Back
Hospital Medicine: Clinical
Category: Abstract Submission
Hospital Medicine: Clinical - Infectious Disease NOS
306 - Antibiotic Use and Outcomes Among Children Hospitalized with Suspected Pneumonia
Saturday, April 23, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 306
Publication Number: 306.213
Publication Number: 306.213
Jillian M. Cotter, University of Colorado School of Medicine, Aurora, CO, United States; Todd A. Florin, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; ANGELA MOSS, ACCORDS, University of Colorado, Aurora, CO, United States; Krithika Suresh, Colorado School of Public Health, Denver, CO, United States; Sriram Ramgopal, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Nidhya Navanandan, University of Colorado School of Medicine, Aurora, CO, United States; Richard M. Ruddy, University of Cincinnati College of Medicine, Cincinnati, OH, United States; Samir S. Shah, Journal of Hospital Medicine, Cincinnati, OH, United States; allison kempe, University of Colorado School of Medicine, denver, CO, United States; Lilliam Ambroggio, Children's Hospital Colorado, Aurora, CO, United States

Jillian Cotter, MD, MSCS
Pediatric Hospitalist
University of Colorado / Children's Hospital Colorado
Aurora, Colorado, United States
Presenting Author(s)
Background: Although viral etiologies predominate, antibiotics are frequently prescribed for community-acquired pneumonia (CAP). Prior work among outpatients with suspected CAP demonstrated no difference in treatment failure between those treated with and without antibiotics.
Objective: We sought to evaluate the association between antibiotic use and outcomes among children hospitalized with suspected CAP.
Design/Methods: We performed a prospective cohort study of children 3 months to 18 years hospitalized for suspected CAP, excluding those initially admitted to an intensive care unit (ICU). The exposure was receipt of antibiotics in the emergency department (ED). The primary outcome was length of stay (LOS). Secondary outcomes included 1) escalated care in the inpatient setting (death, ICU transfer, non-invasive positive-pressure or mechanical ventilation, high flow oxygen, chest drainage, or worsening chest imaging), 2) treatment failure after discharge (30-day respiratory-related readmission, 30-day ED revisit with change in antibiotics, change/addition of antibiotics or new diagnosis of CAP per family report), 3) 30-day respiratory-related ED revisit, and 4) family-reported quality-of-life measures (e.g., symptom duration, days until return to normal activity) collected 7-15 days after discharge. To limit potential bias attributable to treatment selection between children who did and did not receive antibiotics, we performed inverse propensity weighted regression analyses with covariates (listed in Table 2 footnote).
Results: Among 523 children, 290 (55%) received antibiotics in the ED (Table 1). In propensity weighted analysis, there was no difference in LOS between children who received antibiotics and those who did not (effect estimate 0.98 [95% CI 0.88,1.10]; Table 2). There were no differences in the proportion of children with escalated care (5% with antibiotics vs 4% without), treatment failure post-discharge (6% vs 5%), or ED revisits (5% vs 4%). Among those who completed the follow-up survey (n=373, 71%), there was a 0.63-fold decrease (95% CI 0.49,0.80) in the mean number of days with fever post-discharge for children who received antibiotics, but no significant differences in the other quality-of-life measures (Table 3).Conclusion(s): In this propensity-weighted analysis of children hospitalized with suspected CAP, there were no clinically significant differences in most in-hospital or post-discharge outcomes between those who did and did not receive antibiotics. Our findings suggest that potential opportunities exist to safely treat more children hospitalized with suspected CAP without antibiotics.
