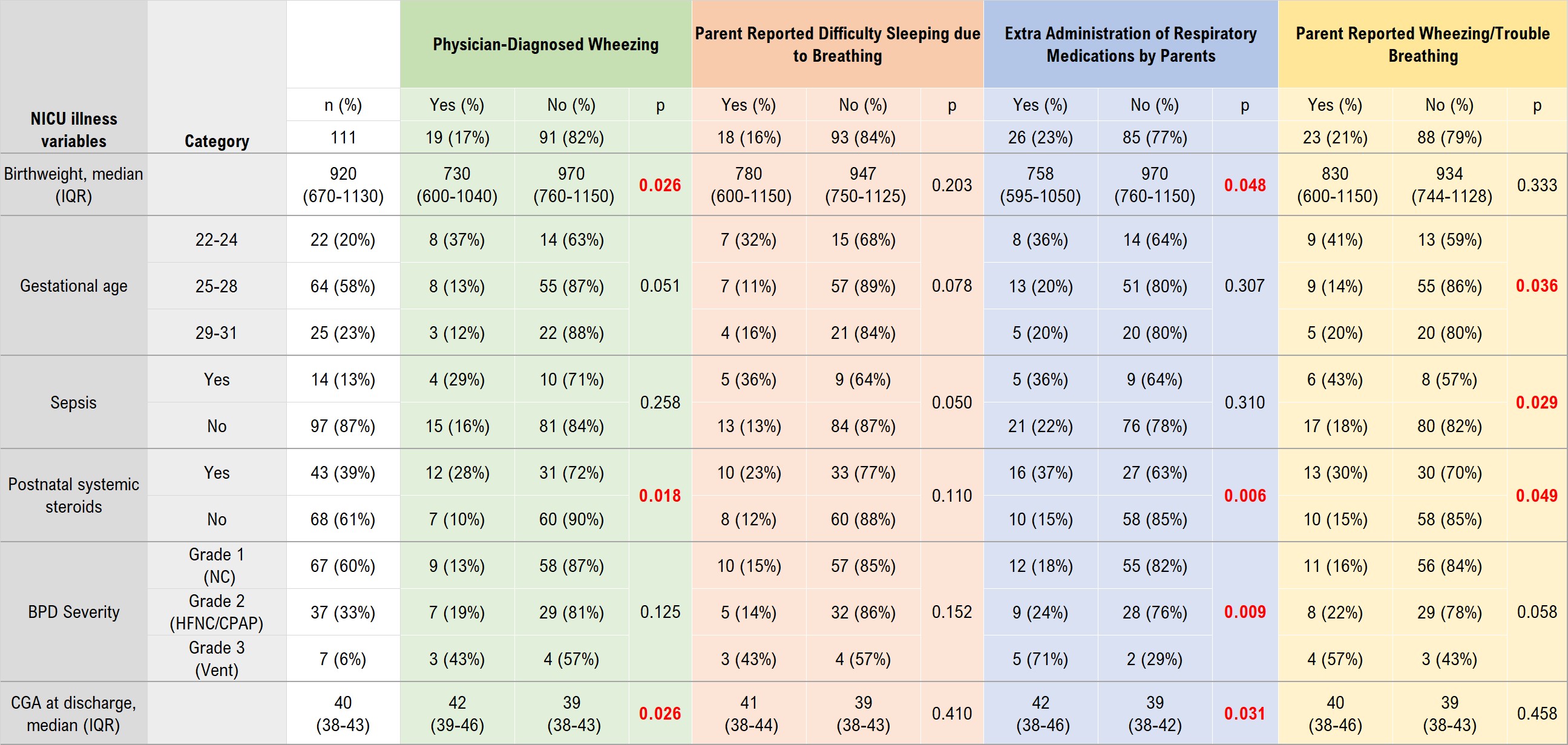 Questions adapted from the Tucson Respiratory Children’s Study and the Test of Respiratory Asthma Control in Kids. P-values are calculated by Kruskal-Wallis for tests of medians, or chi-squared or Fisher’s exact for tests of proportions. Red p-values highlight p < 0.05.
Questions adapted from the Tucson Respiratory Children’s Study and the Test of Respiratory Asthma Control in Kids. P-values are calculated by Kruskal-Wallis for tests of medians, or chi-squared or Fisher’s exact for tests of proportions. Red p-values highlight p < 0.05.
