Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement III: GI and Nutrition
233 - A quality improvement project to reduce necrotizing enterocolitis in high-risk neonates
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 233
Publication Number: 233.128
Publication Number: 233.128
Stephanie Mavis, Mayo Clinic Children's Center, Rochester, MN, United States; Maria C. Gallup, Mayo Clinic, Rochester, MN, United States; Megan A. Misgen, Mayo Clinic Children's Center, New Richland, MN, United States; Laura Schram, Mayo Clinic, Saint Charles, MN, United States; Danielle Herzog, Mayo Clinic Children's Center, Rochester, MN, United States; Brandi Smith, Mayo Clinic Children's Center, Rochester, MN, United States; Angela L. Giese, Mayo Clinic Children's Center, Kasson, MN, United States; Roxanne K. Torgerson, Mayo Clinic Children's Center, Wabasha, MN, United States; Raymond Stetson, Mayo Clinic, Rochester, MN, United States; Jennifer Fang, Mayo Clinic Children's Center, Rochester, MN, United States

Stephanie Mavis, MD (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Mayo Clinic Children's Center
Rochester, Minnesota, United States
Presenting Author(s)
Background: In June 2020, we identified an increase in rates of severe NEC despite unit guidelines and adherence to several known best obstetric and neonatal practices, including antenatal steroid administration, exclusive human milk diets, access to donor breastmilk, and limited use of H2 blockers and antibiotics.
Objective: We aimed to decrease the rate of NEC (Bell’s Stage 2 or greater) in neonates admitted to our Level IV NICU with gestational age (GA) < 30 0/7 weeks and/or very low birth weight (VLBW, < 1500 grams) from 19.5% to less than 9.7% (a 50% reduction) over 24 months, without adversely affecting CLABSI rates. Our secondary improvement measure was the rate of surgical NEC in the same population.
Design/Methods: Our multidisciplinary team used Define-Measure-Analyze-Improve-Control (DMAIC) as our improvement model, including tools such as stakeholder analysis, fishbone diagrams, key driver diagrams, 5 why’s analysis, and impact-effort grids to understand the root causes of our gap and develop potential interventions. PDSA cycles (July 2020 to October 2021) focused on increasing administration rates of oral cares during the first two weeks of life, promoting the early maternal milk supply, increasing access to donor breastmilk, centralizing milk preparation, and reducing the maximum gavage tube dwell times. We regularly monitored stage 2 or greater NEC and adherence to QI interventions. Process measures (oral cares compliance, feeding composition, and gavage tube dwell times) were analyzed via Mann-Whitney and Chi-squared tests.
Results: 116 neonates were included in the improvement project (41 baseline, 75 improve). Combined stage 2 and 3 NEC rates in VLBW infants or infants < 30 weeks GA decreased from a baseline median of 19% to a current median of 4%. Surgical NEC rates decreased from a median of 7% to 0%. Compared with our baseline population, infants in the Improve Phase received significantly more oral cares (median 0% vs 52% of all opportunities provided, p < 0.001) and had lower maximum gavage tube dwell times (median 13 vs. 17 days, p = 0.03). Neonates in the Improve Phase also had less exposure to any preterm formula (0% vs. 7% infants exposed, p = 0.08). There were no CLABSIs during our QI period. A control plan to ensure sustained improvements includes ongoing monitoring of NEC and compliance with the process improvements. Conclusion(s): A multidisciplinary approach has led to improvements in stage 2 or greater NEC, which may be mediated by ongoing adherence to known best practices in NEC reduction, improved oral cares administration, and decreased gavage tube dwell times.
Key driver diagram guiding quality improvement project..png) The key driver diagram illustrates our QI group's improvement theory to reduce severe NEC in high-risk neonates in our level IV NICU.
The key driver diagram illustrates our QI group's improvement theory to reduce severe NEC in high-risk neonates in our level IV NICU.
Run chart of stage 2 or greater NEC in QI population over time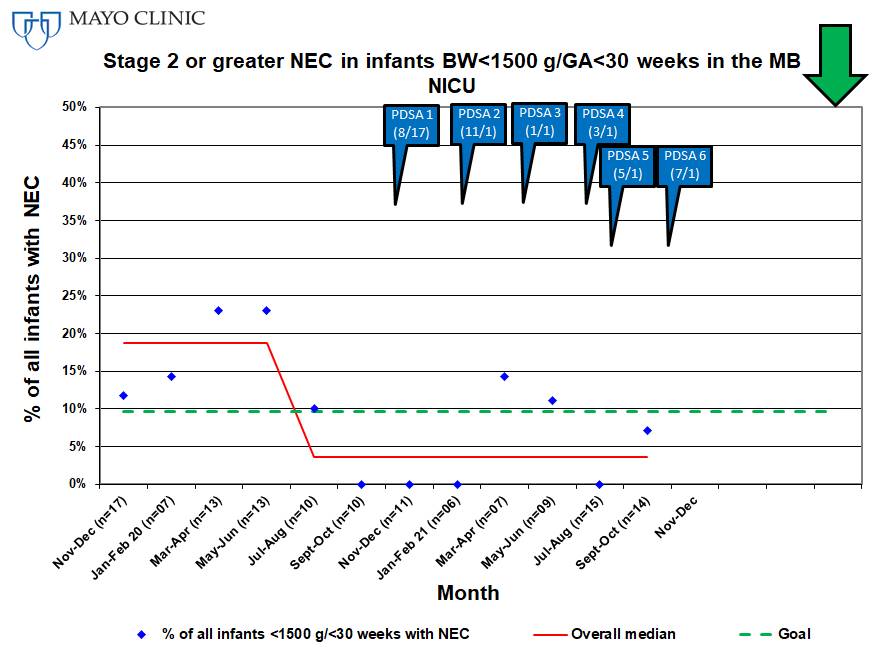 Stage 2 and 3 NEC in baseline cohort (November 2019-June 2020) demonstrates median NEC rate of 19%. In Improve Phase (July 2020-October 2021), NEC rates decrease to median of 4%.
