Breastfeeding/Human Milk
Category: Abstract Submission
Breastfeeding/Human Milk I
415 - Evaluation of exclusive breastfeeding rates in infants less than 90 days old during the initial months of the COVID-19 pandemic
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 415
Publication Number: 415.301
Publication Number: 415.301
Sophie K. Shaikh, Duke, Durham, NC, United States; Melissa C. Kay, Duke University School of Medicine, Durham, NC, United States; Emily A. Hannon, Western Wake Pediatrics, Chapel Hill, NC, United States; Elizabeth S. Erickson, Duke Children's Primary Care, Durham, NC, United States; Gabriela M. Maradiaga Panayotti, Duke University School of Medicine, Durham, NC, United States; Dean S. Miner, Duke University School of Medicine, Durham, NC, United States; Charles Wood, Duke University School of Medicine, Durham, NC, United States
.jpg)
Charles T. Wood, MD, MPH (he/him/his)
Assistant Professor
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background: Stay-at-home recommendations and, later, mandates, at the onset of the COVID-19 pandemic changed access to medical providers and threatened breastfeeding families’ access to lactation support. This support is critical during the newborn period when milk supply is being established.
Objective: To examine the hypothesis that exclusive breastfeeding rates in infants aged less than 90 days during the stay-at-home restrictions in 2020 would be lower than rates in infants during a similar period in 2019.
Design/Methods: We retrospectively analyzed breastfeeding data for infants born between 3/1/2020-4/30/2020 (when the local stay-at-home restrictions were in place) and seen for clinical evaluation in our academic pediatric practice. Data were compared to that of infants born 3/1/2019-4/30/2019 (pre-pandemic). Visits were categorized as newborn (age less than 7 days), follow up (7-21 days), 1 month (21-51 days), and 2 months (51-90 days). Feeding was categorized as exclusive breastfeeding, mixed breastfeeding and formula, or formula only. We used chi-square tests to compare 2019 and 2020 breastfeeding categories and performed logistic regression to compare odds of exclusive breastfeeding adjusted for known confounders, including maternal age, birth weight, sex, gestational age, birth order, and race and ethnicity.
Results: Data were collected from a total of 928 clinic visits in 2019 and 826 visits in 2020, representing 743 unique infants (382 in 2019 and 361 in 2020). The visits were evenly distributed between each age category, with fewer visits at 51-90 days than other categories, and were not statistically different between 2019 and 2020. Adjusted odds of exclusive breastfeeding did not differ between 2019 and 2020. However, we found significant associations between racial and ethnic groups and breastfeeding rates in infants less than 7 days old in 2020 that were not seen in 2019, despite no differences in the demographics of the infants during that time. At both newborn and follow up visits (Tables 1 and 2), a higher percentage of Hispanic infants were feeding formula in 2020 (25% and 19%) than in 2019 (6% and 7%).Conclusion(s): Although we did not find differences in overall rates of breastfeeding between 2019 and 2020, we did find differences in breastfeeding rates based on race and ethnicity for infants in the first month of life. This suggests that the COVID-19 pandemic and stay-at-home mandates did not affect breastfeeding infants in all racial and ethnic groups equally in the first month of life.
Table 1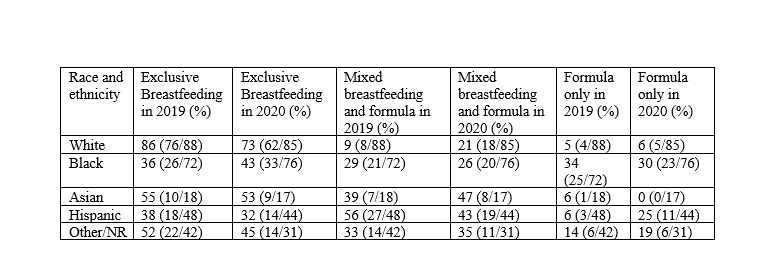 Breastfeeding rates by race and ethnicity among infants age less than 7 days born between 3/1 and 5/1 in 2019 and 2020
Breastfeeding rates by race and ethnicity among infants age less than 7 days born between 3/1 and 5/1 in 2019 and 2020
Table 2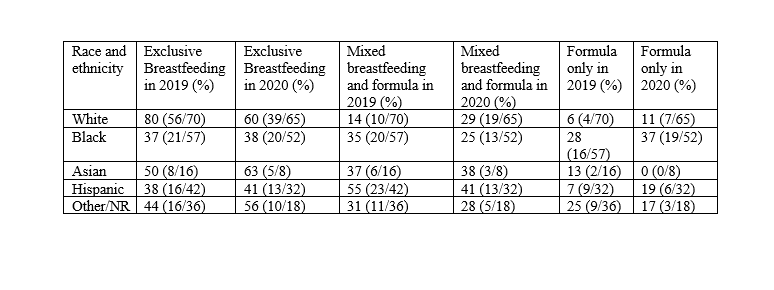 Breastfeeding rates by race and ethnicity among infants seen for follow up visits at ages 7-21 days old between 3/1 and 5/1 in 2019 and 2020
Breastfeeding rates by race and ethnicity among infants seen for follow up visits at ages 7-21 days old between 3/1 and 5/1 in 2019 and 2020
Objective: To examine the hypothesis that exclusive breastfeeding rates in infants aged less than 90 days during the stay-at-home restrictions in 2020 would be lower than rates in infants during a similar period in 2019.
