Social Media & Technology
Category: Abstract Submission
Social Media & Technology I
547 - Feasibility of the Virtual Reality (VR)-based Pediatric Display Enhanced Testing for Cognitive Impairment (PeDETECT) Concussion tool to assess concussion in the pediatric emergency department (ED)
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 547
Publication Number: 547.245
Publication Number: 547.245
Rob Grell, Emory University School of Medicine, Decatur, GA, United States; Michelle LaPlaca, Georgia Institute of Technology / Emory University, Atlanta, GA, United States; David W. Wright, Emory University School of Medicine, Atlanta, GA, United States; Laura S. Blackwell, Children's Healthcare of Atlanta, Atlanta, GA, United States; Andrew Reisner, Emory University School of Medicine, Atlanta, GA, United States; Austin P. Yu, Albany Medical College, Albany, NY, United States; Naina Murthy, Children's Healthcare of Atlanta, Atlanta, GA, United States; Maureen Nsofor, Emory University School of Medicine, Decatur, GA, United States; Justin Leonel Santos, Emory University School of Medicine, Atlanta, GA, United States; Avnee Sarnaik, Children's Healthcare of Atlanta, Marietta, GA, United States; Megha Kulkarni, Georgia Institute of Technology, Bloomfield Hills, MI, United States; Emma Waldon, Georgetown university, washington, DC, United States; Dylan P. Hurley, Children's Healthcare of Atlanta, Decatur, GA, United States; Farzina Zafar, Children’s healthcare of atlanta, Lilburn, GA, United States; Patricia A. Bush, Emory/Children's Healthcare of Atlanta, Atlanta, GA, United States; Harold Simon, Emory University School of Medicine and Children's healthcare of Atlanta, atlanta, GA, United States; Claudia R. Morris, Emory University School of Medicine, Atlanta, GA, United States

Rob Grell, MD (he/him/his)
Fellow, Pediatric Emergency Medicine
Emory University School of Medicine
Decatur, Georgia, United States
Presenting Author(s)
Background: Concussion impacts over half a million pediatric patients annually and can lead to significant and protracted symptoms in up to 30% of patients. Early recognition and intervention have been shown to improve long term outcomes, but upwards of 60% of patients with concussions leave the ED without a proper diagnosis. Concussion is a clinical diagnosis that requires interrogation of multiple domains of brain function. Lengthy testing protocols and subjectivity hampers current assessment in the ED environment. Multimodal testing within a self-contained, immersive virtual environment has potential to provide an objective diagnostic aide for austere settings such as the busy ED. The PeDETECT system is a comprehensive and multimodal portable tool that utilizes VR to measure concussion-relevant brain function.
Objective: To assess the feasibility of the PeDETECT VR device for assessment of pediatric concussion in the pediatric ED setting.
Design/Methods: A prospective feasibility study was designed with a pre-enrollment feasibility that was defined as ≥80% completion of the PeDETECT VR module. The main objective was to compare the completion percentage of the PeDETECT VR test in the pediatric ED patients presenting with head-injury vs control subjects without head injury. Secondary outcomes included user subjective feedback on the device, complex choice reaction time, simple reaction time, patient satisfaction, and ED length of stay. Mean±SD, unpaired student t-test, and chi-square were used for statistical analysis.
Results: To date, 144 patients have been approached, of which 83 were consented and 79 patients (55%) were enrolled (18 head injury, 61 Controls). Mean age of the group was 12±2 years and 54% were male (Table 1). There were no differences in age or gender between cases and controls. Rate of completion was 87% overall with no completion difference between head injury vs control groups (89% vs 87%, p=0.81 respectively). There was a statistically significant difference for gender between males (n= 43) and females (n=36) found for completion rates in combined groups (95% vs 78%, p< 0.02). Secondary analyses of patient responses within the PeDETECT tests are ongoing.Conclusion(s): The data demonstrates feasibility of PeDETECT use in the pediatric ED setting, supported by a completion rate of ≥80%. Headset use was not limited by head-injury or age. Gender differences were identified for rate of completion. As enrollment is ongoing, future analysis will include secondary outcomes, including the measured reaction time, which could be useful in demonstrating validity for objective concussion diagnosis.
