Back
Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement V
395 - Neonatal Intensive Care Unit – Family Involvement, Responsibility and Satisfaction Task (NICU-FIRST) – A Novel Quality Improvement Project
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 395
Publication Number: 395.435
Publication Number: 395.435
Venkata Raju, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Tara Lyngaas, Baylor Scott White McLane Children's Medical Center, Georgetown, TX, United States; Shelly D. Hill, Baylor Scott White McLane Children's Medical Center, Lorena, TX, United States; Martha Hemingway, Baylor Scott White McLane Children's Medical Center, Harker Heights, TX, United States; Erica Stone, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; raza Bajwa, Baylor Scott White McLane Children's Medical Center, round rock, TX, United States; Muppala Raju, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Niraj Vora, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Mahmoud Ali, MetroHealth Medical center/Case Western Reserve university, North olmsted, OH, United States; Katherine R. Jones, Baylor Scott & White Health, Hewitt, TX, United States
- VG
Vinayak P. Govande, MBBS MD MS MBA
Neonatologist
McLane CHildren's Hospital, Baylor Scott and White
Temple, Texas, United States
Presenting Author(s)
Background: Family involvement in the care of their infants in the Neonatal Intensive Care Unit (NICU) is crucial to improved patient outcomes. Families who receive clear, concise communication, experience attentive listening and respect, feel safe and prepared to assume the care of their child.
Objective: To identify opportunities and improve the family’s perception of their involvement, responsibility and satisfaction with the care provided to their infants. Success was recognized through an increased response return and improved satisfaction scores.
Design/Methods: NICU-FIRST, a multidisciplinary team, including a parent of NICU graduate, focused on the importance of family feedback related to the discharge process. An initiative was implemented titled the “CHAIR” project, “Communication in Hospital giving Attention, Information and Respect, which aligned with the goals set forth for the Press Ganey NICU Survey scores. The 51 bed NICU is an open unit allowing the team members to encourage providers to be seated in a chair while talking to the families. Monthly Operating Review (MOR) meetings were held with a formal partnership of administration, nurse and physician leaders. Interactions between the pediatric units and the NICU helped identify on-going issues, idea sharing, and standardizing expectations for the discharge process.
Results: Overall Press Ganey scores in the NICU saw a significant improvement. The “likelihood of recommending” question increased from a mean score of 91.67 (43rd percentile) to 92.86 (54th percentile) in 11 months. Overall scores of parents’ experiences with the care team reached a mean of 96.7 (99th percentile) in “Nurses Overall” and a mean of 95.4 (99th percentile) in “Doctors Overall” scores. The NICU-FIRST team developed a NICU Handbook for parents, which included admission details, NICU course of the babies and discharge criteria for all infants. The team identified barriers with parents of infants who required shorter stay in the NICU and addressed them effectively. Pre-discharge screens and discharge teaching were formalized with a regularized schedule. Parental feedback response rate tripled from the baseline. The parent satisfaction scores remained high even with restricted visitation due to COVID pandemic.Conclusion(s): A team approach to encourage family involvement and responsibility improved the family satisfaction scores. Partnership of physician and nursing leaders was synergistic in reaching the target scores. In the process, NICU-FIRST team came up with innovative interventions and practical solutions. CHAIR project also aided this QI process in achieving the goals.
