Hospital Medicine: Clinical
Category: Abstract Submission
Hospital Medicine: Clinical - Infectious Disease NOS
307 - Assessing appropriateness, acceptability, and feasibility of care recommendations for children with neurologic impairment hospitalized with pneumonia
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 307
Publication Number: 307.213
Publication Number: 307.213
Abigail E. Woolums, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Dan Benscoter, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Scott R. Callahan, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; David Haslam, Cincinnati Children's Hospital, Cincinnati, OH, United States; Abigail M. Musial, Cincinnati Children's Hospital Medical Center, CINCINNATI, OH, United States; Samir S. Shah, Journal of Hospital Medicine, Cincinnati, OH, United States; Rebecca Steuart, Medical College of Wisconsin, Milwaukee, WI, United States; Christine White, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Joanna Thomson, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Michael Rafferty, cchmc, Cincinnati, OH, United States

Abigail E. Woolums
Medical Student
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Recommendations for management of pediatric pneumonia exclude children with neurologic impairment. Thus, there is wide variation in their care and outcomes. In prior work, a national multidisciplinary expert panel reviewed existing evidence in the development of care recommendations for diagnostic testing, antimicrobial use, airway clearance, and discharge in children with NI hospitalized with pneumonia.
Objective: To assess the acceptability, appropriateness, and feasibility of care recommendations to prioritize implementation.