Design/Methods: We retrospectively analyzed breastfeeding data for infants born between 3/1/2020-4/30/2020 (when the local stay-at-home restrictions were in place) and seen for clinical evaluation in our academic pediatric practice. Data were compared to that of infants born 3/1/2019-4/30/2019 (pre-pandemic). Visits were categorized as newborn (age less than 7 days), follow up (7-21 days), 1 month (21-51 days), and 2 months (51-90 days). Feeding was categorized as exclusive breastfeeding, mixed breastfeeding and formula, or formula only. We used chi-square tests to compare 2019 and 2020 breastfeeding categories and performed logistic regression to compare odds of exclusive breastfeeding adjusted for known confounders, including maternal age, birth weight, sex, gestational age, birth order, and race and ethnicity.
Results: Data were collected from a total of 928 clinic visits in 2019 and 826 visits in 2020, representing 743 unique infants (382 in 2019 and 361 in 2020). The visits were evenly distributed between each age category, with fewer visits at 51-90 days than other categories, and were not statistically different between 2019 and 2020. Adjusted odds of exclusive breastfeeding did not differ between 2019 and 2020. However, we found significant associations between racial and ethnic groups and breastfeeding rates in infants less than 7 days old in 2020 that were not seen in 2019, despite no differences in the demographics of the infants during that time. At both newborn and follow up visits (Tables 1 and 2), a higher percentage of Hispanic infants were feeding formula in 2020 (25% and 19%) than in 2019 (6% and 7%).Conclusion(s): Although we did not find differences in overall rates of breastfeeding between 2019 and 2020, we did find differences in breastfeeding rates based on race and ethnicity for infants in the first month of life. This suggests that the COVID-19 pandemic and stay-at-home mandates did not affect breastfeeding infants in all racial and ethnic groups equally in the first month of life.
Table 1
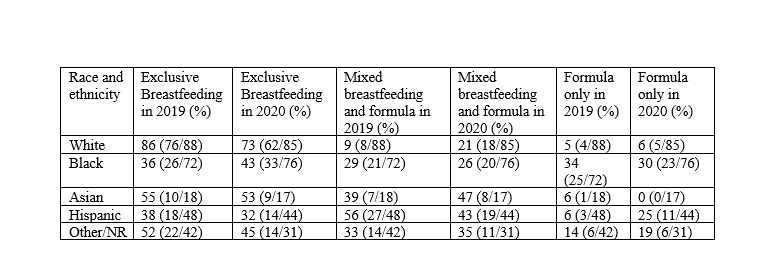 Breastfeeding rates by race and ethnicity among infants age less than 7 days born between 3/1 and 5/1 in 2019 and 2020
Breastfeeding rates by race and ethnicity among infants age less than 7 days born between 3/1 and 5/1 in 2019 and 2020Table 2
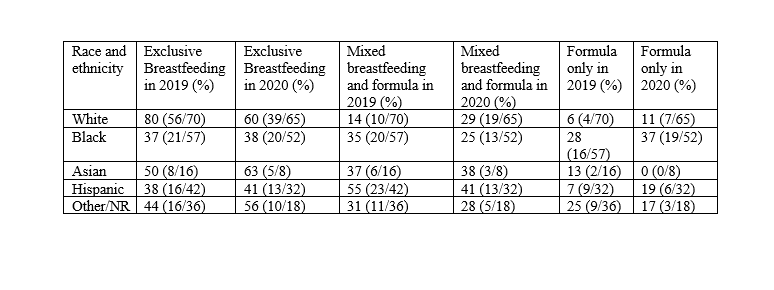 Breastfeeding rates by race and ethnicity among infants seen for follow up visits at ages 7-21 days old between 3/1 and 5/1 in 2019 and 2020
Breastfeeding rates by race and ethnicity among infants seen for follow up visits at ages 7-21 days old between 3/1 and 5/1 in 2019 and 2020