Nephrology: Clinical
Category: Abstract Submission
Nephrology III: General Nephrology and Dialysis
44 - Acute kidney injury in children with severe sepsis is associated with increased risk of mortality and health care utilization.
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 44
Publication Number: 44.340
Publication Number: 44.340
Jasmine Khatana, Metrohealth-Case Western Reserve Univ, Cleveland, OH, United States; Aravind Thavamani, UH Rainbow Babies and Children's Hospital/ Case Western Reserve University/, Cleveland, OH, United States; Krishna Kishore Umapathi, Rush University Medical Center, Chicago, IL, United States; Senthilkumar Sankararaman, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Aparna Roy, The MetroHealth System, Cleveland, OH, United States
- JK
Jasmine Khatana, MBBS, MD (she/her/hers)
Metro Health Medical Center
Cleveland, Ohio, United States
Presenting Author(s)
Background: Pediatric severe sepsis (PSS) is associated with increased risk of mortality. There is paucity of data on the impact of acute kidney injury (AKI) on hospital outcomes in PSS.
Objective: To analyze the impact of AKI on hospital outcomes in patients with PSS.
Design/Methods: We analyzed non-overlapping years of the Kids Inpatient Database (KID) and National Inpatient Sample (NIS) database between 2003 and 2014 of all pediatric patients with severe sepsis up to 20 years of age. PSS was defined using specific International Classification of Diseases (ICD) codes and modified Angus criteria. Using ICD-9 diagnosis codes, patients were divided into two groups based on presence of AKI and were compared for outcomes measures including in-hospital mortality and healthcare resource utilization using the length of stay and inflation-adjusted hospitalization charges. We included various common comorbid conditions which predispose so PSS and focus of infection as covariates in the regression model.
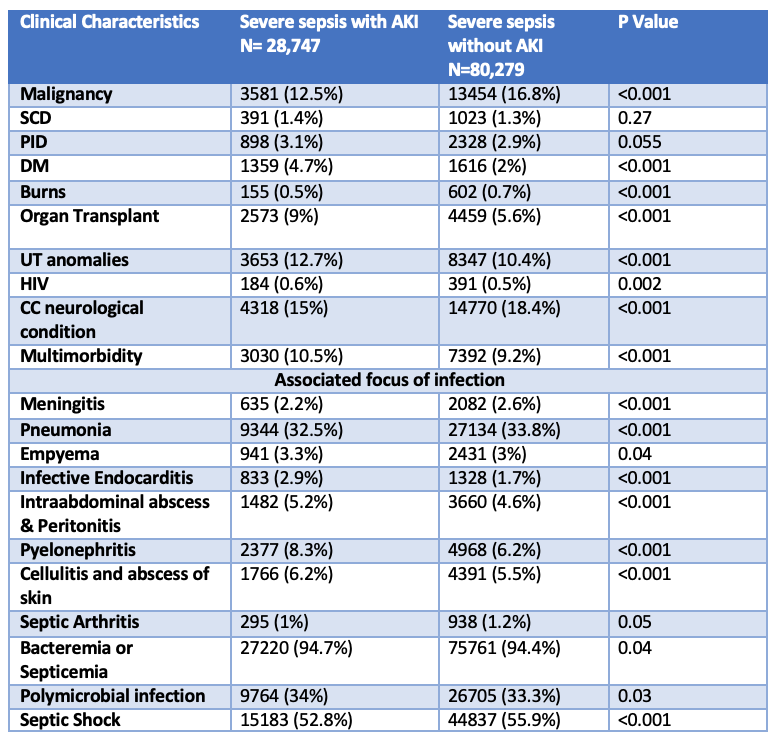
Results: We analyzed 109 027 hospitalizations due to PSS during the study period. The prevalence rate of AKI in PSS was 26.4%. Patients with AKI were significantly older, more often males and public insurance compared to those without AKI (Table 1). PSS patients with Diabetes mellitus, immunodeficiency disorders including HIV, urinary tract abnormality and multiple comorbidities had increased prevalence of AKI, P< 0.01 (Table 2). Similarly increased prevalence of AKI was observed in patients with infective endocarditis, intraabdominal infection, cellulitis, and skin infection (Table 2). Mortality rate was significantly higher among patients with AKI (22.7% vs 10.7%, P< 0.001). Multivariate logistic regression analysis showed that AKI was associated with 2.9 times increased odds of mortality (95% CI:2.3 to 3.1; P< 0.001). PSS with AKI had significantly higher median length of stay (13 vs 10) and total hospitalization charges (137495 vs 84176), P< 0.001.Conclusion(s): 1 out of 4 hospitalizations with PSS had AKI and was associated with almost 3 times increased risk of mortality and increased health care resource utilization. Our findings help identify comorbid conditions more commonly associated with AKI and aggressive management of these at-risk population to improve hospital outcomes.