Figure 1. "Likelihood of recommending" Mean score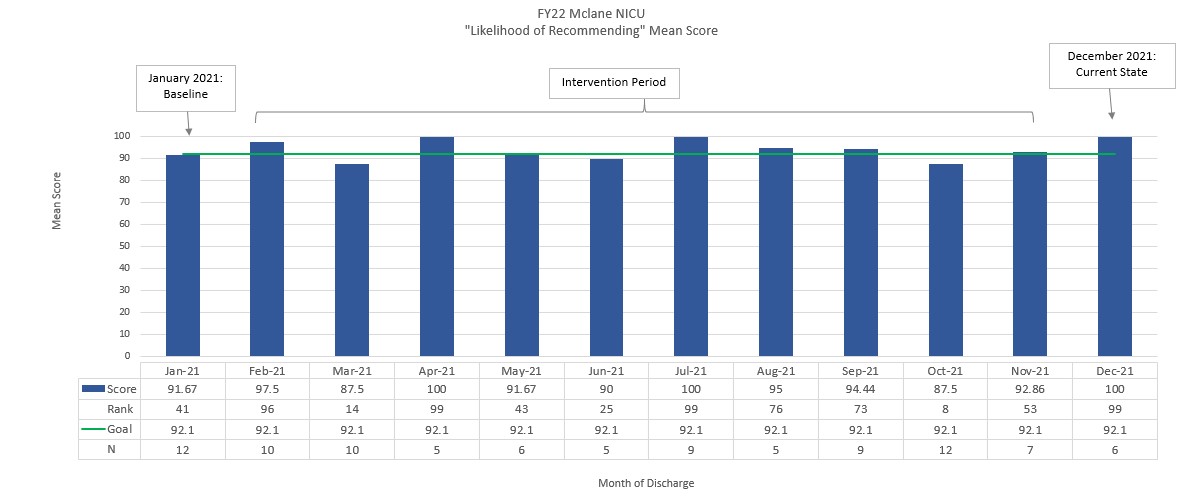
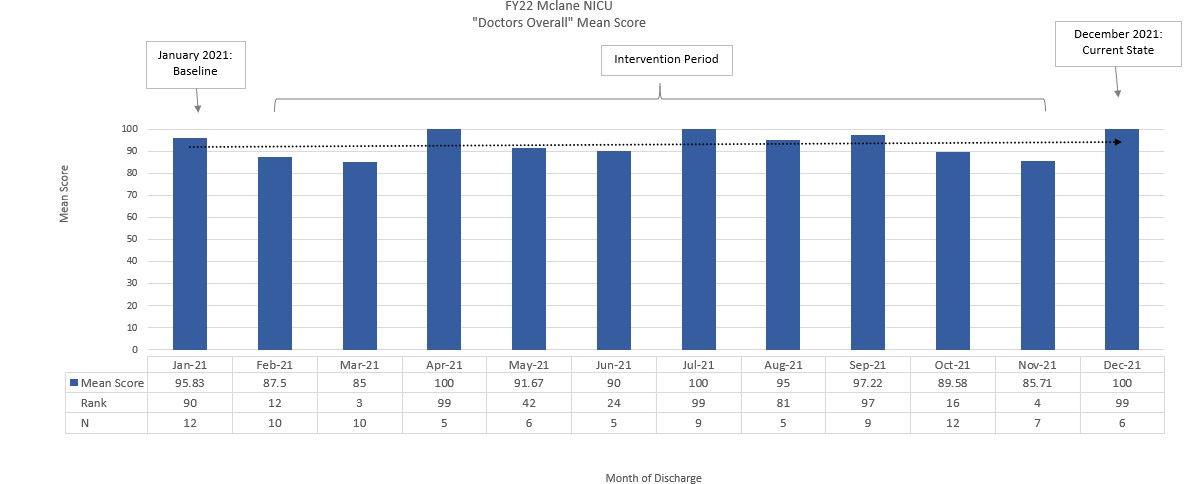
Figure 2. "Doctor Overall" Mean Score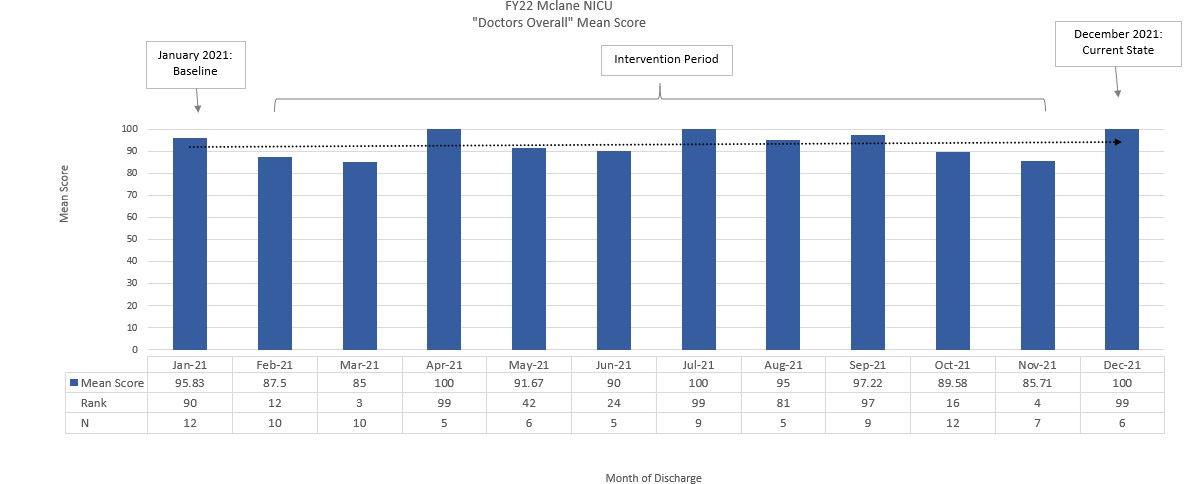
Objective: To identify opportunities and improve the family’s perception of their involvement, responsibility and satisfaction with the care provided to their infants. Success was recognized through an increased response return and improved satisfaction scores.
