Hospital Medicine: Hospital Medicine Quality Improvement
Category: Abstract Submission
Hospital Medicine: QI
334 - Medication Frustrations: Improving Discharge Medication Instructions for Families
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 334
Publication Number: 334.323
Publication Number: 334.323
Anna Brown, Akron Children's Hospital, Akron, OH, United States; Samantha M. Gunkelman, Akron Children's Hospital, Akron, OH, United States; Elizabeth Smith, Akron Children's Hospital, Akron, OH, United States

Emily Kramer, DO
Chief Resident
Akron Children's Hospital
Brecksville, Ohio, United States
Presenting Author(s)
Background: Transitioning care from inpatient to outpatient is known to be high risk time for medication errors. Standardizing the discharge medication instruction process by quality improvement methodology is known to decrease errors.
Objective: To increases the percentage of patients discharged from the Pediatric Hospital Medicine (PHM) service who received detailed discharge medication instructions on new prescriptions from 0% to 50% in a six-month period (Figure 1).
Design/Methods: A multidisciplinary team including a pediatric fellow, attending, nurse specialist, and pharmacist was created. The Model for Improvement was utilized and twice monthly data was collected from July 2021 – December 2021. MEDRITES model was used as a framework (Table 1). Documentation of at least five MEDRITES components was required to meet criteria for discharge instructions. Pediatric residents were the primary target of interventions as they are primarily responsible for discharge instructions for patients on the PHM service. A survey of residents identified medication knowledge as the primary barrier to provide appropriate discharge medication instructions to families. Multiple Plan-Do-Study-Act cycles were conducted including education on rounding doses for easy administration, tips of administering medication to children, medication instruction tip sheets, creating templates of instructions in the electronic health record for the most commonly prescribed new medications and including reviewing instructions on rounds.
Results: The key process measure was the percentage of patients discharged from the PHM service with new medication discharge instructions included in their After Visit Summary. The frequency of discharge medication instructions provided at discharge had a statistically significant increase from a baseline 0% to 38.3% in 6 months (Figure 2).Conclusion(s): Interventions implemented through this project led to an improvement in medication instructions given to families as well as increasing awareness of the importance of this education for families. To meet the goal of 50% instruction rate, next steps include the development of pre-recorded educational videos and further education on use of templated instructions in the electronic medical record. A goal of future work is to include the development of patient-based outcomes.