Design/Methods: Our local study team prioritized the care recommendations developed by the national expert panel for consideration of implementation. In a cross-sectional single center survey administered via REDCap, clinical team members across several divisions who care for children with NI hospitalized with pneumonia rated the acceptability, appropriateness, and feasibility of high priority recommendations. Ratings were made on a scale of 1 (completely disagree) to 5 (completely agree) using questions from the Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM). Mean scores (with standard deviation) for acceptability, appropriateness, and feasibility were calculated for each recommendation. Ratings were also compared across divisions using ANOVA to identify potential differences across specialties.
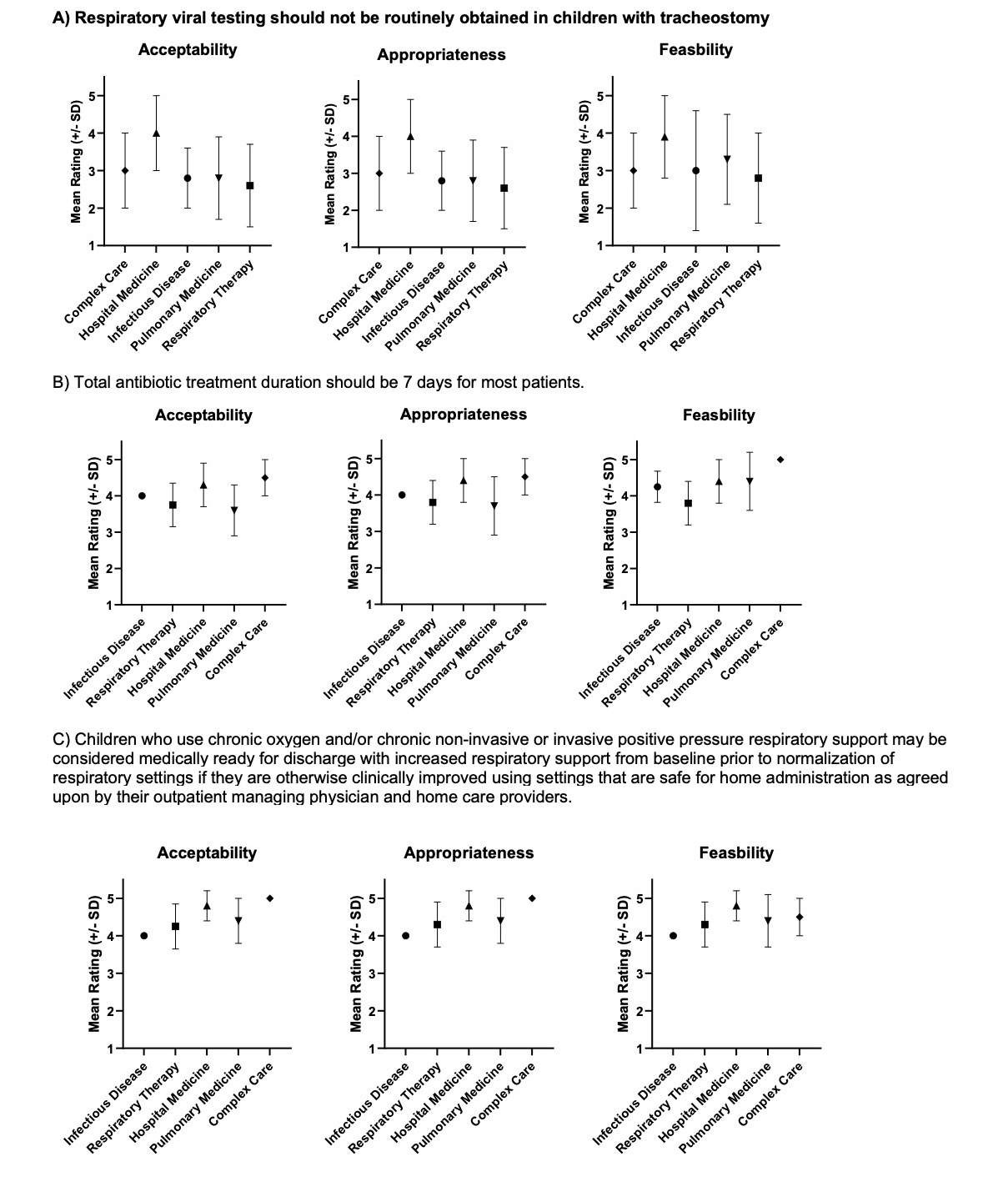
Results: Healthcare professionals in hospital medicine (n=24/29), respiratory therapy (n=21), pulmonary medicine (n=16/64), infectious disease (n=4/17), and complex care (n=3/5), rated all 15 care recommendations as highly acceptable, appropriate, and feasible for implementation by the majority of responders (Table 1). There was little difference between ratings of acceptability, appropriateness, and feasibility for individual recommendations. However, professionals in hospital medicine and complex care were generally more likely to find recommendations limiting testing, treatment, and discharge criteria more acceptable, appropriate, and feasible than other divisions (Figure 1).Conclusion(s): Though there are differences across divisions in ratings, prioritized care recommendations from a