Table 2. Respiratory PROs associated with 1-year respiratory healthcare utilization.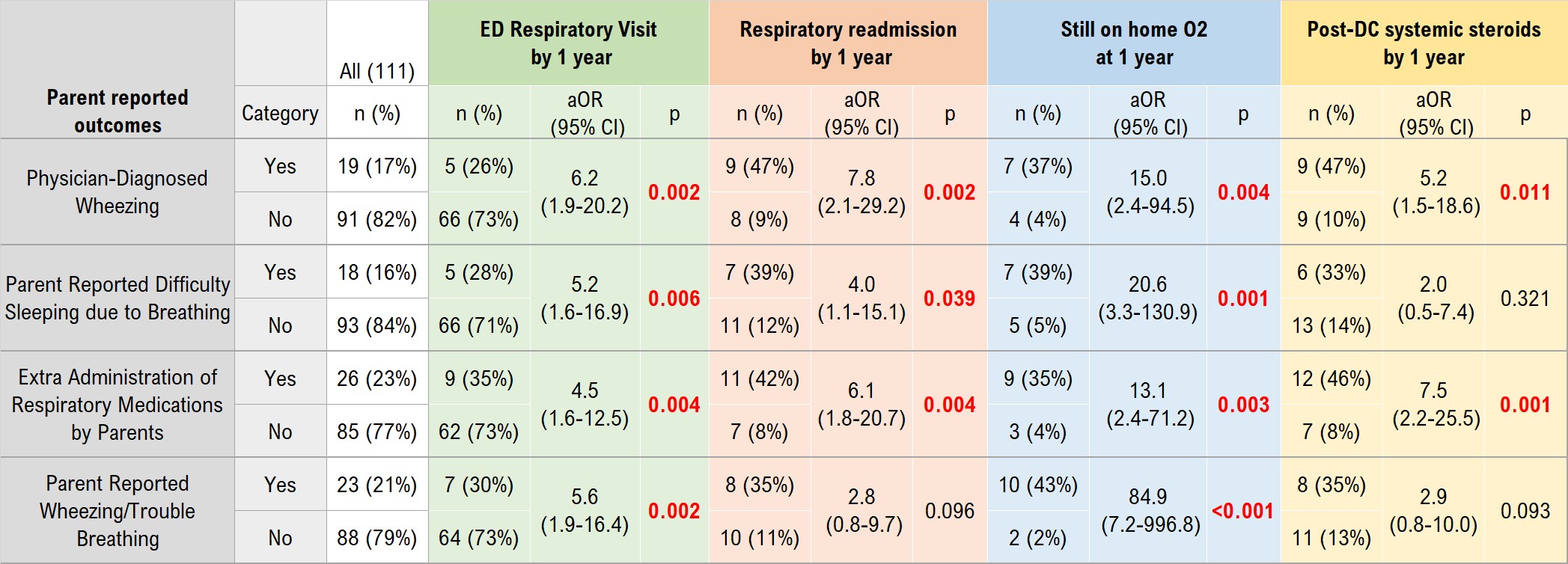 Adjusted OR (aOR) indicates the odds ratio for each 1-year respiratory outcome for infants whose parents respond “yes” within the past month to each question, compared to infants of parents responding “no”, adjusted for significant NICU illness factors including birth weight, sepsis, BPD severity, postnatal systemic steroids, and corrected gestational age at NICU discharge.
Adjusted OR (aOR) indicates the odds ratio for each 1-year respiratory outcome for infants whose parents respond “yes” within the past month to each question, compared to infants of parents responding “no”, adjusted for significant NICU illness factors including birth weight, sepsis, BPD severity, postnatal systemic steroids, and corrected gestational age at NICU discharge.
Objective: To determine if 1-year respiratory PROs in infants with BPD correlated with NICU illness factors and post-DC respiratory healthcare utilization.
Design/Methods: A Prospective observational single-center cohort of preterm infants born < 32 weeks gestational age with BPD and their parents. Infants with congenital anomalies, tracheostomy, or surgical comorbidities were excluded. NICU illness factors and healthcare utilization were collected via chart review; parent questionnaires of demographics and PROs were completed by phone or electronically. Respiratory PROs at 1 year included 4 questions about physician-diagnosed wheezing or asthma, trouble breathing, trouble sleeping due to breathing, and use of extra respiratory medications. PROs were compared to NICU illness factors and 1-year respiratory healthcare utilization including respiratory readmissions, emergency room visits, home oxygen through 1 year, or use of systemic corticosteroids. Multivariable logistic regression adjusted the association between PROs and respiratory healthcare utilization for significant NICU illness factors.
