Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement II: Neurology and Infection
228 - Risk Stratification to Support Antibiotic Stewardship and Breastfeeding Exclusivity in a Military Treatment Facility: A Quality Improvement Project
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 228
Publication Number: 228.127
Publication Number: 228.127
Lisa J. Mitchell, Carl R. Darnall Army Medical Center, Harker Heights, TX, United States; Bethany Gardner, US Army MEDCOM, Temple, TX, United States
- LM
Lisa J. Mitchell, DO
Neonatologist
Carl R. Darnall Army Medical Center
Harker Heights, Texas, United States
Presenting Author(s)
Background: Within our mid-size military treatment facility (~2000 births/year), all infants exposed to chorioamnionitis or inadequately treated GBS were immediately separated from their mothers after birth for IV access and antibiotic initiation regardless of clinical status. If clinically well, infants then remained with their mothers while receiving 48 hours of antibiotic prophylaxis. Our historical data demonstrated low rates of both blood culture-proven sepsis and exclusive breastfeeding in treated infants.
Objective: To reduce unnecessary antibiotic exposure, we implemented use of the Neonatal Early-Onset Sepsis (EOS) Calculator and a 36-hour antibiotic duration. We hypothesized that avoiding infant-mother separation during the crucial Golden Hour would improve breastfeeding rates at discharge.
Design/Methods: We used the Model for Improvement. Participants were inborn infants ≥35 weeks of gestation without congenital anomalies. Our multidisciplinary team included physicians, nursing leaders, and nursing champions from the Mother-Baby and Labor & Delivery units. Key diagram is shown (Fig. 1). All inborn infants ≥35 weeks of gestation were risk-stratified and calculator instructions followed. We used PDSA cycles to educate staff, monitor for sepsis, and improve adherence to calculator use. Our PDSA cycles included initial staff education, nursing note template creation in the EMR, and then significant revisions to the note template after nursing feedback was received, with improvement in compliance. Our institutional practice already included vital signs every 4 hours for all infants. We added newborn rapid assessments to preexisting hourly nursing rounds.
Results: In the 12 months after calculator implementation, we saw a 65% decrease in antibiotic treatment for chorioamnionitis or inadequate GBS prophylaxis (Fig. 2) with a concomitant 49% increase in exclusive breastfeeding at discharge in the same population (Fig. 3). There were no readmissions to our institution for culture-proven sepsis within 14 days of discharge. Only 1 blood culture was positive, drawn from an infant exposed to chorioamnionitis who immediately risk-stratified at birth to receiving antibiotics based on clinical condition.Conclusion(s): Multidisciplinary team-led implementation of the EOS calculator and reduced antibiotic duration safely reduced antibiotic use in well-appearing infants with chorioamnionitis and GBS exposure, and correlated with dramatically improved rates of breastfeeding. Our results show that keeping mothers and infants together during the Golden Hour is key to establishing effective breastfeeding.
Fig. 1: Key Driver Diagram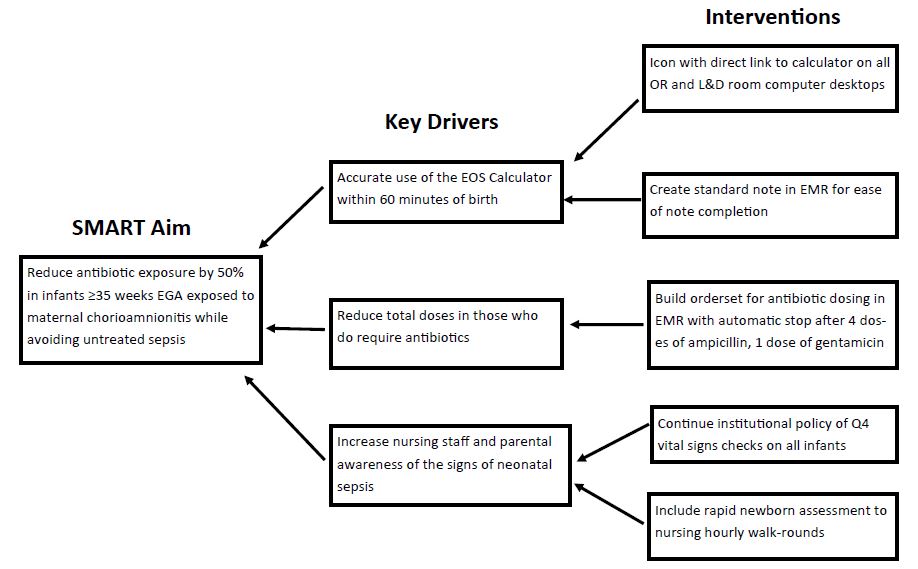
Fig. 2: Rate of Antibiotic Treatment in Infants Exposed to Chorioamnionitis or Inadequate GBS Prophylaxis.jpg)
Objective: To reduce unnecessary antibiotic exposure, we implemented use of the Neonatal Early-Onset Sepsis (EOS) Calculator and a 36-hour antibiotic duration. We hypothesized that avoiding infant-mother separation during the crucial Golden Hour would improve breastfeeding rates at discharge.