Figure 1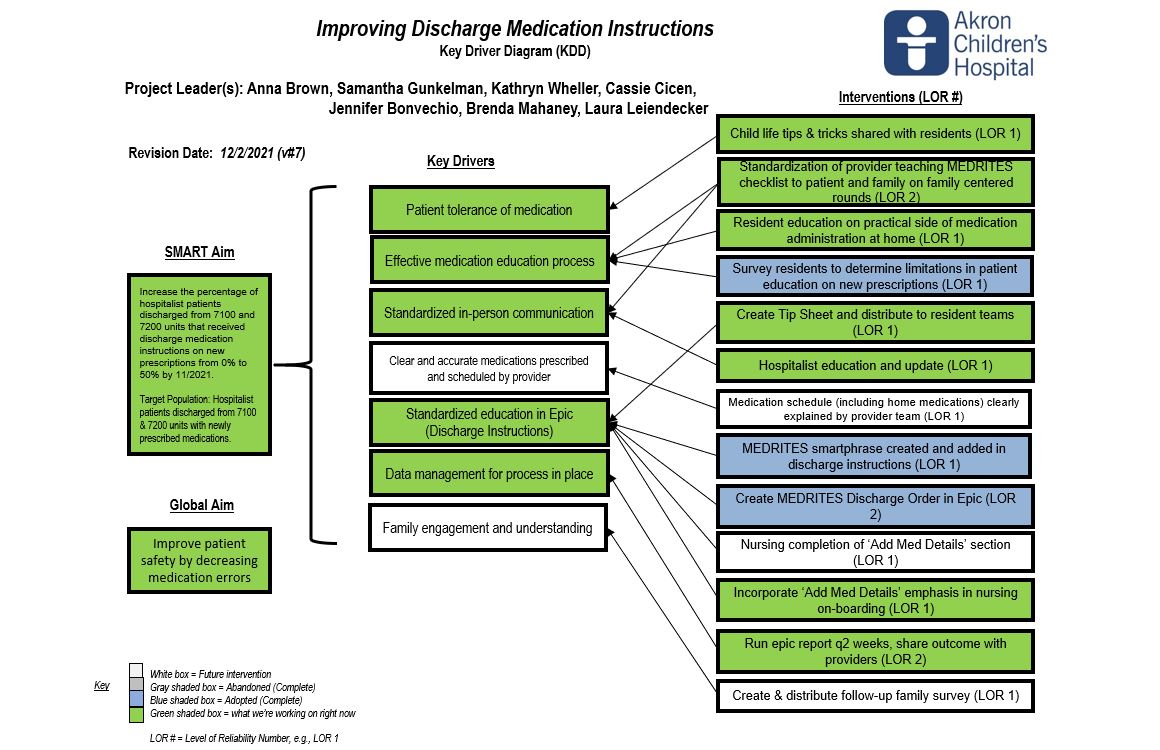 Key Driver Diagram
Key Driver Diagram
Figure 2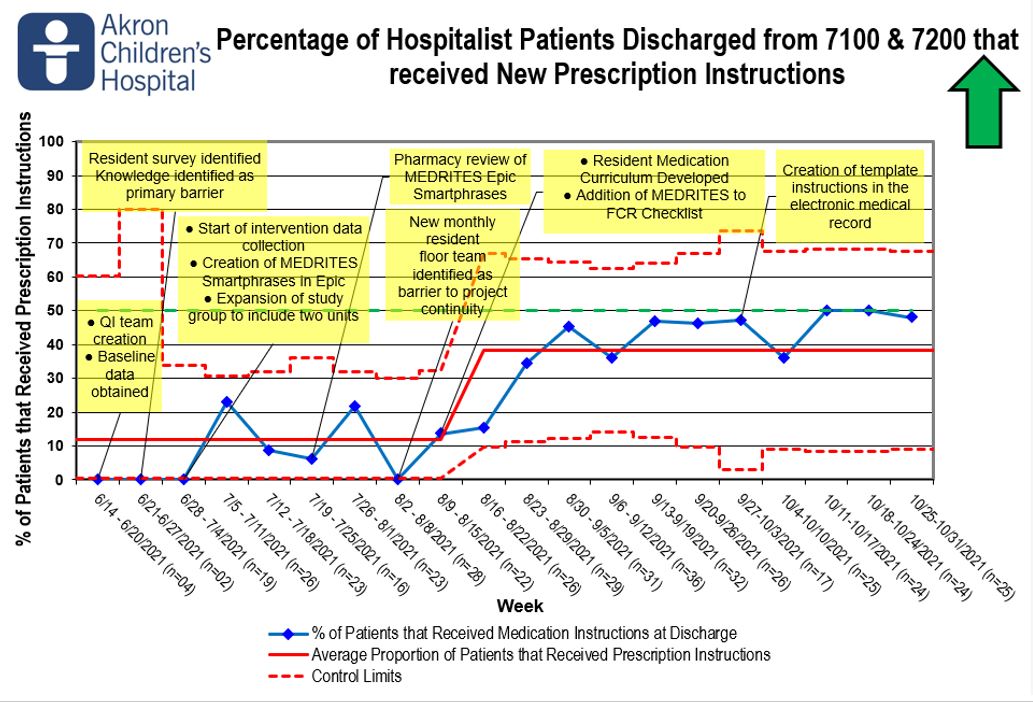 Discharge Medication Instruction P-Chart
Discharge Medication Instruction P-Chart
Objective: To increases the percentage of patients discharged from the Pediatric Hospital Medicine (PHM) service who received detailed discharge medication instructions on new prescriptions from 0% to 50% in a six-month period (Figure 1).
Design/Methods: A multidisciplinary team including a pediatric fellow, attending, nurse specialist, and pharmacist was created. The Model for Improvement was utilized and twice monthly data was collected from July 2021 – December 2021. MEDRITES model was used as a framework (Table 1). Documentation of at least five MEDRITES components was required to meet criteria for discharge instructions. Pediatric residents were the primary target of interventions as they are primarily responsible for discharge instructions for patients on the PHM service. A survey of residents identified medication knowledge as the primary barrier to provide appropriate discharge medication instructions to families. Multiple Plan-Do-Study-Act cycles were conducted including education on rounding doses for easy administration, tips of administering medication to children, medication instruction tip sheets, creating templates of instructions in the electronic health record for the most commonly prescribed new medications and including reviewing instructions on rounds.
Results: The key process measure was the percentage of patients discharged from the PHM service with new medication discharge instructions included in their After Visit Summary. The frequency of discharge medication instructions provided at discharge had a statistically significant increase from a baseline 0% to 38.3% in 6 months (Figure 2).Conclusion(s): Interventions implemented through this project led to an improvement in medication instructions given to families as well as increasing awareness of the importance of this education for families. To meet the goal of 50% instruction rate, next steps include the development of pre-recorded educational videos and further education on use of templated instructions in the electronic medical record. A goal of future work is to include the development of patient-based outcomes.
