Back
General Pediatrics: Primary Care/Prevention
Category: Abstract Submission
General Pediatrics III
169 - Food insecurity screening, social needs program engagement, and clinic visits for children with special healthcare needs
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 169
Publication Number: 169.316
Publication Number: 169.316
Charmaine Yuan, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Kristin Topel, Johns Hopkins University, Baltimore, MD, United States; Laura Prichett, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Rama B. Imad, Hopkins Community Connection, Baltimore, MD, United States; Julia M. Kim, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Barry S. Solomon, Johns Hopkins University School of Medicine, Baltimore, MD, United States
Charmaine Yuan, BS
Medical student
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background:
Food insecurity is a major social determinant of health that disproportionately affects families with children with complex medical needs; unfortunately, Supplemental Security Income (SSI) is often inadequate. Our objective was to assess the association between emergency food receipt and enrollment in a clinic-based social needs program (Hopkins Community Connection, HCC) on follow-up rates among families receiving SSI in the Harriet Lane Clinic (HLC).
Objective: Our objective was to assess the association between emergency food receipt and enrollment in a clinic-based social needs program (Hopkins Community Connection, HCC) on follow-up rates among families receiving SSI in the Harriet Lane Clinic (HLC).
Design/Methods:
In this retrospective cohort study, we conducted a chart review to compare SSI patients who did and did not receive food and those who did and did not enroll in HCC during HLC visits between March-December 2020; number of diagnoses and no-show rates were also abstracted. Adjusted logistic regression was used to determine if food receipt and/or HCC enrollment increased the likelihood of attending primary and specialty care follow-up appointments (FU) by July 2020.
Results: In bivariate analysis, compared to those who did not enroll with HCC, a higher percentage of enrolled SSI patients completed a FU (49% vs. 70%, P < 0.05). SSI patients who completed a FU had a significantly lower no-show rate than those who did not (21% vs. 27%, P < 0.01). Food receipt and number of diagnoses were not associated with FU. Adjusting for number of diagnoses, no-show rate, and then both, the association between food receipt and completing a FU and between HCC enrollment and FU remained non-significant. Conclusion(s): HCC enrollment and no-show rate were found to be significantly associated with completed FU while food receipt and number of diagnoses were not. All findings from the logistic regression were non-significant but suggested that providing emergency food and helping families access community resources may be effective interventions to increase attendance at follow-up appointments. Based on chart review, a majority of the sample was not screened for food insecurity, offering an area for improvement.
ResumeCharmaine Yuan_Resume Jan 2022.pdf
Table 2: Logistic regression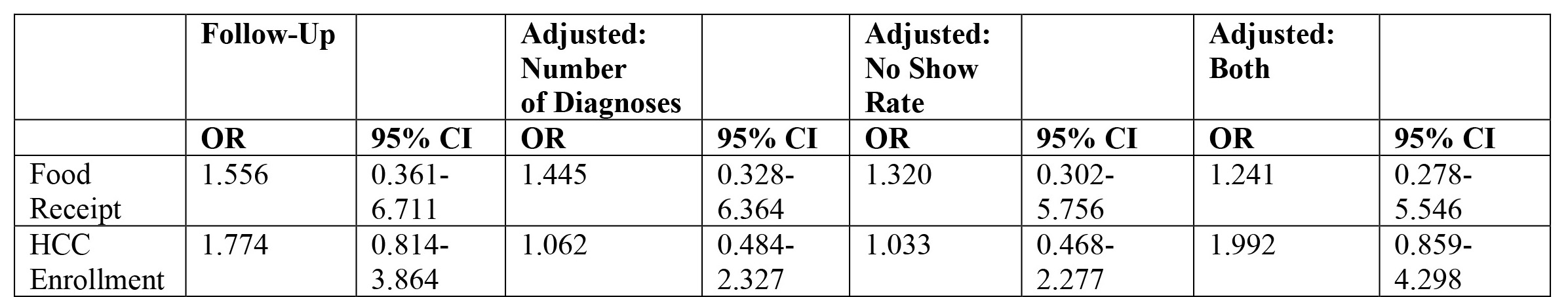 Increased odds of follow-up, non-significant.