national expert panel for management of pneumonia in hospitalized children with NI were rated as acceptable, appropriate, and feasible for implementation into clinical care. As we begin implementation efforts, incorporating family perspectives and study of patient outcomes will be critical.
Table 1. Mean rating (± Standard Deviation) of Acceptability, Appropriateness, and Feasibility of Implementing Care Recommendations. (5=completely agree, 1=completely disagree).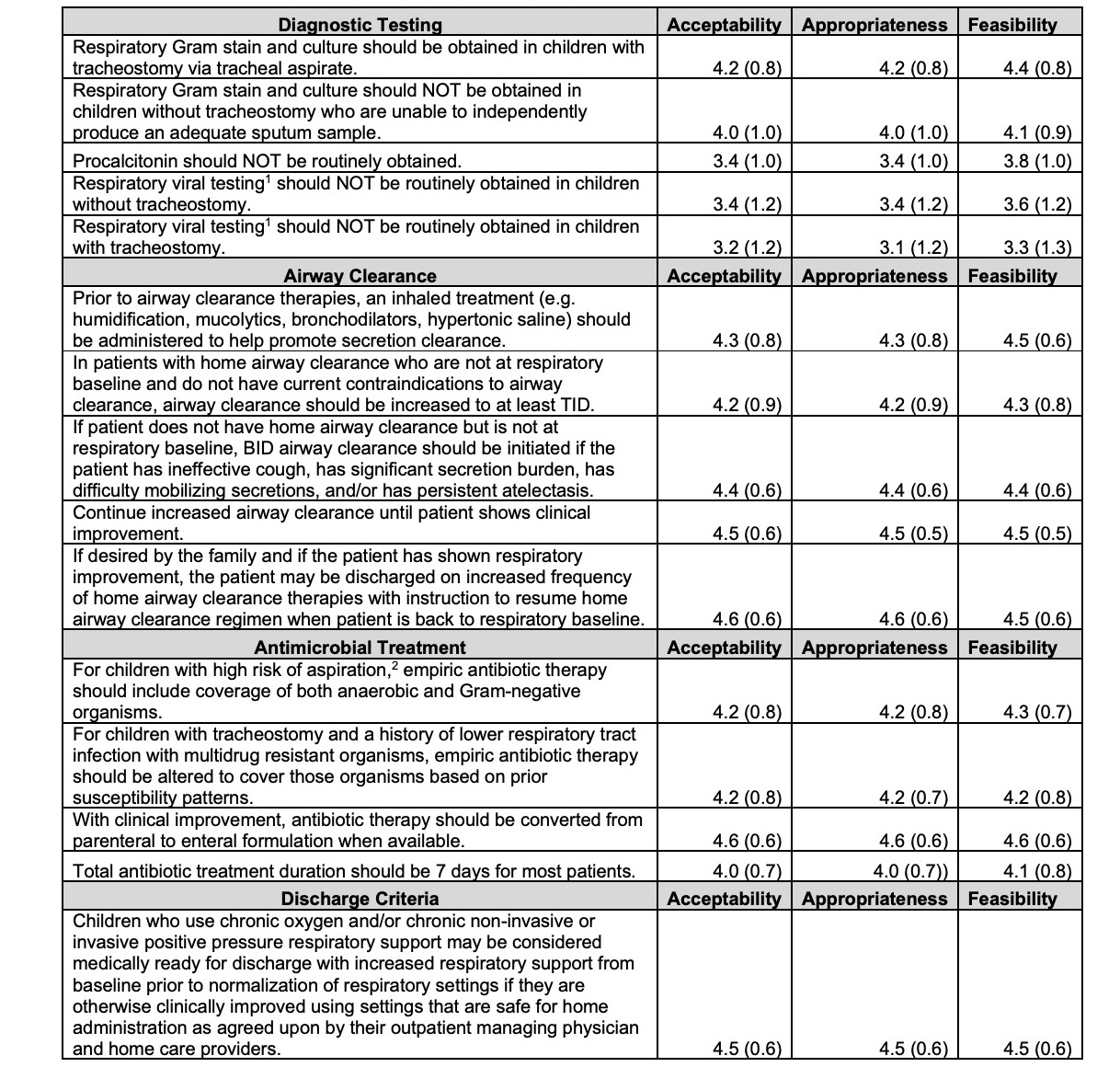 1. Exclusive of influenza and SARS-COV-2 testing.
1. Exclusive of influenza and SARS-COV-2 testing.
2. As there is no standardized definition or diagnostic test that differentiates aspiration pneumonia from community acquired pneumonia, clinicians must rely on diagnostic reasoning skill (including consideration of a patient’s complexities including known risks for aspiration as well as their clinical presentation and history of prior pneumonia illnesses) to determine if a patient is at high or low risk for aspiration pneumonia.
Figure 1. Comparison of Mean Ratings (± standard deviation [SD]) by Division (p-value < 0.05 via ANOVA)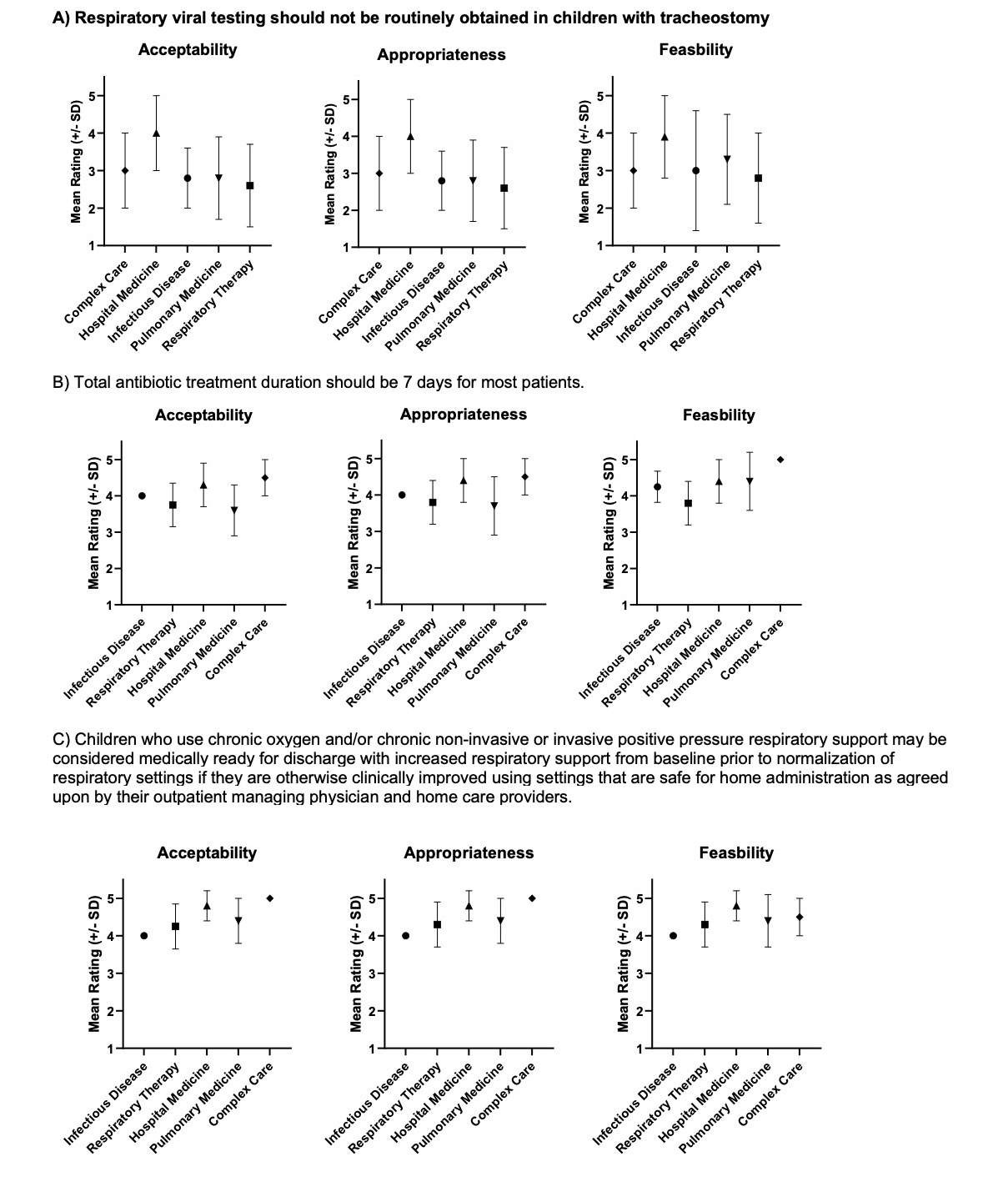
Objective: To assess the acceptability, appropriateness, and feasibility of care recommendations to prioritize implementation.
Design/Methods: Our local study team prioritized the care recommendations developed by the national expert panel for consideration of implementation. In a cross-sectional single center survey administered via REDCap, clinical team members across several divisions who care for children with NI hospitalized with pneumonia rated the acceptability, appropriateness, and feasibility of high