Endocrinology: Thyroid
Category: Abstract Submission
Endocrinology I
529 - Screening for Delayed Thyroid Stimulating Hormone (TSH) Rise and Congenital Hypothyroidism in Very Low Birth Weight (VLBW) Infants.
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 529
Publication Number: 529.107
Publication Number: 529.107
Bret Nolan, UCI Medical Center, Orange, CA, United States; Cherry Uy, University of California, Irvine, School of Medicine, Orange, CA, United States; Lisa Stablein, UC Irvine Medical Center, Orange, CA, United States; Fayez M. Bany-Mohammed, UC Irvine Medical Center, Orange, CA, United States
- BN
Bret Nolan, DO
Neonatology Fellow
UCI Medical Center
Alhambra , California, United States
Presenting Author(s)
Background: Congenital Hypothyroidism (CH) is a known cause of severe neurodevelopmental impairment. VLBW infants are at higher risk for delayed TSH rise and CH which may be missed by State newborn screening (NBS). More than 25 states mandate repeat thyroid screening in this vulnerable population, but not California. Our institution started performing repeat thyroid screening in October 2011.
Objective: The goal of this study is to determine the prevalence of: 1) delayed TSH rise and its associated co-morbidities. 2) CH requiring thyroxine replacement therapy.
Design/Methods: This is a retrospective chart review of VLBW infants born at UCI Medical Center between 1/1/2012 and 9/230/2019. Repeat thyroid screens (TSH and Free T4) were obtained at 30 (+ 7) days. Infants with abnormal screens underwent follow up testing and pediatric endocrinology consultation. Initial NBS and repeat thyroid screens data were collected via chart review. Demographic data and short-term outcomes were prospectively collected as part of participation in the California Perinatal Quality Care Collaborative (CPQCC). Exclusion criteria were congenital malformations, death, transfer, discharge before 30 days of age, or out-born infants admitted to UCI outside the screening window.
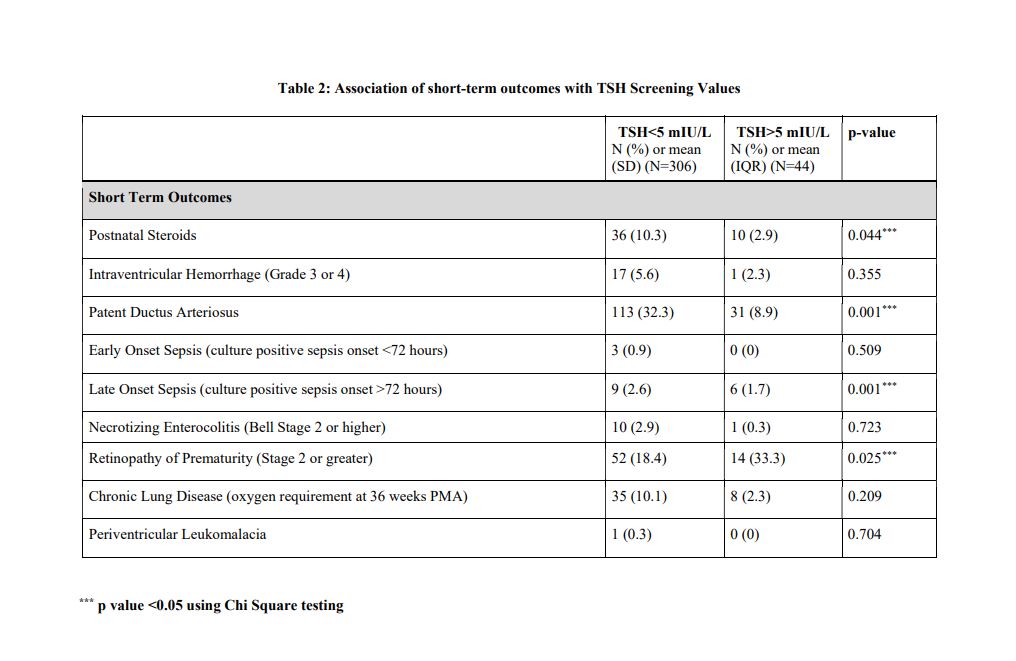
Results: Three hundred and fifty patients who met the eligibility criteria were included. Delayed TSH rise was defined as TSH >5 uIU/ml. CH was diagnosed by pediatric endocrinologist based on persistent and up trending TSH values. Infant and maternal demographic data and short-term outcomes of infants with delayed TSH rise compared with those screened normal is shown in Tables 1&2 (attached). Forty-four patients (12.5%) were diagnosed with delayed TSH rise; none of them were identified by State NBS. Upon multiple logistic regression analysis, risk factors associated with delayed TSH rise included low birth weight (p < 0.006), patent ductus arteriosus (p < 0.003), late onset sepsis (p 0.019) and prolonged length of stay (p 0.002). CH requiring thyroxine treatment through NICU discharge was diagnosed in three patients (prevalence of 0.8%).Conclusion(s): Delayed TSH rise is relatively common in VLBW infants. Those infants, including some with CH requiring thyroxine therapy, are missed by State NBS. We recommend repeat thyroid screening (Free T4, TSH) in VLBW infants to identify CH that may require impactful hormone replacement therapy.
