General Pediatrics: All Areas
Category: Abstract Submission
General Pediatrics IV
186 - Surviving or Thriving? A Qualitative Assessment of Barriers to Follow-up Care after Hospitalization for Pediatric Sepsis
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 186
Publication Number: 186.317
Publication Number: 186.317
James A. Watson, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Patricia Z. Labellarte, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Melissa L. Turner, Pediatric Associates of Arlington Heights, Arlington Hieghts, IL, United States; Ashley Hayes, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Adam B. Becker, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Rebecca Stephen, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
Andrew Watson, MD
Fellow, Pediatric Hospital Medicine
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: While there has been a decrease in mortality from community-acquired pediatric sepsis in recent decades, deterioration in patient-reported health-related quality of life has been described in approximately one-fourth of survivors. There are currently no screening tools or guidelines for pediatricians to identify which patients may require more resources in post-hospital discharge follow-up.
Objective: To identify themes of pediatric providers current practices, knowledge, and existing barriers to care following hospitalization for sepsis
Design/Methods: Semi-structured interviews were conducted with 18 providers, including hospital providers identified as sepsis content experts and primary care providers (PCPs), between March and May 20, 2021. Interview questions focused on provider knowledge, preparedness, available resources, and barriers to identification of sequelae associated with hospitalization for sepsis. Interviews were audio-recorded, transcribed, de-identified, and then analyzed using qualitative and mixed methods analysis software (Dedoose Version 8.3.47b) to uncover any themes using a constant comparative approach.
Results: We interviewed 8 PCPs from 7 practices in a metropolitan area and 10 sepsis experts with expertise in infectious disease, critical care, emergency medicine, and hospital medicine (range 1-22 years in practice) (Table 1). Common themes were identified by PCPs and hospital providers including heterogeneity of complications (e.g. physical, emotional, social) and variable discharge communication between inpatient teams and PCPs (e.g. incomplete discharge summaries, insufficient verbal handoff) (Table 2). PCPs noted a lack of personal experience identifying long-term complications of sepsis, lack of reliable screening tools, and difficulty determining which problems were attributable to sepsis as barriers. Hospital providers noted a lack of comfort in counseling families to identify and seek treatment for morbidities of sepsis, including setting expectations of possible long-term sequelae following discharge.Conclusion(s): Providers highlighted multiple barriers in identifying and treating new morbidities in patients surviving sepsis hospitalization, including mental health and psycho-social sequelae. Further exploration of provider-identified themes and study of patient and family-identified barriers warrant additional investigation. Initiatives to address the post-hospital discharge care of sepsis survivors, including improvements in the hospital to ambulatory transition, may alleviate barriers and improve patient care and health outcomes in this high-risk population.
Table 1: Providers interviewed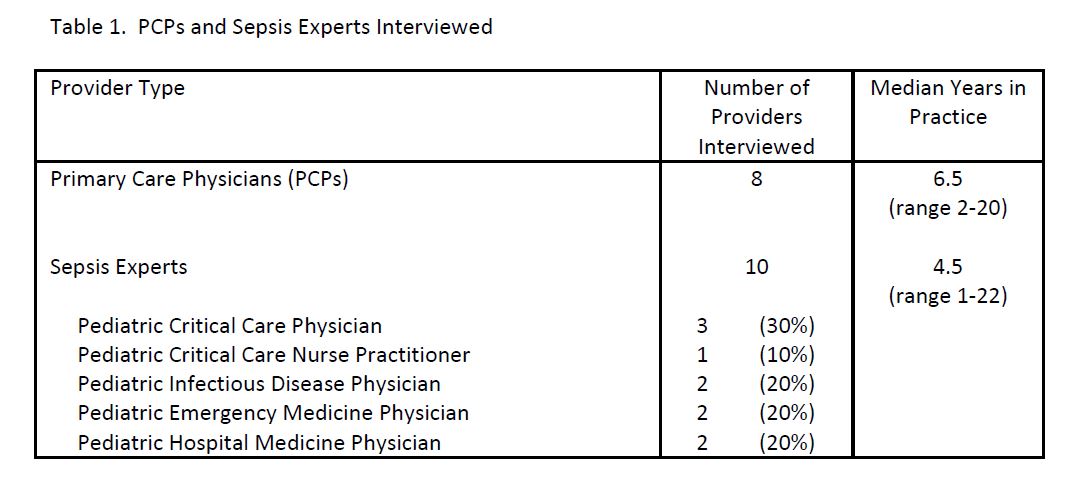
Table 2: Provider quotations.jpg)
Objective: To identify themes of pediatric providers current practices, knowledge, and existing barriers to care following hospitalization for sepsis
Design/Methods: Semi-structured interviews were conducted with 18 providers, including hospital providers identified as sepsis content experts and primary care providers (PCPs), between March and May 20, 2021. Interview questions focused on provider knowledge, preparedness, available resources, and barriers to identification of sequelae associated with hospitalization for sepsis. Interviews were audio-recorded, transcribed, de-identified, and then analyzed using qualitative and mixed methods analysis software (Dedoose Version 8.3.47b) to uncover any themes using a constant comparative approach.
