Infectious Diseases
Category: Abstract Submission
Infectious Diseases: COVID-19
302 - Risk Factors for Severe COVID-19 in Children
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 302
Publication Number: 302.215
Publication Number: 302.215
Esra Akkoyun, University of Texas Southwestern Medical School, Irving, TX, United States; Meera Devarajan, University of Texas Southwestern Medical School, Dallas, TX, United States; Bilal Ashraf, University of Texas Southwestern Medical School, Dallas, TX, United States; Natasha W. Wyndham Hanners, University of Texas Southwestern Medical School, Dallas, TX, United States; Jeffrey Kahn, University of Texas Southwestern Medical Center, Dallas, TX, United States; Zachary M. Most, University of Texas Southwestern Medical Center, Dallas, TX, United States

Esra Akkoyun, MD
Fellow
University of Texas Southwestern Medical School
Irving, Texas, United States
Presenting Author(s)
Background: Children with medical co-morbidities may be at higher risk of hospitalization and need for critical care from coronavirus disease 2019 (COVID-19). Extremes of age and comorbid conditions have been shown as predictors of severe disease in children.
Objective: To determine the risk factors for hospitalization and critical disease due to COVID-19 in pediatric patients.
Design/Methods: We conducted a case control study of 300 patients with COVID-19 from July 1 – August 14, 2020. Two distinct outcomes were evaluated. The first categorized individuals hospitalized with symptomatic COVID-19 (Hospital) vs. individuals with COVID-19 not hospitalized or hospitalized with asymptomatic COVID-19 (Nonhospital). The second categorized individuals who required critical care (ICU) vs. individuals who did not require critical care (Floor). Demographics, medical co-morbidities, and symptoms at presentation were compared. Univariable analysis was done utilizing the Mann Whitney U test or the chi square test.
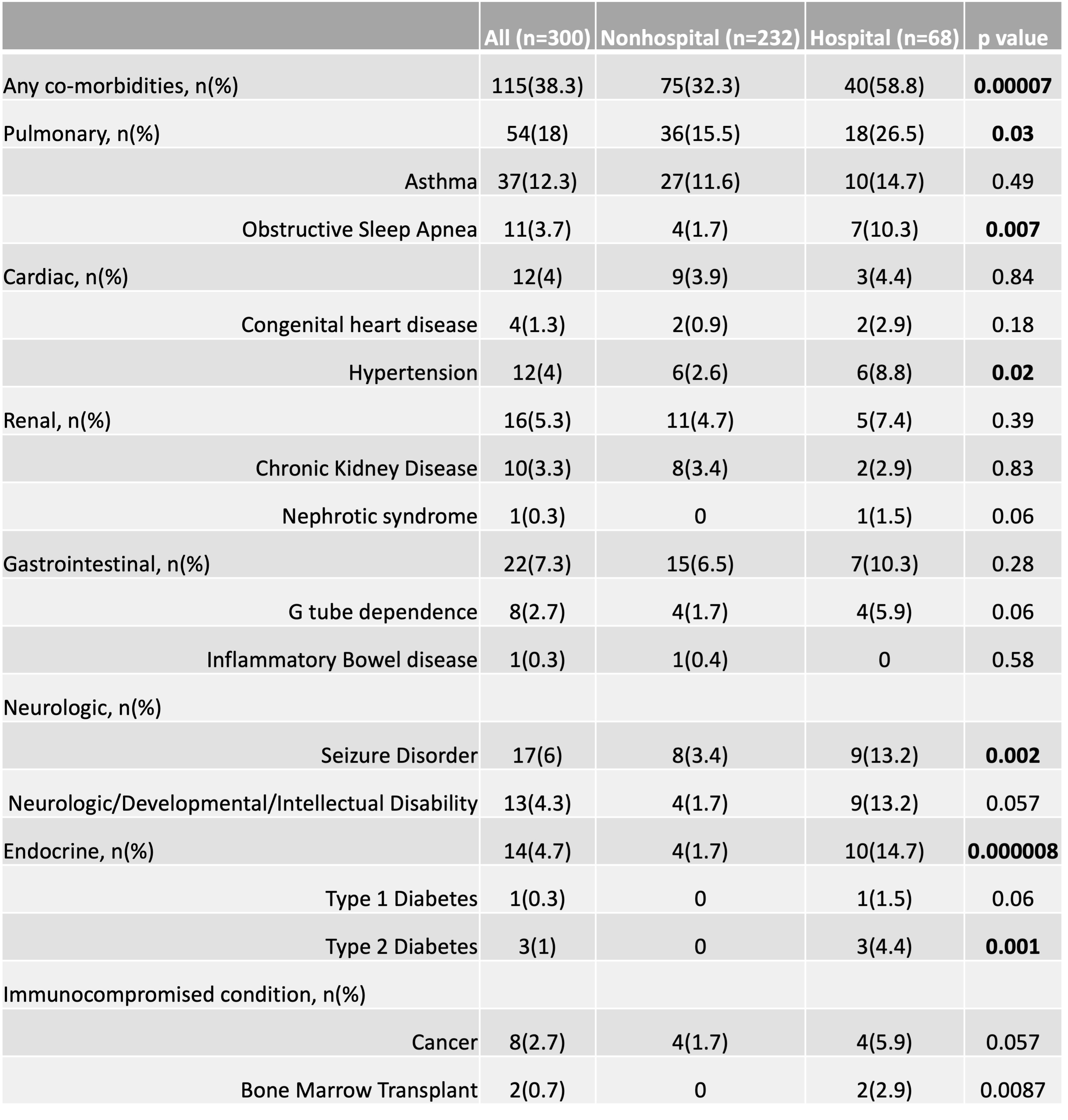