Design/Methods: We used the Model for Improvement. Participants were inborn infants ≥35 weeks of gestation without congenital anomalies. Our multidisciplinary team included physicians, nursing leaders, and nursing champions from the Mother-Baby and Labor & Delivery units. Key diagram is shown (Fig. 1). All inborn infants ≥35 weeks of gestation were risk-stratified and calculator instructions followed. We used PDSA cycles to educate staff, monitor for sepsis, and improve adherence to calculator use. Our PDSA cycles included initial staff education, nursing note template creation in the EMR, and then significant revisions to the note template after nursing feedback was received, with improvement in compliance. Our institutional practice already included vital signs every 4 hours for all infants. We added newborn rapid assessments to preexisting hourly nursing rounds.
Results: In the 12 months after calculator implementation, we saw a 65% decrease in antibiotic treatment for chorioamnionitis or inadequate GBS prophylaxis (Fig. 2) with a concomitant 49% increase in exclusive breastfeeding at discharge in the same population (Fig. 3). There were no readmissions to our institution for culture-proven sepsis within 14 days of discharge. Only 1 blood culture was positive, drawn from an infant exposed to chorioamnionitis who immediately risk-stratified at birth to receiving antibiotics based on clinical condition.Conclusion(s): Multidisciplinary team-led implementation of the EOS calculator and reduced antibiotic duration safely reduced antibiotic use in well-appearing infants with chorioamnionitis and GBS exposure, and correlated with dramatically improved rates of breastfeeding. Our results show that keeping mothers and infants together during the Golden Hour is key to establishing effective breastfeeding.
Fig. 1: Key Driver Diagram
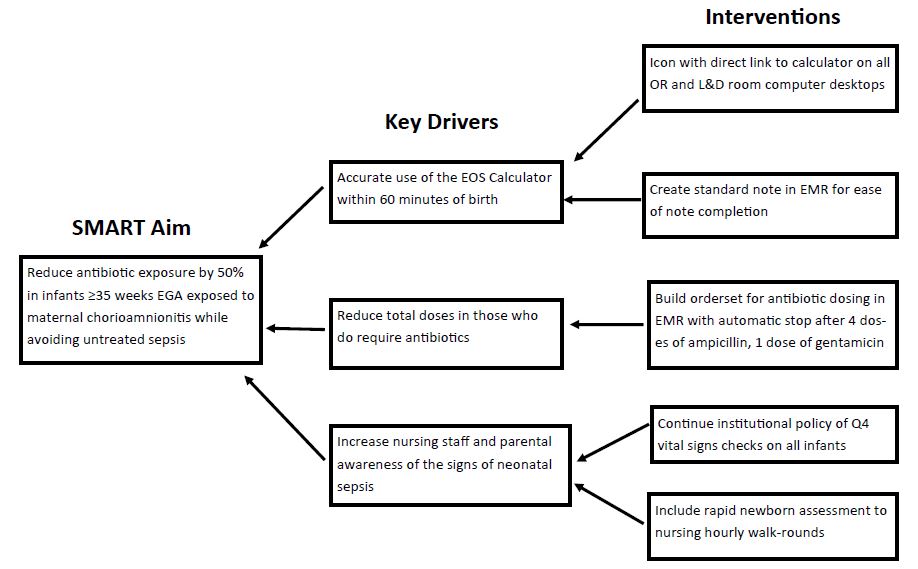
Fig. 2: Rate of Antibiotic Treatment in Infants Exposed to Chorioamnionitis or Inadequate GBS Prophylaxis
.jpg)