priority recommendations. Ratings were made on a scale of 1 (completely disagree) to 5 (completely agree) using questions from the Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM). Mean scores (with standard deviation) for acceptability, appropriateness, and feasibility were calculated for each recommendation. Ratings were also compared across divisions using ANOVA to identify potential differences across specialties.
Results: Healthcare professionals in hospital medicine (n=24/29), respiratory therapy (n=21), pulmonary medicine (n=16/64), infectious disease (n=4/17), and complex care (n=3/5), rated all 15 care recommendations as highly acceptable, appropriate, and feasible for implementation by the majority of responders (Table 1). There was little difference between ratings of acceptability, appropriateness, and feasibility for individual recommendations. However, professionals in hospital medicine and complex care were generally more likely to find recommendations limiting testing, treatment, and discharge criteria more acceptable, appropriate, and feasible than other divisions (Figure 1).Conclusion(s): Though there are differences across divisions in ratings, prioritized care recommendations from a national expert panel for management of pneumonia in hospitalized children with NI were rated as acceptable, appropriate, and feasible for implementation into clinical care. As we begin implementation efforts, incorporating family perspectives and study of patient outcomes will be critical.
Table 1. Mean rating (± Standard Deviation) of Acceptability, Appropriateness, and Feasibility of Implementing Care Recommendations. (5=completely agree, 1=completely disagree).