Increased odds of follow-up, non-significant.
Food insecurity is a major social determinant of health that disproportionately affects families with children with complex medical needs; unfortunately, Supplemental Security Income (SSI) is often inadequate. Our objective was to assess the association between emergency food receipt and enrollment in a clinic-based social needs program (Hopkins Community Connection, HCC) on follow-up rates among families receiving SSI in the Harriet Lane Clinic (HLC).
Objective: Our objective was to assess the association between emergency food receipt and enrollment in a clinic-based social needs program (Hopkins Community Connection, HCC) on follow-up rates among families receiving SSI in the Harriet Lane Clinic (HLC).
Design/Methods:
In this retrospective cohort study, we conducted a chart review to compare SSI patients who did and did not receive food and those who did and did not enroll in HCC during HLC visits between March-December 2020; number of diagnoses and no-show rates were also abstracted. Adjusted logistic regression was used to determine if food receipt and/or HCC enrollment increased the likelihood of attending primary and specialty care follow-up appointments (FU) by July 2020.
Results: In bivariate analysis, compared to those who did not enroll with HCC, a higher percentage of enrolled SSI patients completed a FU (49% vs. 70%, P < 0.05). SSI patients who completed a FU had a significantly lower no-show rate than those who did not (21% vs. 27%, P < 0.01). Food receipt and number of diagnoses were not associated with FU. Adjusting for number of diagnoses, no-show rate, and then both, the association between food receipt and completing a FU and between HCC enrollment and FU remained non-significant. Conclusion(s): HCC enrollment and no-show rate were found to be significantly associated with completed FU while food receipt and number of diagnoses were not. All findings from the logistic regression were non-significant but suggested that providing emergency food and helping families access community resources may be effective interventions to increase attendance at follow-up appointments. Based on chart review, a majority of the sample was not screened for food insecurity, offering an area for improvement.
ResumeCharmaine Yuan_Resume Jan 2022.pdf
Table 2: Logistic regression
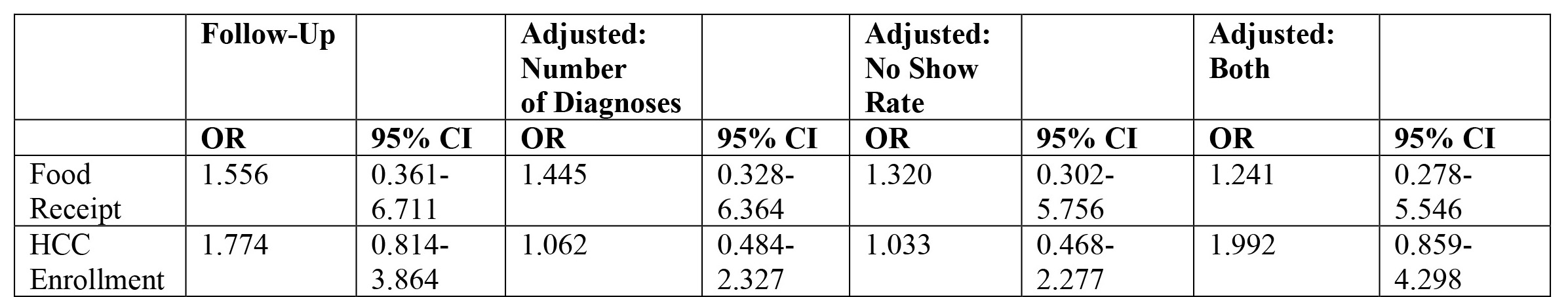 Increased odds of follow-up, non-significant.
Increased odds of follow-up, non-significant.