Stage 2 and 3 NEC in baseline cohort (November 2019-June 2020) demonstrates median NEC rate of 19%. In Improve Phase (July 2020-October 2021), NEC rates decrease to median of 4%.
Objective: We aimed to decrease the rate of NEC (Bell’s Stage 2 or greater) in neonates admitted to our Level IV NICU with gestational age (GA) < 30 0/7 weeks and/or very low birth weight (VLBW, < 1500 grams) from 19.5% to less than 9.7% (a 50% reduction) over 24 months, without adversely affecting CLABSI rates. Our secondary improvement measure was the rate of surgical NEC in the same population.
Design/Methods: Our multidisciplinary team used Define-Measure-Analyze-Improve-Control (DMAIC) as our improvement model, including tools such as stakeholder analysis, fishbone diagrams, key driver diagrams, 5 why’s analysis, and impact-effort grids to understand the root causes of our gap and develop potential interventions. PDSA cycles (July 2020 to October 2021) focused on increasing administration rates of oral cares during the first two weeks of life, promoting the early maternal milk supply, increasing access to donor breastmilk, centralizing milk preparation, and reducing the maximum gavage tube dwell times. We regularly monitored stage 2 or greater NEC and adherence to QI interventions. Process measures (oral cares compliance, feeding composition, and gavage tube dwell times) were analyzed via Mann-Whitney and Chi-squared tests.
Results: 116 neonates were included in the improvement project (41 baseline, 75 improve). Combined stage 2 and 3 NEC rates in VLBW infants or infants < 30 weeks GA decreased from a baseline median of 19% to a current median of 4%. Surgical NEC rates decreased from a median of 7% to 0%. Compared with our baseline population, infants in the Improve Phase received significantly more oral cares (median 0% vs 52% of all opportunities provided, p < 0.001) and had lower maximum gavage tube dwell times (median 13 vs. 17 days, p = 0.03). Neonates in the Improve Phase also had less exposure to any preterm formula (0% vs. 7% infants exposed, p = 0.08). There were no CLABSIs during our QI period. A control plan to ensure sustained improvements includes ongoing monitoring of NEC and compliance with the process improvements. Conclusion(s): A multidisciplinary approach has led to improvements in stage 2 or greater NEC, which may be mediated by ongoing adherence to known best practices in NEC reduction, improved oral cares administration, and decreased gavage tube dwell times.
Key driver diagram guiding quality improvement project.
.png) The key driver diagram illustrates our QI group's improvement theory to reduce severe NEC in high-risk neonates in our level IV NICU.
The key driver diagram illustrates our QI group's improvement theory to reduce severe NEC in high-risk neonates in our level IV NICU.Run chart of stage 2 or greater NEC in QI population over time
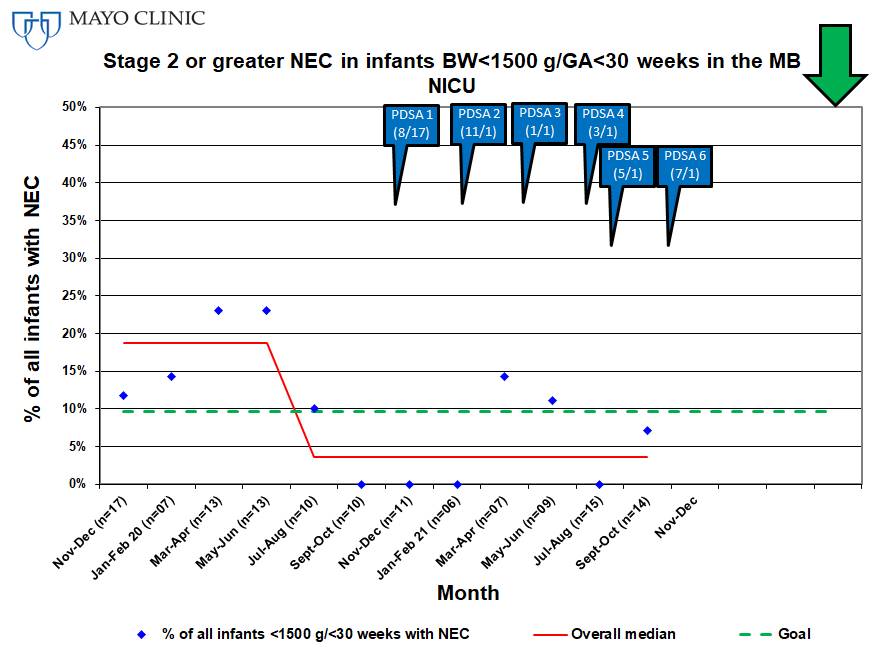 Stage 2 and 3 NEC in baseline cohort (November 2019-June 2020) demonstrates median NEC rate of 19%. In Improve Phase (July 2020-October 2021), NEC rates decrease to median of 4%.
Stage 2 and 3 NEC in baseline cohort (November 2019-June 2020) demonstrates median NEC rate of 19%. In Improve Phase (July 2020-October 2021), NEC rates decrease to median of 4%.