Table 1. Patient Demographics and Clinical Characteristics by Receipt of ED Antibiotics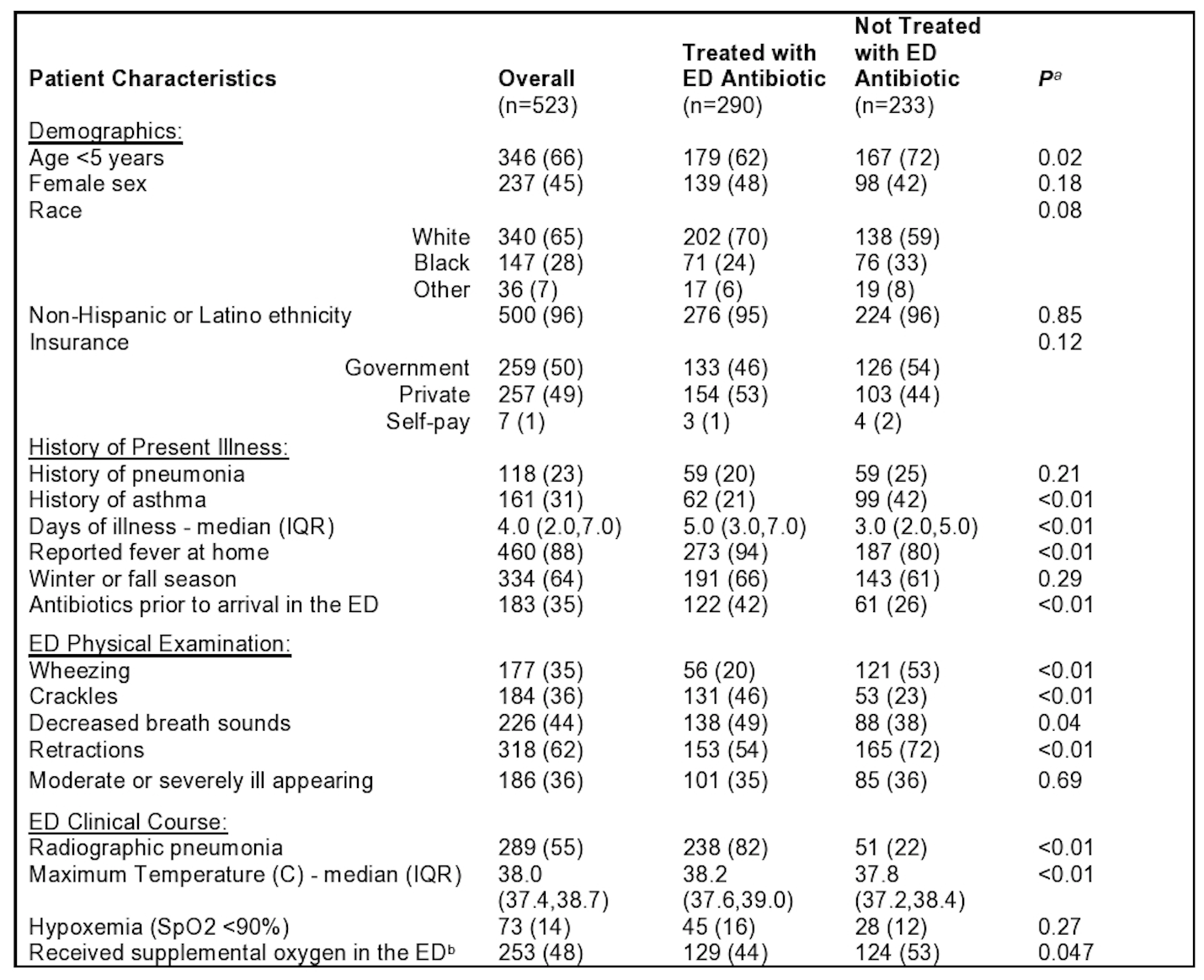 Values represent N(%) unless otherwise specified.
Values represent N(%) unless otherwise specified.