Design/Methods: NICU-FIRST, a multidisciplinary team, including a parent of NICU graduate, focused on the importance of family feedback related to the discharge process. An initiative was implemented titled the “CHAIR” project, “Communication in Hospital giving Attention, Information and Respect, which aligned with the goals set forth for the Press Ganey NICU Survey scores. The 51 bed NICU is an open unit allowing the team members to encourage providers to be seated in a chair while talking to the families. Monthly Operating Review (MOR) meetings were held with a formal partnership of administration, nurse and physician leaders. Interactions between the pediatric units and the NICU helped identify on-going issues, idea sharing, and standardizing expectations for the discharge process.
Results: Overall Press Ganey scores in the NICU saw a significant improvement. The “likelihood of recommending” question increased from a mean score of 91.67 (43rd percentile) to 92.86 (54th percentile) in 11 months. Overall scores of parents’ experiences with the care team reached a mean of 96.7 (99th percentile) in “Nurses Overall” and a mean of 95.4 (99th percentile) in “Doctors Overall” scores. The NICU-FIRST team developed a NICU Handbook for parents, which included admission details, NICU course of the babies and discharge criteria for all infants. The team identified barriers with parents of infants who required shorter stay in the NICU and addressed them effectively. Pre-discharge screens and discharge teaching were formalized with a regularized schedule. Parental feedback response rate tripled from the baseline. The parent satisfaction scores remained high even with restricted visitation due to COVID pandemic.Conclusion(s): A team approach to encourage family involvement and responsibility improved the family satisfaction scores. Partnership of physician and nursing leaders was synergistic in reaching the target scores. In the process, NICU-FIRST team came up with innovative interventions and practical solutions. CHAIR project also aided this QI process in achieving the goals.
Figure 1. "Likelihood of recommending" Mean score
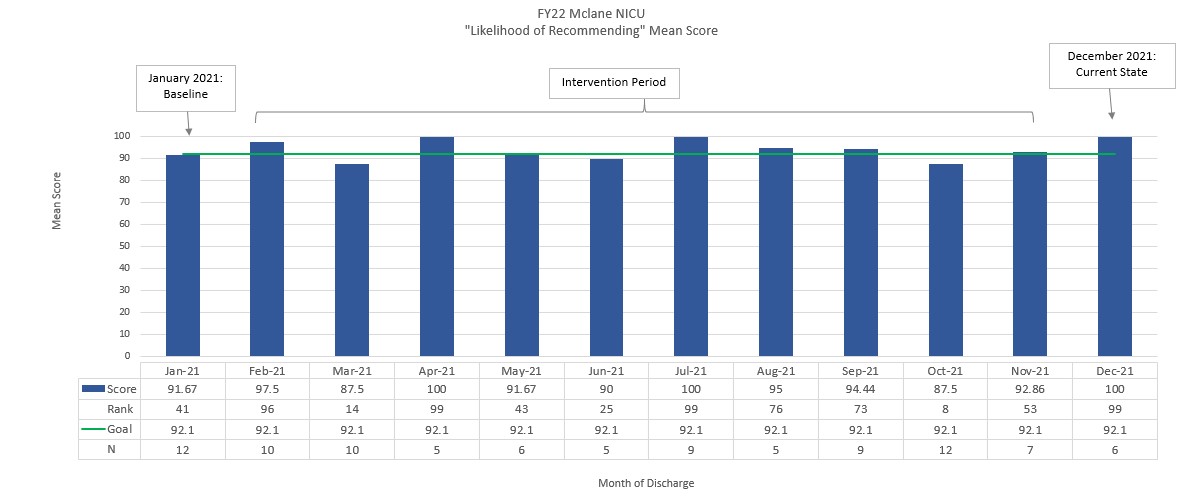
Figure 2. "Doctor Overall" Mean Score