Table 1: Comparison of demographics of pediatric patients with severe sepsis..png)
Table 2. Clinical comorbid conditions in patients with severe sepsis.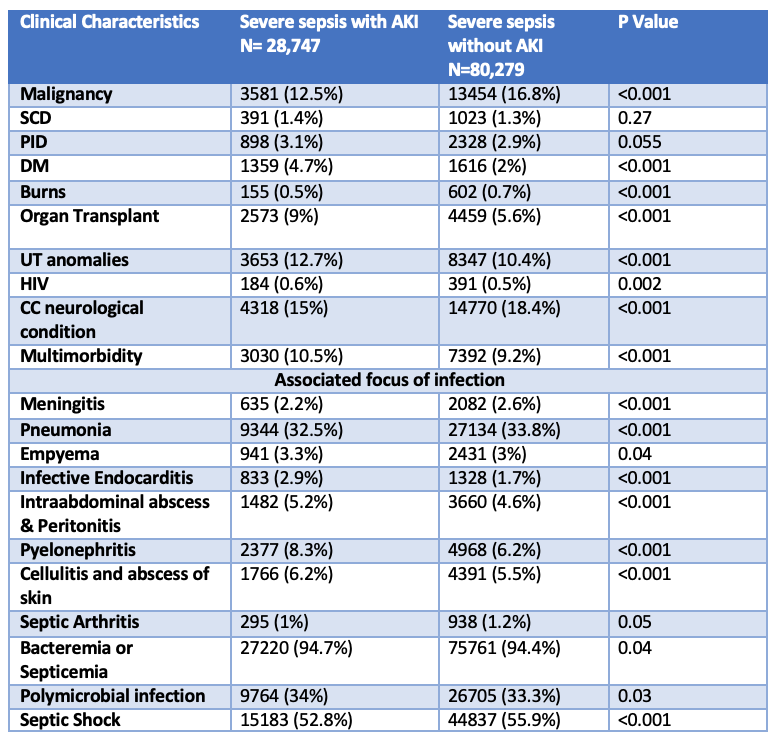
Objective: To analyze the impact of AKI on hospital outcomes in patients with PSS.
Design/Methods: We analyzed non-overlapping years of the Kids Inpatient Database (KID) and National Inpatient Sample (NIS) database between 2003 and 2014 of all pediatric patients with severe sepsis up to 20 years of age. PSS was defined using specific International Classification of Diseases (ICD) codes and modified Angus criteria. Using ICD-9 diagnosis codes, patients were divided into two groups based on presence of AKI and were compared for outcomes measures including in-hospital mortality and healthcare resource utilization using the length of stay and inflation-adjusted hospitalization charges. We included various common comorbid conditions which predispose so PSS and focus of infection as covariates in the regression model.
Results: We analyzed 109 027 hospitalizations due to PSS during the study period. The prevalence rate of AKI in PSS was 26.4%. Patients with AKI were significantly older, more often males and public insurance compared to those without AKI (Table 1). PSS patients with Diabetes mellitus, immunodeficiency disorders including HIV, urinary tract abnormality and multiple comorbidities had increased prevalence of AKI, P< 0.01 (Table 2). Similarly increased prevalence of AKI was observed in patients with infective endocarditis, intraabdominal infection, cellulitis, and skin infection (Table 2). Mortality rate was significantly higher among patients with AKI (22.7% vs 10.7%, P< 0.001). Multivariate logistic regression analysis showed that AKI was associated with 2.9 times increased odds of mortality (95% CI:2.3 to 3.1; P< 0.001). PSS with AKI had significantly higher median length of stay (13 vs 10) and total hospitalization charges (137495 vs 84176), P< 0.001.Conclusion(s): 1 out of 4 hospitalizations with PSS had AKI and was associated with almost 3 times increased risk of mortality and increased health care resource utilization. Our findings help identify comorbid conditions more commonly associated with AKI and aggressive management of these at-risk population to improve hospital outcomes.
Table 1: Comparison of demographics of pediatric patients with severe sepsis.
.png)
Table 2. Clinical comorbid conditions in patients with severe sepsis.