Back
Neonatal General
Category: Abstract Submission
Neonatology General 8: Health Disparities - Health Services Research
222 - Spatial Patterns of Spontaneous and Medically Indicated Preterm Birth in Philadelphia
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 222
Publication Number: 222.339
Publication Number: 222.339
Nancy Yang, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Harrison Quick, Drexel University, Philadelphia, PA, United States; Steven J. Melly, Drexel University, Philadelphia, PA, United States; Anne M. Mullin, Tufts University School of Medicine, Brookline, MA, United States; Leah H. Schinasi, Drexel University Dornsife School of Public Health, Philadelphia, PA, United States; Heather Burris, Children's Hospital of Philadelphia, Philadelphia, PA, United States
Nancy Yang, BA
Clinical Research Assistant
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Understanding area-level patterns of preterm birth (PTB) may inform social and environmental determinants of PTB and PTB disparities. Because spontaneous preterm birth (sPTB) and medically indicated preterm birth (mPTB) may have different underlying causes, reliable estimates of small-scale geographic variations in PTB, sPTB, and mPTB rates are needed.
Objective: (1) To detect and compare neighborhood spatial patterns of PTB, sPTB, and mPTB across block groups in Philadelphia using spatial methods that account for sparse numbers and allow derivation of more reliable small area estimates and (2) to determine whether spatial patterns differed between Black and non-Black patients.
Design/Methods: We used a pregnancy cohort of singleton births at two Penn Medicine hospitals in 2008-2020. Each PTB ( < 37 wks’ gestation) was manually classified by two independent, blinded reviewers as sPTB (e.g., preterm labor, spontaneous rupture of membranes) or mPTB (e.g., clinician initiated due to maternal or fetal health condition). Addresses at birth were geocoded, and residential block groups were included in the analysis if they were contained within census tracts where ≥25% of births occurred at Penn Medicine. We applied a Bayesian model that accounts for spatial dependence structures and smooths estimates of PTB rates by borrowing information from neighboring block groups to obtain more reliable estimates than one would by simply calculating percent of births that are preterm in each block group. We used Global Moran’s I to test whether PTB was spatially autocorrelated.
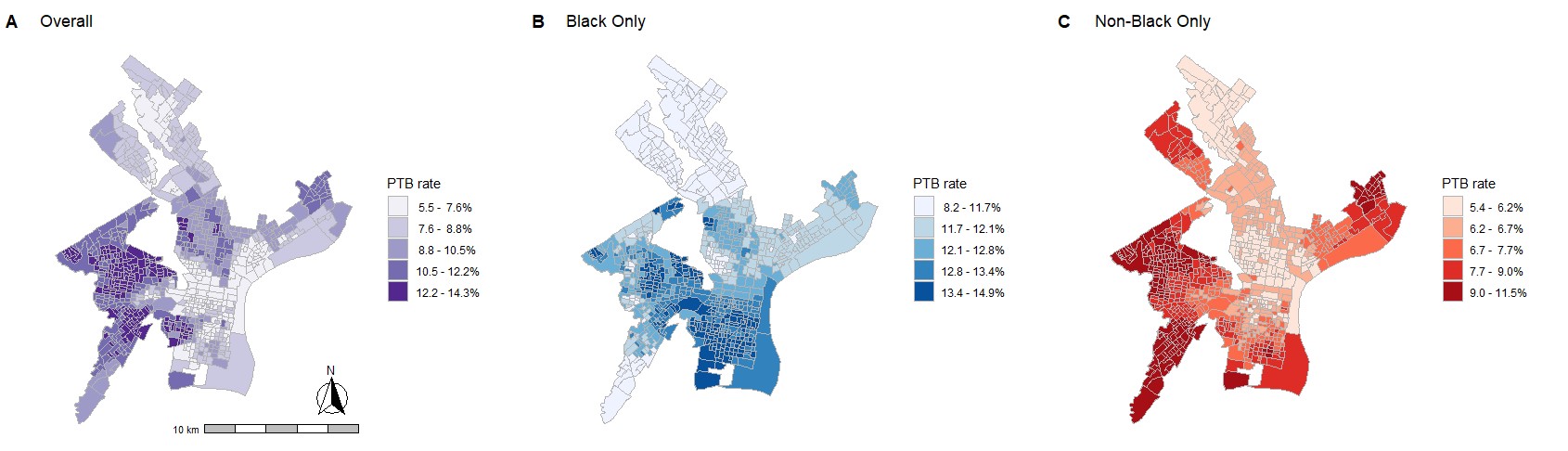
Results: 65,715 births were included in this analysis. There were 6670 (10.1%) PTBs, of which 3787 (56.8%) were sPTB, 2276 (34.1%) were mPTB, and 626 (9.1%) could not be adjudicated. Bayesian small area estimates revealed clustering of rates of PTB across different areas of Philadelphia, with PTB hot spots differing by race (Figure 1). For example, southwest Philadelphia is a hot spot for non-Black patients whereas South Philadelphia is a hot spot for Black patients. In addition, there were different spatial patterns of clustering of sPTB and mPTB (Figure 2). Moran’s I was significant for PTB overall and by race (p < 0.05), suggesting that PTB is not randomly distributed across the city.Conclusion(s): In Philadelphia, geographic patterns of PTB differ for Black vs. non-Black patients, and according to PTB phenotypes (sPTB vs. mPTB). Further analysis of spatial patterns and social and environmental exposures that may explain these geographic patterns may provide evidence needed to improve birth outcomes.