Results: Of 145 parent-infant dyads, respiratory PROs were completed for 111 infants (77%). Respiratory symptoms at 1 year were reported by 38 (34%); 1-year respiratory healthcare utilization was reported by 47 (42%). PROs were associated with NICU illness factors, including lower birthweight, postnatal systemic steroid use, and corrected gestational age (CGA) at DC (Table 1). PROs were also associated with 1-year respiratory healthcare utilization, before and after adjusting for NICU illness factors (Table 2). Of note, 11 (29%) of those parents reporting respiratory symptoms had no acute respiratory healthcare utilization.Conclusion(s): Respiratory PROs in infants with BPD correlate with 1-year healthcare utilization, which suggests that these questions may be useful targets for further validation to improve outpatient follow-up of infants with BPD. Further work is needed to understand respiratory symptoms in patients not presenting for acute healthcare utilization.
Table 1. NICU illness factors associated with respiratory PROs.
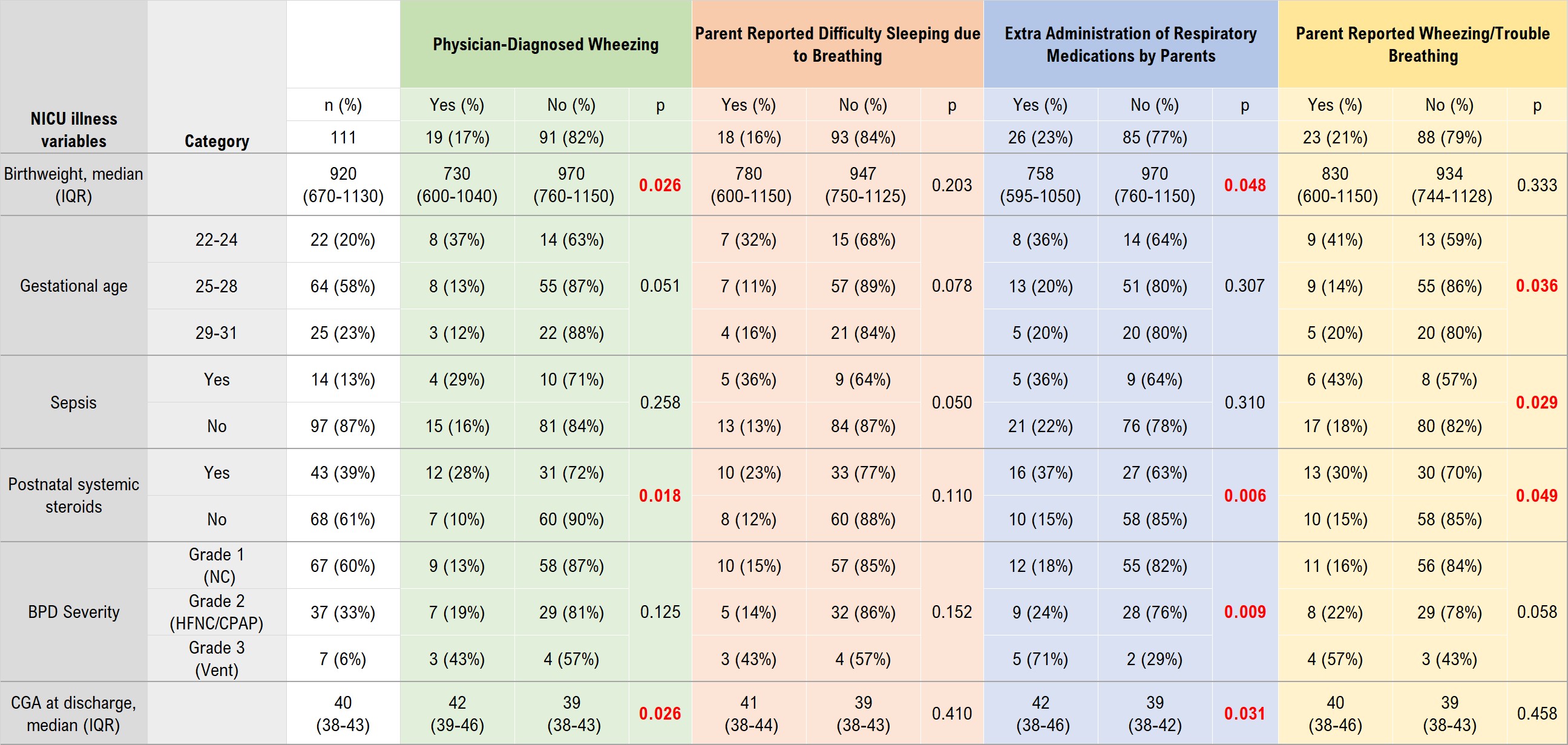 Questions adapted from the Tucson Respiratory Children’s Study and the Test of Respiratory Asthma Control in Kids. P-values are calculated by Kruskal-Wallis for tests of medians, or chi-squared or Fisher’s exact for tests of proportions. Red p-values highlight p < 0.05.