ED, emergency department
a Calculated using Wilcoxon Rank Sum test (for continuous variables) or Pearson’s chi-squared test (for categorical variables)
b Including low flow or heated high flow oxygen
Table 2. In-hospital and Post-Discharge Clinical Outcomes with Propensity Score Analysis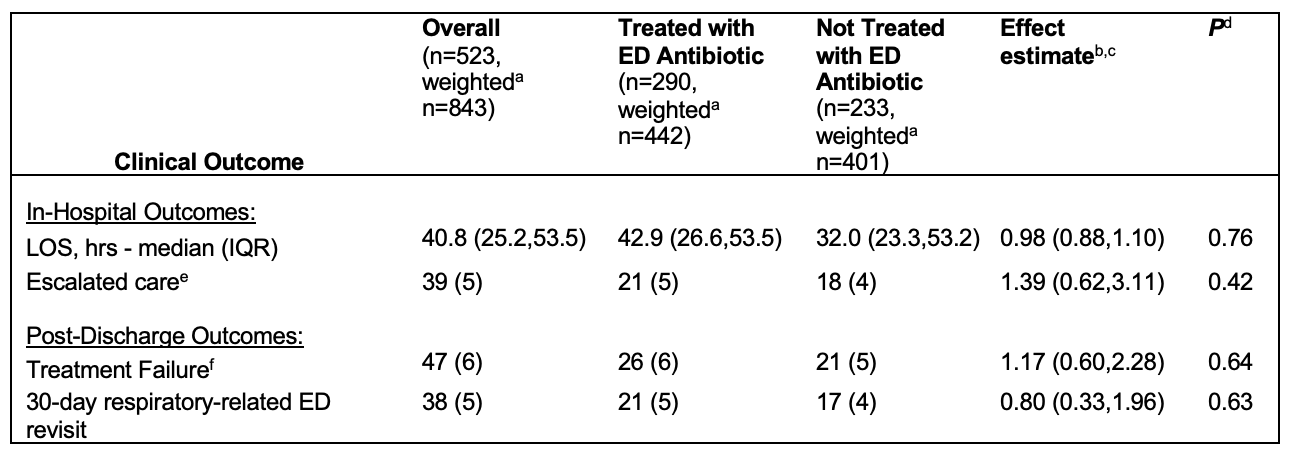 Values represent N(%) from weighted bivariable analysis unless otherwise stated.
Values represent N(%) from weighted bivariable analysis unless otherwise stated.
ED, emergency department; LOS, length of stay
a To improve treatment-control balance between groups, treated subjects with a low propensity for treatment and control subjects with high propensity for treatment are given more weight than other subjects. This results in an increased sample size to balance the two groups.
b Weighted logistic regression (for binary outcomes) with effect estimates as odds ratios and log gamma regression (for continuous LOS outcome) with effect interpreted as the relative increase in LOS in hours for those with antibiotics in the ED compared to those without antibiotics.
c Effects were calculate using the inverse probability of receiving treatment method and adjusted for the following covariates: gender, age, race, history of pneumonia, history of asthma/RAD, winter/fall season, fever at home, days of illness, ED antibiotics prior to arrival in the ED, decreased breath sounds, crackles, wheeze, retractions, and moderate/severe ill appearance based on ED physical examination, maximum temperature in the ED, hypoxemia in the ED, presence of radiographic pneumonia, and receipt of supplemental oxygen in the ED
d After adjusting p-values for multiple comparisons using Hochberg p-value adjustment, there was no change in statistical significance
e Escalated care in the inpatient setting was a composite outcome defined as any of the following 1) pneumonia-related death, 2) transferred to ICU, 3) received high flow oxygen, non-invasive positive-pressure or mechanical ventilation, 4) received chest drainage, or 5) worsening findings on repeat chest imaging
f Post-discharge treatment failure was a composite outcome defined as 1) 30-day respiratory-related readmission, 2) 30-day ED revisit with change in antibiotics, 3) change or addition of antibiotics per family report, or 4) new diagnosis of CAP per family report
Objective: We sought to evaluate the association between antibiotic use and outcomes among children hospitalized with suspected CAP.
Design/Methods: We performed a prospective cohort study of children 3 months to 18 years hospitalized for suspected CAP, excluding those initially admitted to an intensive care unit (ICU). The exposure was receipt of antibiotics in the emergency department (ED). The primary outcome was length of stay (LOS). Secondary outcomes included 1) escalated care in the inpatient setting (death, ICU transfer, non-invasive positive-pressure or mechanical ventilation, high flow oxygen, chest drainage, or worsening chest imaging), 2) treatment failure after discharge (30-day respiratory-related readmission, 30-day ED revisit with change in antibiotics, change/addition of antibiotics or new diagnosis of CAP per family report), 3) 30-day respiratory-related ED revisit, and 4) family-reported quality-of-life measures (e.g., symptom duration, days until return to normal activity) collected 7-15 days after discharge. To limit potential bias attributable to treatment selection between children who did and did not receive antibiotics, we performed inverse propensity weighted regression analyses with covariates (listed in Table 2 footnote).