Rob Grell CV 2022Grell.CV.Update.07-10-19.docx (1).pdf
Figure 1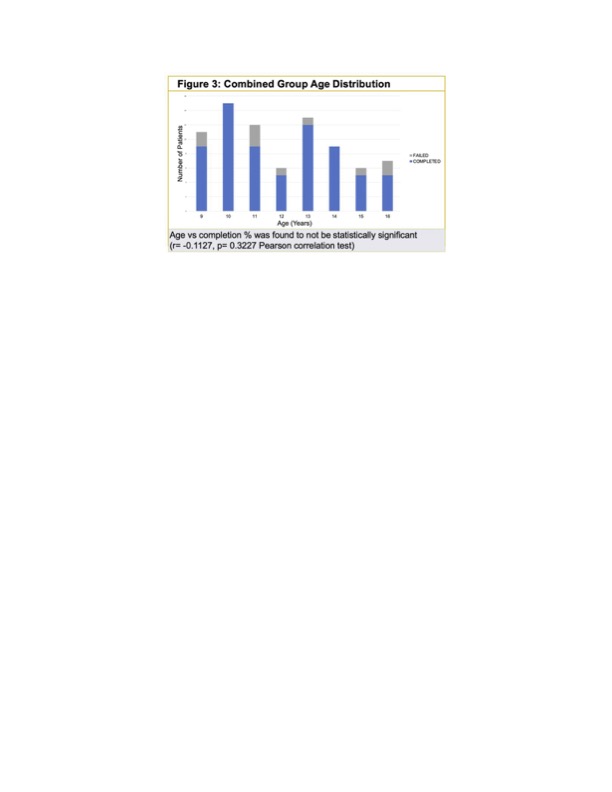 PeDETECT age-grouped completion rates
PeDETECT age-grouped completion rates
Objective: To assess the feasibility of the PeDETECT VR device for assessment of pediatric concussion in the pediatric ED setting.
Design/Methods: A prospective feasibility study was designed with a pre-enrollment feasibility that was defined as ≥80% completion of the PeDETECT VR module. The main objective was to compare the completion percentage of the PeDETECT VR test in the pediatric ED patients presenting with head-injury vs control subjects without head injury. Secondary outcomes included user subjective feedback on the device, complex choice reaction time, simple reaction time, patient satisfaction, and ED length of stay. Mean±SD, unpaired student t-test, and chi-square were used for statistical analysis.
Results: To date, 144 patients have been approached, of which 83 were consented and 79 patients (55%) were enrolled (18 head injury, 61 Controls). Mean age of the group was 12±2 years and 54% were male (Table 1). There were no differences in age or gender between cases and controls. Rate of completion was 87% overall with no completion difference between head injury vs control groups (89% vs 87%, p=0.81 respectively). There was a statistically significant difference for gender between males (n= 43) and females (n=36) found for completion rates in combined groups (95% vs 78%, p< 0.02). Secondary analyses of patient responses within the PeDETECT tests are ongoing.Conclusion(s): The data demonstrates feasibility of PeDETECT use in the pediatric ED setting, supported by a completion rate of ≥80%. Headset use was not limited by head-injury or age. Gender differences were identified for rate of completion. As enrollment is ongoing, future analysis will include secondary outcomes, including the measured reaction time, which could be useful in demonstrating validity for objective concussion diagnosis.
Rob Grell CV 2022Grell.CV.Update.07-10-19.docx (1).pdf
Figure 1
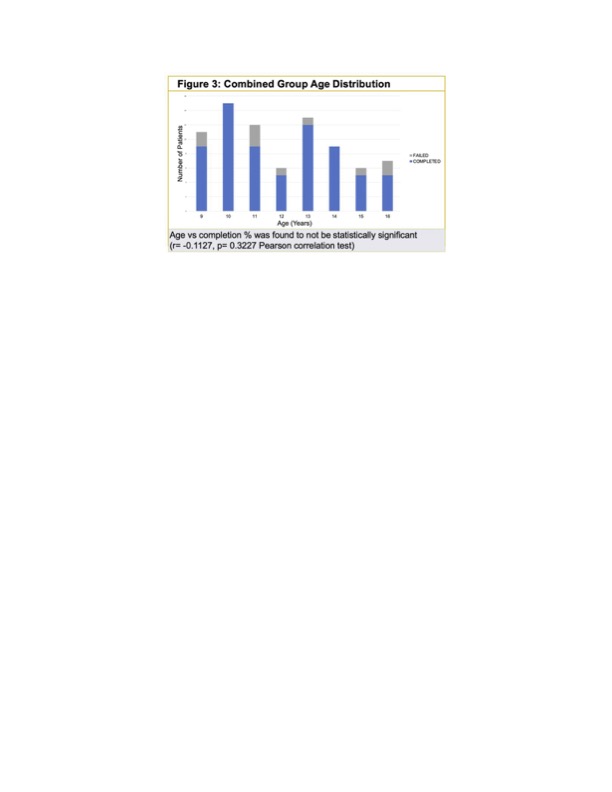 PeDETECT age-grouped completion rates
PeDETECT age-grouped completion rates