Table 1: Association of demographic and maternal/ delivery room data with TSH Screening Values.jpg)
Table 2: Association of short-term outcomes with TSH Screening Values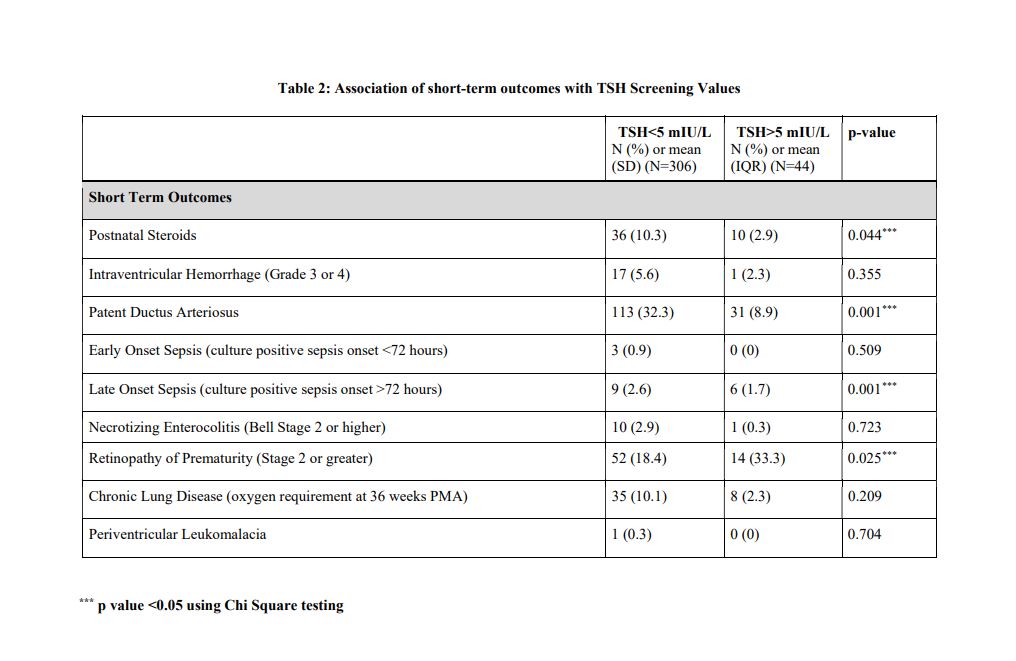
Objective: The goal of this study is to determine the prevalence of: 1) delayed TSH rise and its associated co-morbidities. 2) CH requiring thyroxine replacement therapy.
Design/Methods: This is a retrospective chart review of VLBW infants born at UCI Medical Center between 1/1/2012 and 9/230/2019. Repeat thyroid screens (TSH and Free T4) were obtained at 30 (+ 7) days. Infants with abnormal screens underwent follow up testing and pediatric endocrinology consultation. Initial NBS and repeat thyroid screens data were collected via chart review. Demographic data and short-term outcomes were prospectively collected as part of participation in the California Perinatal Quality Care Collaborative (CPQCC). Exclusion criteria were congenital malformations, death, transfer, discharge before 30 days of age, or out-born infants admitted to UCI outside the screening window.
Results: Three hundred and fifty patients who met the eligibility criteria were included. Delayed TSH rise was defined as TSH >5 uIU/ml. CH was diagnosed by pediatric endocrinologist based on persistent and up trending TSH values. Infant and maternal demographic data and short-term outcomes of infants with delayed TSH rise compared with those screened normal is shown in Tables 1&2 (attached). Forty-four patients (12.5%) were diagnosed with delayed TSH rise; none of them were identified by State NBS. Upon multiple logistic regression analysis, risk factors associated with delayed TSH rise included low birth weight (p < 0.006), patent ductus arteriosus (p < 0.003), late onset sepsis (p 0.019) and prolonged length of stay (p 0.002). CH requiring thyroxine treatment through NICU discharge was diagnosed in three patients (prevalence of 0.8%).Conclusion(s): Delayed TSH rise is relatively common in VLBW infants. Those infants, including some with CH requiring thyroxine therapy, are missed by State NBS. We recommend repeat thyroid screening (Free T4, TSH) in VLBW infants to identify CH that may require impactful hormone replacement therapy.
Table 1: Association of demographic and maternal/ delivery room data with TSH Screening Values
.jpg)
Table 2: Association of short-term outcomes with TSH Screening Values