Results: Among 523 children, 290 (55%) received antibiotics in the ED (Table 1). In propensity weighted analysis, there was no difference in LOS between children who received antibiotics and those who did not (effect estimate 0.98 [95% CI 0.88,1.10]; Table 2). There were no differences in the proportion of children with escalated care (5% with antibiotics vs 4% without), treatment failure post-discharge (6% vs 5%), or ED revisits (5% vs 4%). Among those who completed the follow-up survey (n=373, 71%), there was a 0.63-fold decrease (95% CI 0.49,0.80) in the mean number of days with fever post-discharge for children who received antibiotics, but no significant differences in the other quality-of-life measures (Table 3).Conclusion(s): In this propensity-weighted analysis of children hospitalized with suspected CAP, there were no clinically significant differences in most in-hospital or post-discharge outcomes between those who did and did not receive antibiotics. Our findings suggest that potential opportunities exist to safely treat more children hospitalized with suspected CAP without antibiotics.
Table 1. Patient Demographics and Clinical Characteristics by Receipt of ED Antibiotics
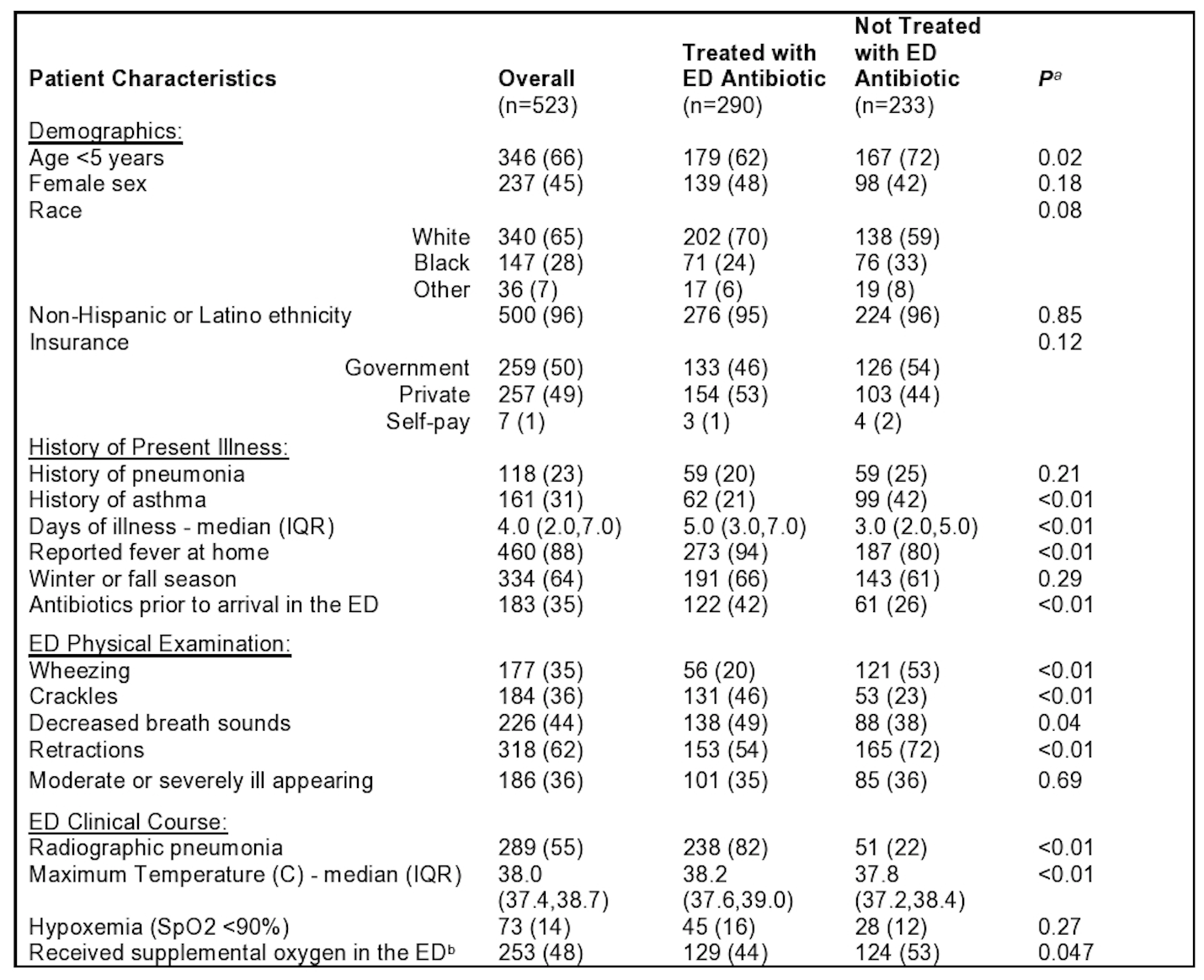 Values represent N(%) unless otherwise specified.