Results: Of 300 children, 68 (22.6%) were hospitalized and symptomatic. The Hospital group trended towards being older (6.5 vs 9.9 years, p=0.16) and more likely to be African American (25% vs 13.3%, p=0.03) compared to the Nonhospital group. The Hospital group was more likely to have any comorbidity (58.8% vs 32.3%, p < 0.0001), including diabetes mellitus (14.7% vs 1.7%, p=0.001), seizure disorder (13.2% vs 3.4%, p=0.002), hypertension (8.8% vs 2.6%, p=0.02), sickle cell disease (5.9% vs 0.4%, p=0.002), and bone marrow transplant (2.9% vs 0%, p=0.008). Nausea/vomiting (35.3% vs. 20.3%, p=0.01) and abdominal pain (23.5% vs 10.8%, p=0.07) were more common in the Hospital group, while rhinorrhea (7.4% vs. 17.7%, p=0.03) was more common in the Nonhospital group. The ICU group was more likely to have any comorbidity (82.4% vs 51%, p=0.02), including seizure disorder (35% vs 6%, p=0.001), obstructive sleep apnea (OSA) (29.4% vs 3.9%, p=0.002), gastrostomy tube dependence (23.5% vs 0%, p < 0.001), and neurological disability (29.4% vs 7.8%, p=0.02) than the Floor group. Shortness of breath (SOB) (47% vs 6%, p < 0.0001) and diarrhea (35% vs 6%, p=0.001) were more common among the ICU group.Conclusion(s): Children who required admission with symptomatic COVID-19 infection were more likely to have chronic medical conditions. Children who required critical care were more likely to have seizure disorder and OSA. Gastrointestinal complaints and SOB were more common symptoms in severe COVID-19. Larger studies are required to confirm the risk factors of severe/critical COVID-19 disease that we found among children.
Table 1: Demographic Characteristics.jpg)
Table 2: Co-morbidities in Nonhospital and Hospital Groups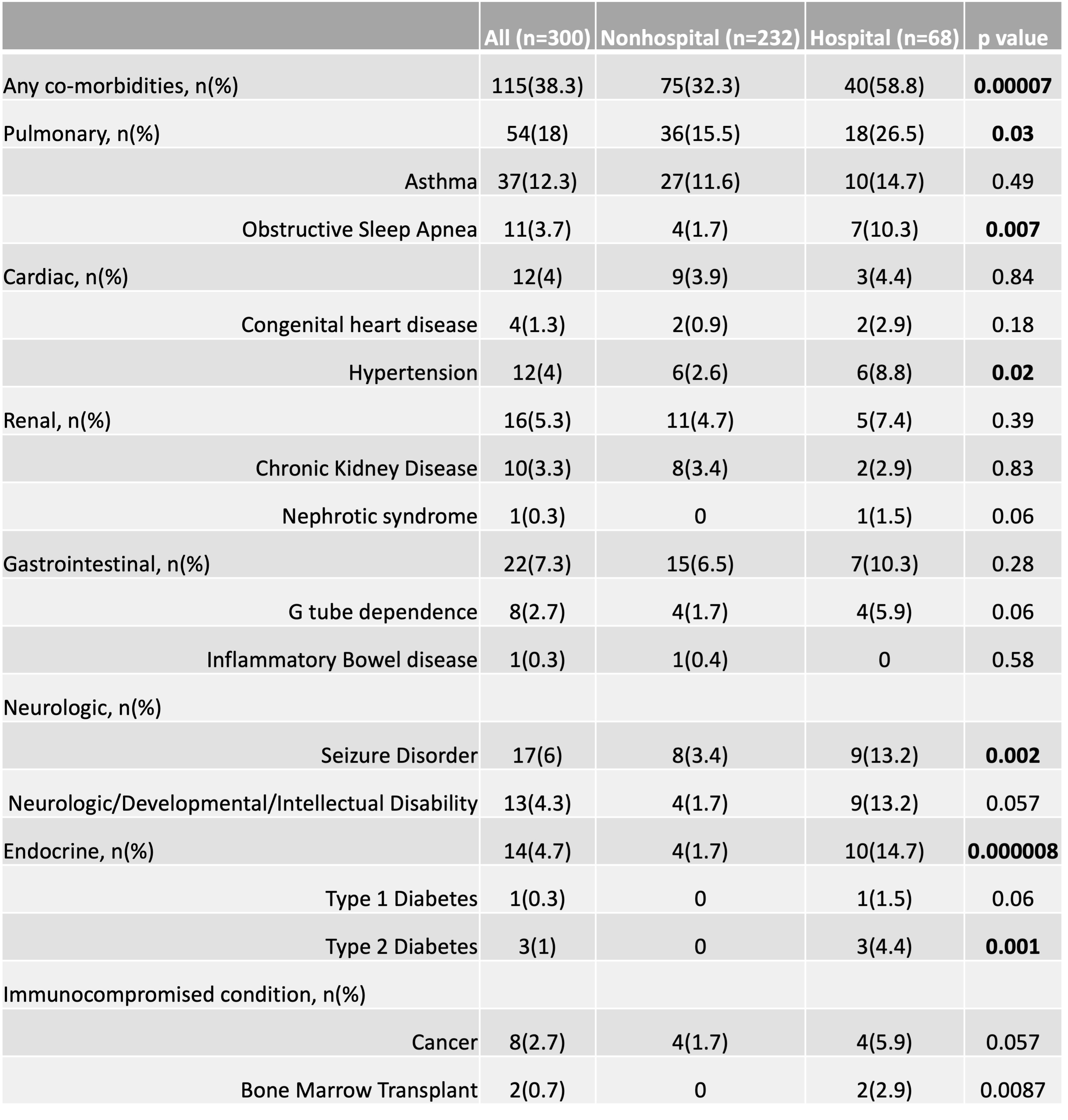
Objective: To determine the risk factors for hospitalization and critical disease due to COVID-19 in pediatric patients.