Figure 1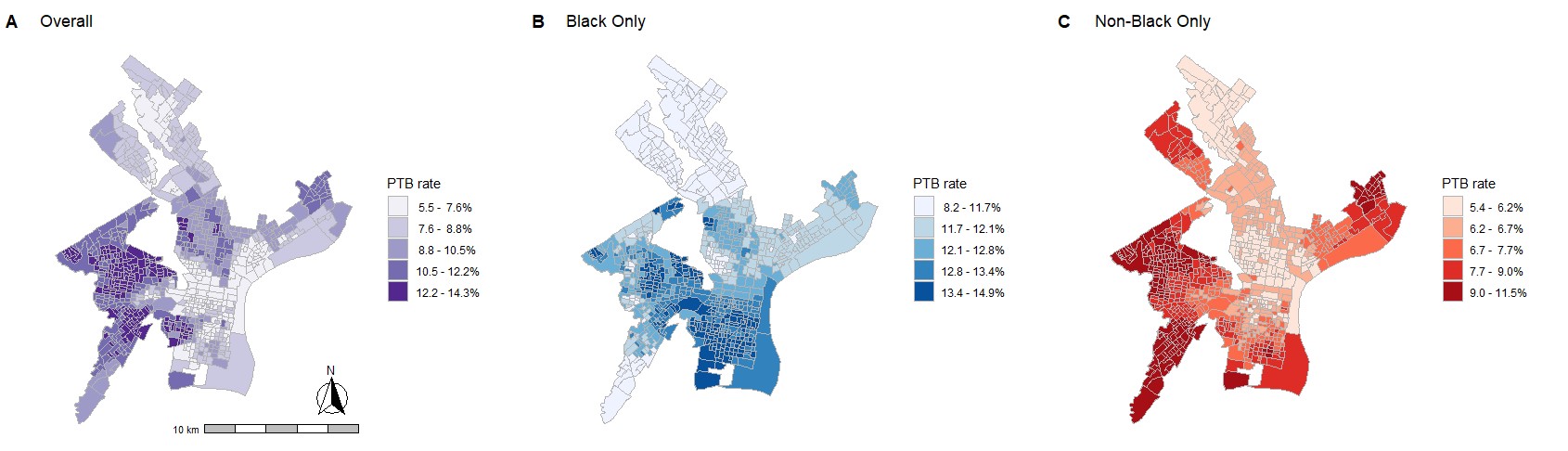 Spatial patterns of PTB rate among the overall population, Black patients, and non-Black patients
Spatial patterns of PTB rate among the overall population, Black patients, and non-Black patients
Figure 2.jpg) Spatial patterns of sPTB and mPTB rates among the overall population, Black patients, and non-Black patients
Spatial patterns of sPTB and mPTB rates among the overall population, Black patients, and non-Black patients
Objective: (1) To detect and compare neighborhood spatial patterns of PTB, sPTB, and mPTB across block groups in Philadelphia using spatial methods that account for sparse numbers and allow derivation of more reliable small area estimates and (2) to determine whether spatial patterns differed between Black and non-Black patients.
Design/Methods: We used a pregnancy cohort of singleton births at two Penn Medicine hospitals in 2008-2020. Each PTB ( < 37 wks’ gestation) was manually classified by two independent, blinded reviewers as sPTB (e.g., preterm labor, spontaneous rupture of membranes) or mPTB (e.g., clinician initiated due to maternal or fetal health condition). Addresses at birth were geocoded, and residential block groups were included in the analysis if they were contained within census tracts where ≥25% of births occurred at Penn Medicine. We applied a Bayesian model that accounts for spatial dependence structures and smooths estimates of PTB rates by borrowing information from neighboring block groups to obtain more reliable estimates than one would by simply calculating percent of births that are preterm in each block group. We used Global Moran’s I to test whether PTB was spatially autocorrelated.
Results: 65,715 births were included in this analysis. There were 6670 (10.1%) PTBs, of which 3787 (56.8%) were sPTB, 2276 (34.1%) were mPTB, and 626 (9.1%) could not be adjudicated. Bayesian small area estimates revealed clustering of rates of PTB across different areas of Philadelphia, with PTB hot spots differing by race (Figure 1). For example, southwest Philadelphia is a hot spot for non-Black patients whereas South Philadelphia is a hot spot for Black patients. In addition, there were different spatial patterns of clustering of sPTB and mPTB (Figure 2). Moran’s I was significant for PTB overall and by race (p < 0.05), suggesting that PTB is not randomly distributed across the city.Conclusion(s): In Philadelphia, geographic patterns of PTB differ for Black vs. non-Black patients, and according to PTB phenotypes (sPTB vs. mPTB). Further analysis of spatial patterns and social and environmental exposures that may explain these geographic patterns may provide evidence needed to improve birth outcomes.
Figure 1
 Spatial patterns of PTB rate among the overall population, Black patients, and non-Black patients
Spatial patterns of PTB rate among the overall population, Black patients, and non-Black patientsFigure 2
.jpg) Spatial patterns of sPTB and mPTB rates among the overall population, Black patients, and non-Black patients
Spatial patterns of sPTB and mPTB rates among the overall population, Black patients, and non-Black patients