Figure 1
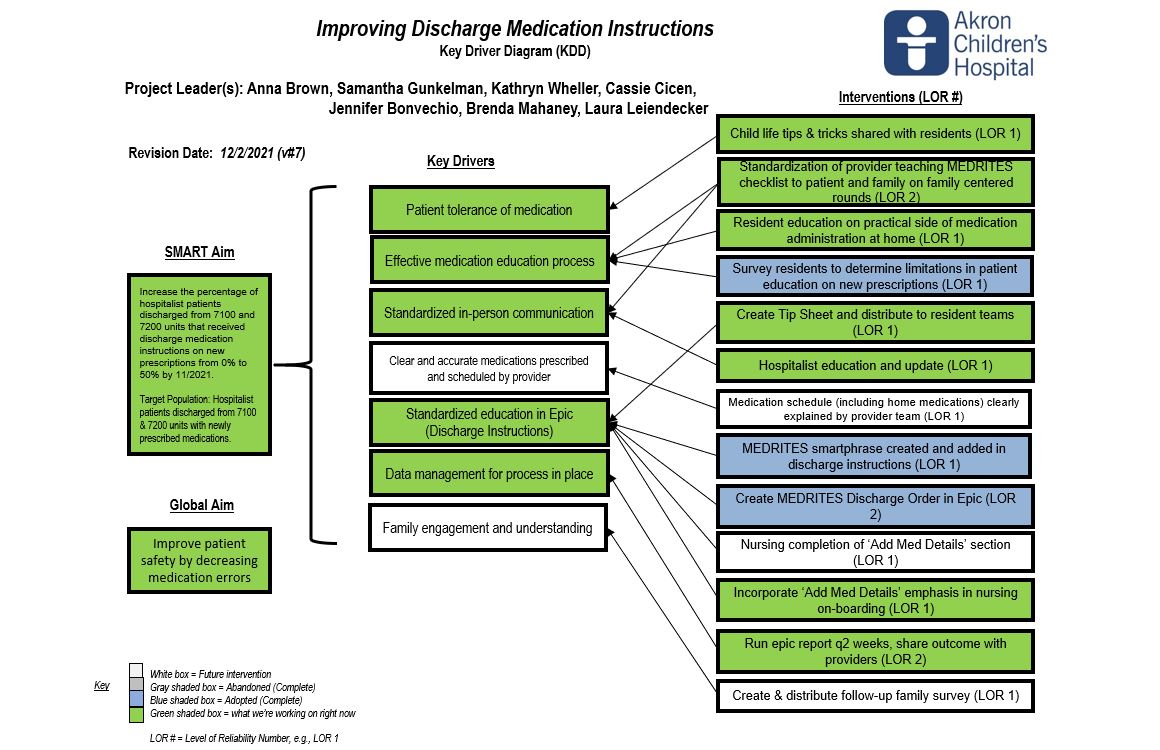 Key Driver Diagram
Key Driver DiagramFigure 2
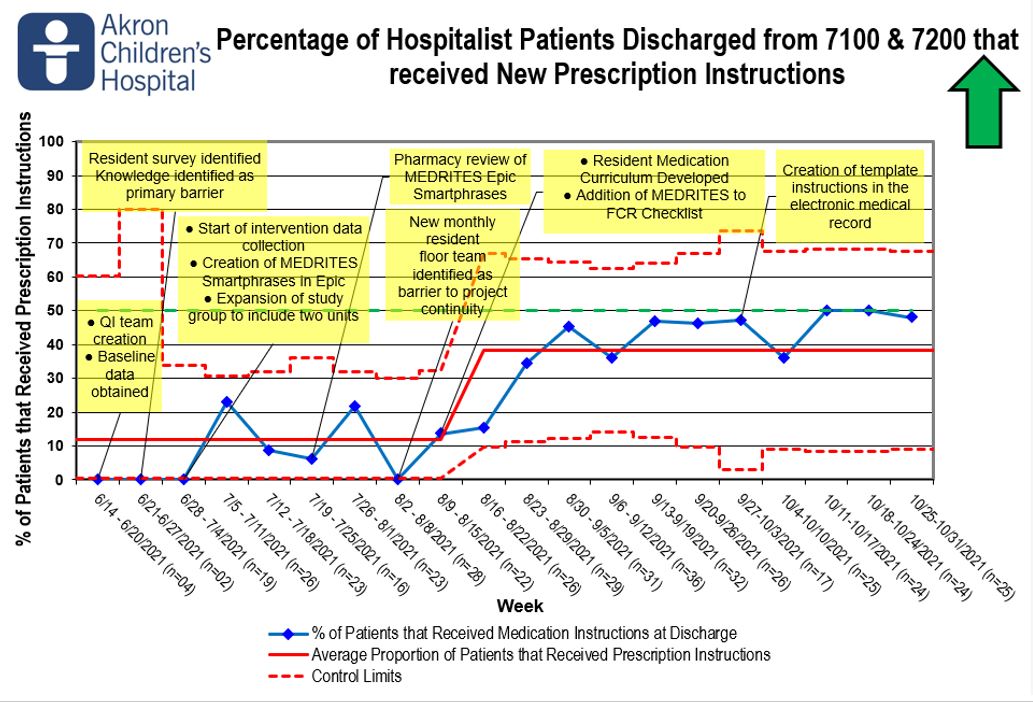 Discharge Medication Instruction P-Chart
Discharge Medication Instruction P-Chart