Results: We interviewed 8 PCPs from 7 practices in a metropolitan area and 10 sepsis experts with expertise in infectious disease, critical care, emergency medicine, and hospital medicine (range 1-22 years in practice) (Table 1). Common themes were identified by PCPs and hospital providers including heterogeneity of complications (e.g. physical, emotional, social) and variable discharge communication between inpatient teams and PCPs (e.g. incomplete discharge summaries, insufficient verbal handoff) (Table 2). PCPs noted a lack of personal experience identifying long-term complications of sepsis, lack of reliable screening tools, and difficulty determining which problems were attributable to sepsis as barriers. Hospital providers noted a lack of comfort in counseling families to identify and seek treatment for morbidities of sepsis, including setting expectations of possible long-term sequelae following discharge.Conclusion(s): Providers highlighted multiple barriers in identifying and treating new morbidities in patients surviving sepsis hospitalization, including mental health and psycho-social sequelae. Further exploration of provider-identified themes and study of patient and family-identified barriers warrant additional investigation. Initiatives to address the post-hospital discharge care of sepsis survivors, including improvements in the hospital to ambulatory transition, may alleviate barriers and improve patient care and health outcomes in this high-risk population.
Table 1: Providers interviewed
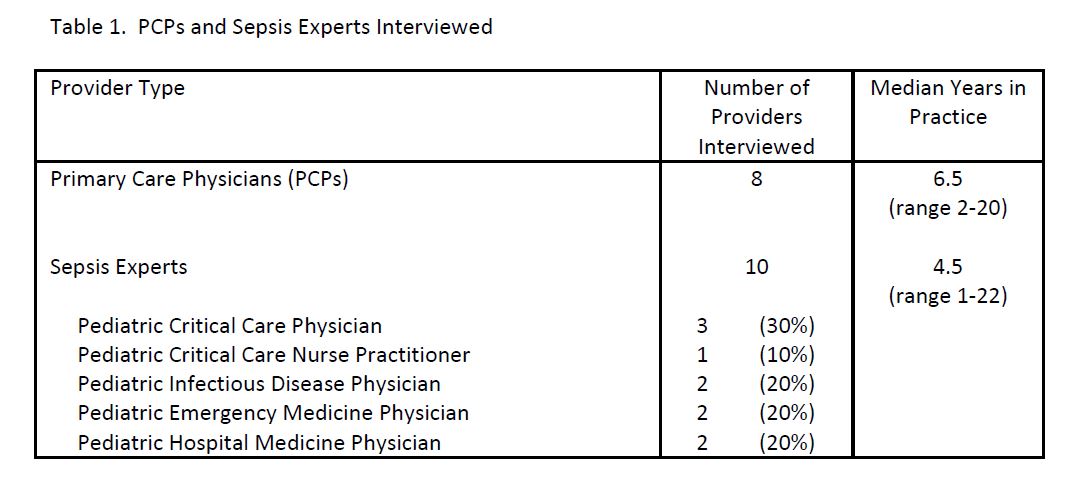
Table 2: Provider quotations
.jpg)