Questions adapted from the Tucson Respiratory Children’s Study and the Test of Respiratory Asthma Control in Kids. P-values are calculated by Kruskal-Wallis for tests of medians, or chi-squared or Fisher’s exact for tests of proportions. Red p-values highlight p < 0.05.Table 2. Respiratory PROs associated with 1-year respiratory healthcare utilization.
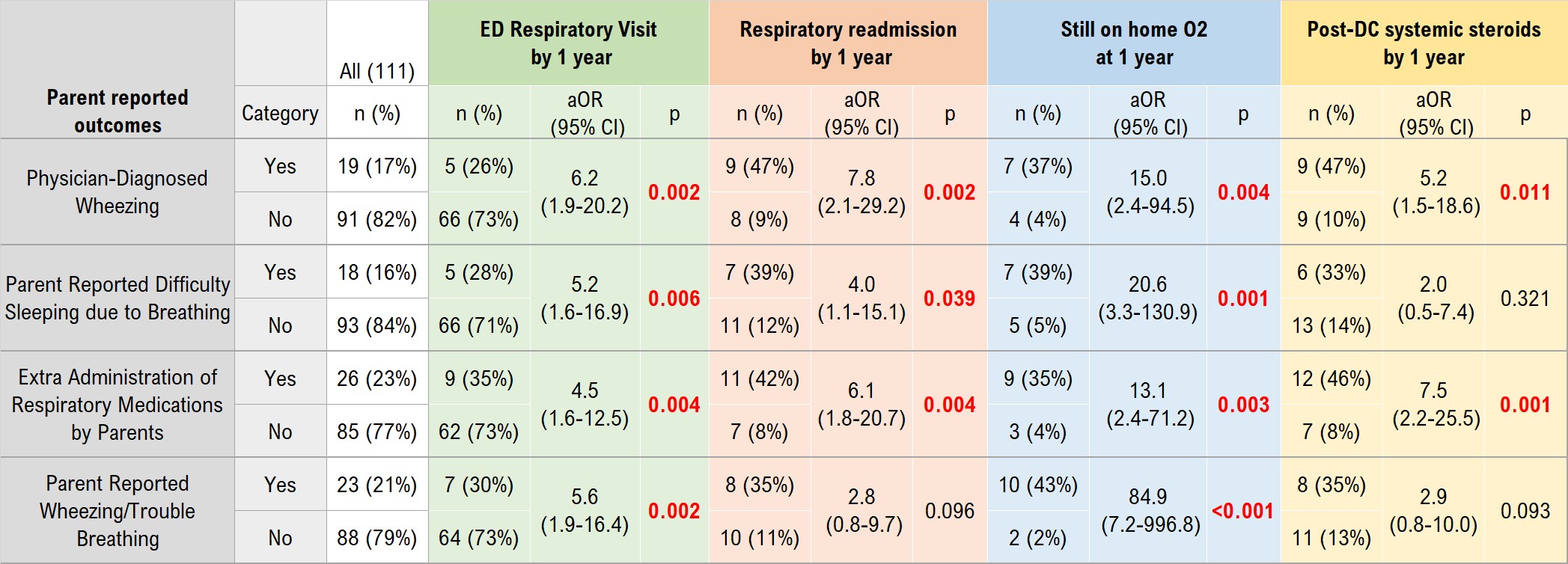 Adjusted OR (aOR) indicates the odds ratio for each 1-year respiratory outcome for infants whose parents respond “yes” within the past month to each question, compared to infants of parents responding “no”, adjusted for significant NICU illness factors including birth weight, sepsis, BPD severity, postnatal systemic steroids, and corrected gestational age at NICU discharge.
Adjusted OR (aOR) indicates the odds ratio for each 1-year respiratory outcome for infants whose parents respond “yes” within the past month to each question, compared to infants of parents responding “no”, adjusted for significant NICU illness factors including birth weight, sepsis, BPD severity, postnatal systemic steroids, and corrected gestational age at NICU discharge.