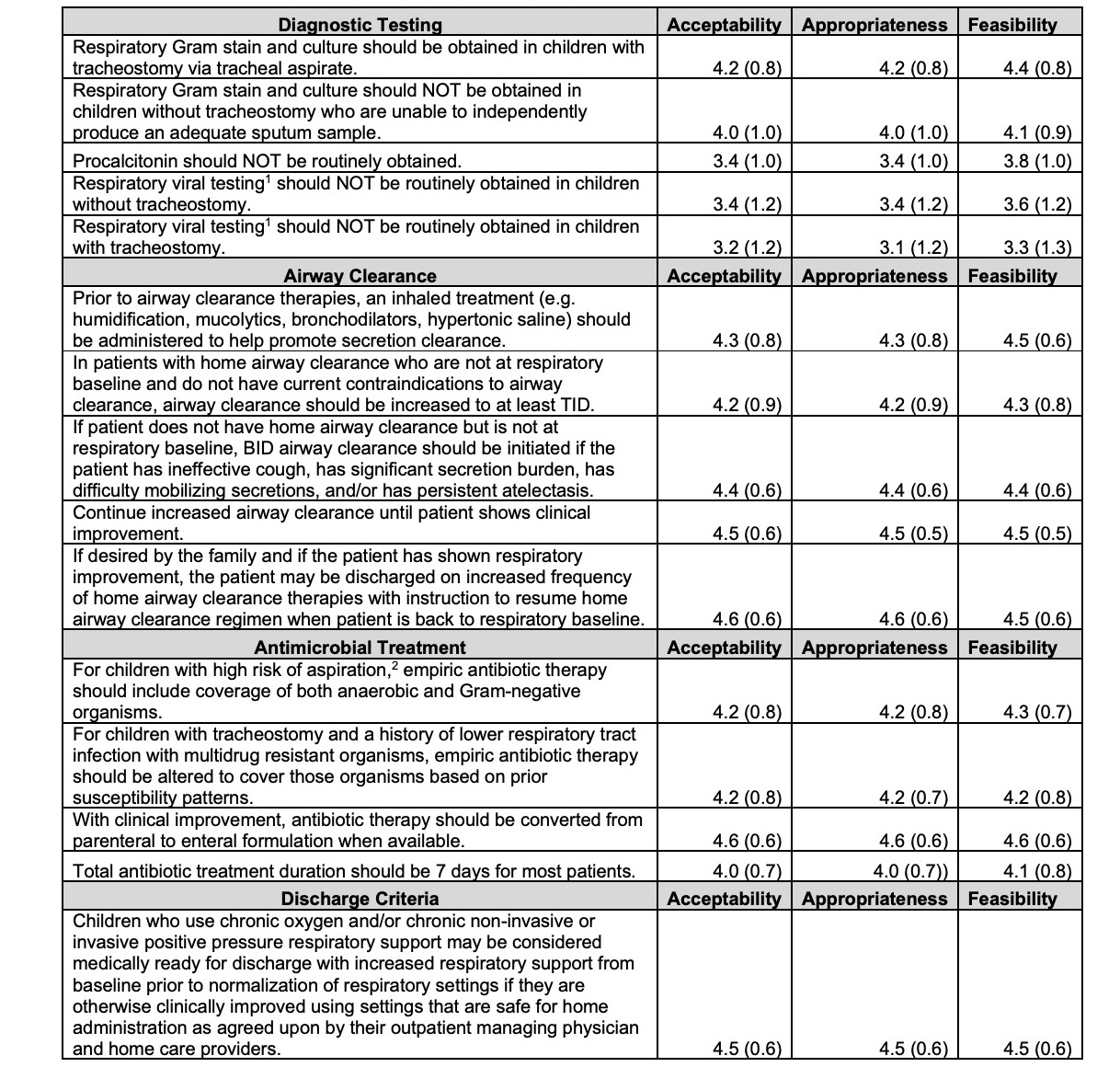 1. Exclusive of influenza and SARS-COV-2 testing.
1. Exclusive of influenza and SARS-COV-2 testing.2. As there is no standardized definition or diagnostic test that differentiates aspiration pneumonia from community acquired pneumonia, clinicians must rely on diagnostic reasoning skill (including consideration of a patient’s complexities including known risks for aspiration as well as their clinical presentation and history of prior pneumonia illnesses) to determine if a patient is at high or low risk for aspiration pneumonia.
Figure 1. Comparison of Mean Ratings (± standard deviation [SD]) by Division (p-value < 0.05 via ANOVA)