Design/Methods: We conducted a case control study of 300 patients with COVID-19 from July 1 – August 14, 2020. Two distinct outcomes were evaluated. The first categorized individuals hospitalized with symptomatic COVID-19 (Hospital) vs. individuals with COVID-19 not hospitalized or hospitalized with asymptomatic COVID-19 (Nonhospital). The second categorized individuals who required critical care (ICU) vs. individuals who did not require critical care (Floor). Demographics, medical co-morbidities, and symptoms at presentation were compared. Univariable analysis was done utilizing the Mann Whitney U test or the chi square test.
Results: Of 300 children, 68 (22.6%) were hospitalized and symptomatic. The Hospital group trended towards being older (6.5 vs 9.9 years, p=0.16) and more likely to be African American (25% vs 13.3%, p=0.03) compared to the Nonhospital group. The Hospital group was more likely to have any comorbidity (58.8% vs 32.3%, p < 0.0001), including diabetes mellitus (14.7% vs 1.7%, p=0.001), seizure disorder (13.2% vs 3.4%, p=0.002), hypertension (8.8% vs 2.6%, p=0.02), sickle cell disease (5.9% vs 0.4%, p=0.002), and bone marrow transplant (2.9% vs 0%, p=0.008). Nausea/vomiting (35.3% vs. 20.3%, p=0.01) and abdominal pain (23.5% vs 10.8%, p=0.07) were more common in the Hospital group, while rhinorrhea (7.4% vs. 17.7%, p=0.03) was more common in the Nonhospital group. The ICU group was more likely to have any comorbidity (82.4% vs 51%, p=0.02), including seizure disorder (35% vs 6%, p=0.001), obstructive sleep apnea (OSA) (29.4% vs 3.9%, p=0.002), gastrostomy tube dependence (23.5% vs 0%, p < 0.001), and neurological disability (29.4% vs 7.8%, p=0.02) than the Floor group. Shortness of breath (SOB) (47% vs 6%, p < 0.0001) and diarrhea (35% vs 6%, p=0.001) were more common among the ICU group.Conclusion(s): Children who required admission with symptomatic COVID-19 infection were more likely to have chronic medical conditions. Children who required critical care were more likely to have seizure disorder and OSA. Gastrointestinal complaints and SOB were more common symptoms in severe COVID-19. Larger studies are required to confirm the risk factors of severe/critical COVID-19 disease that we found among children.
Table 1: Demographic Characteristics
.jpg)
Table 2: Co-morbidities in Nonhospital and Hospital Groups