Values represent N(%) unless otherwise specified.ED, emergency department
a Calculated using Wilcoxon Rank Sum test (for continuous variables) or Pearson’s chi-squared test (for categorical variables)
b Including low flow or heated high flow oxygen
Table 2. In-hospital and Post-Discharge Clinical Outcomes with Propensity Score Analysis
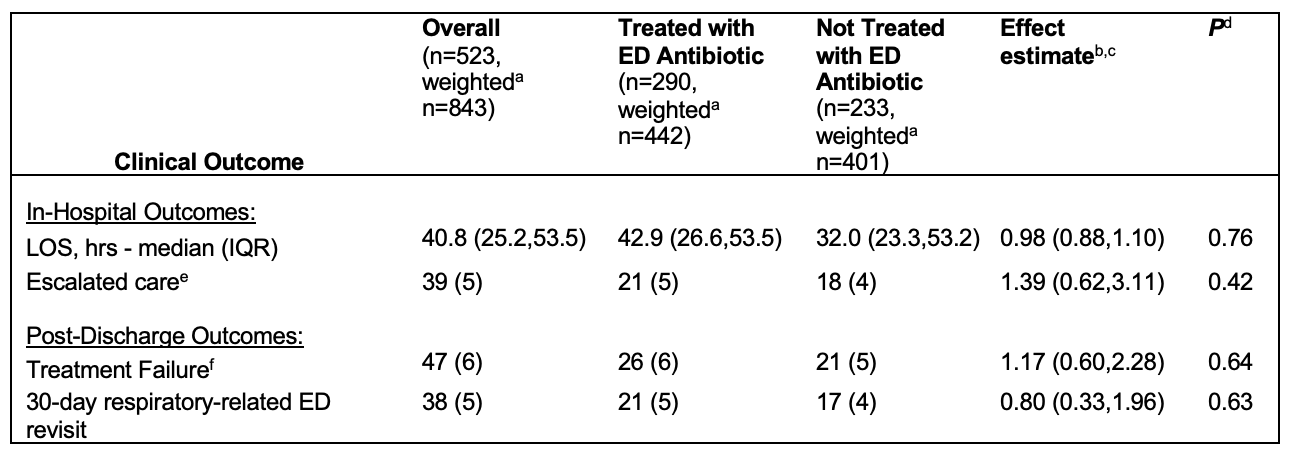 Values represent N(%) from weighted bivariable analysis unless otherwise stated.
Values represent N(%) from weighted bivariable analysis unless otherwise stated. ED, emergency department; LOS, length of stay
a To improve treatment-control balance between groups, treated subjects with a low propensity for treatment and control subjects with high propensity for treatment are given more weight than other subjects. This results in an increased sample size to balance the two groups.
b Weighted logistic regression (for binary outcomes) with effect estimates as odds ratios and log gamma regression (for continuous LOS outcome) with effect interpreted as the relative increase in LOS in hours for those with antibiotics in the ED compared to those without antibiotics.
c Effects were calculate using the inverse probability of receiving treatment method and adjusted for the following covariates: gender, age, race, history of pneumonia, history of asthma/RAD, winter/fall season, fever at home, days of illness, ED antibiotics prior to arrival in the ED, decreased breath sounds, crackles, wheeze, retractions, and moderate/severe ill appearance based on ED physical examination, maximum temperature in the ED, hypoxemia in the ED, presence of radiographic pneumonia, and receipt of supplemental oxygen in the ED
d After adjusting p-values for multiple comparisons using Hochberg p-value adjustment, there was no change in statistical significance
e Escalated care in the inpatient setting was a composite outcome defined as any of the following 1) pneumonia-related death, 2) transferred to ICU, 3) received high flow oxygen, non-invasive positive-pressure or mechanical ventilation, 4) received chest drainage, or 5) worsening findings on repeat chest imaging
f Post-discharge treatment failure was a composite outcome defined as 1) 30-day respiratory-related readmission, 2) 30-day ED revisit with change in antibiotics, 3) change or addition of antibiotics per family report, or 4) new diagnosis of CAP per family report
