Palliative Care
Category: Abstract Submission
Palliative Care I
514 - Factors Influencing Provider Perceptions of Good vs Bad Deaths in the PICU
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 514
Publication Number: 514.140
Publication Number: 514.140
Jason Werner, Saint Louis University, St. Louis, MO, United States; Benjamin M. Rooney, United States Department of Veterans Affairs, Chicago, IL, United States; Melinda J. Owens, Saint Louis University, New Athens, IL, United States; Fletcher Hoague, Saint Louis University School of Medicine, St. Louis, MO, United States; Lauren R. Draper, Saint Louis University School of Medicine, Saint Louis, MO, United States
- FH
Fletcher Hoague, MPH, MSW, LMSW
Program Specialist
Saint Louis University School of Medicine
St. Louis, Missouri, United States
Presenting Author(s)
Background: A large proportion of patients who die in children's hospitals do so in the Pediatric Intensive Care Unit (PICU). Patient deaths can be a major driver of mental health problems for registered nurses (RNs) in the PICU. Not all deaths are perceived equally by RNs, and the potential for the grief and loss of some deaths to be balanced by a release from suffering and distress is recognized. Teams debriefing after patient deaths is known to provide opportunities to learn from the event and also to process and validate provider feelings.
Objective: As part of a scoping review for future qualitative research, we sought to determine how often PICU RNs perceived deaths as "good" vs "bad", how often deaths in the PICU were debriefed, and what the effect of patient age was on perceptions and debriefing.
Design/Methods: Work was conducted in a university-associated, free-standing urban children's hospital. Surveys were distributed to PICU RNs in March, 2020 using a secure, anonymous Qualtrics link distributed through an employee email list as well as by paper copies in a break area in the PICU. Subjects were asked demographic and professional information as well as subjective questions regarding their participation in a patient death in the PICU.
Results: 41 of 76 potential subjects returned surveys (54%). Respondents all identified as female and averaged 29 years old. 35 of 41 subjects reported ever participating in a death, and the mean time since participation was 7.5 months (SD 6.6mos). Of these, 24/35 were perceived as "bad". 70% of bad and 40% of good deaths were debriefed. 13/24 deaths had some discordance between whether the family and/or the medical team had anticipated the patient's death, but this did not affect perceptions of "good" vs "bad" (p=0.36). No bad deaths were expected by the family but not by the medical team. Patient age did not affect perceptions of quality of death (p=0.75). No respondents indicated that participation negatively affected their ability to care for future patients, though respondents indicated some degree of ongoing reflection about the death (0-3pt "never"-"often" scale, "at work" mean 1.5, SD 0.7. "At home" mean 1.5, SD 0.86). Bad deaths were debriefed more often than good ones (p=0.09), but neither age (p=0.90) nor discordant expectations (p=0.37) affected how often debriefings were conducted.Conclusion(s): PICU RNs frequently participate in patient deaths, not all of which are debriefed. Deaths perceived as "bad" were more likely to be debriefed. This work was supported by a grant from the Midamerica Transplant Foundation.
Debriefings by Patient Age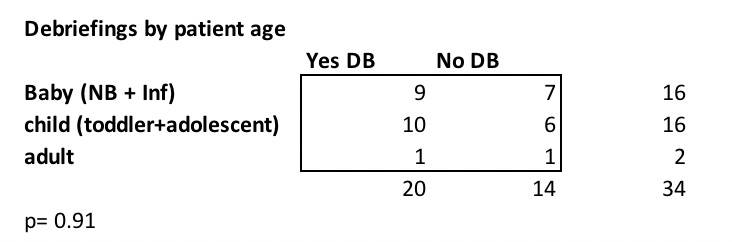 Team debriefings conducted based on patient age categorization (infant, child, adult)
Team debriefings conducted based on patient age categorization (infant, child, adult)
Debriefings by Quality Perceived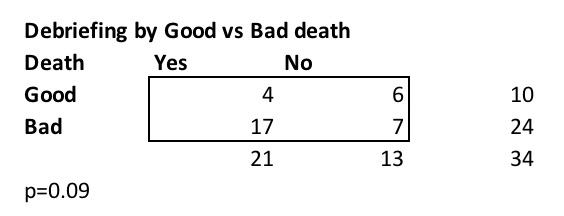 Team debriefings conducted based on RN perception of quality of patient death (good vs bad)
Team debriefings conducted based on RN perception of quality of patient death (good vs bad)
Objective: As part of a scoping review for future qualitative research, we sought to determine how often PICU RNs perceived deaths as "good" vs "bad", how often deaths in the PICU were debriefed, and what the effect of patient age was on perceptions and debriefing.
Design/Methods: Work was conducted in a university-associated, free-standing urban children's hospital. Surveys were distributed to PICU RNs in March, 2020 using a secure, anonymous Qualtrics link distributed through an employee email list as well as by paper copies in a break area in the PICU. Subjects were asked demographic and professional information as well as subjective questions regarding their participation in a patient death in the PICU.
Results: 41 of 76 potential subjects returned surveys (54%). Respondents all identified as female and averaged 29 years old. 35 of 41 subjects reported ever participating in a death, and the mean time since participation was 7.5 months (SD 6.6mos). Of these, 24/35 were perceived as "bad". 70% of bad and 40% of good deaths were debriefed. 13/24 deaths had some discordance between whether the family and/or the medical team had anticipated the patient's death, but this did not affect perceptions of "good" vs "bad" (p=0.36). No bad deaths were expected by the family but not by the medical team. Patient age did not affect perceptions of quality of death (p=0.75). No respondents indicated that participation negatively affected their ability to care for future patients, though respondents indicated some degree of ongoing reflection about the death (0-3pt "never"-"often" scale, "at work" mean 1.5, SD 0.7. "At home" mean 1.5, SD 0.86). Bad deaths were debriefed more often than good ones (p=0.09), but neither age (p=0.90) nor discordant expectations (p=0.37) affected how often debriefings were conducted.Conclusion(s): PICU RNs frequently participate in patient deaths, not all of which are debriefed. Deaths perceived as "bad" were more likely to be debriefed. This work was supported by a grant from the Midamerica Transplant Foundation.
Debriefings by Patient Age
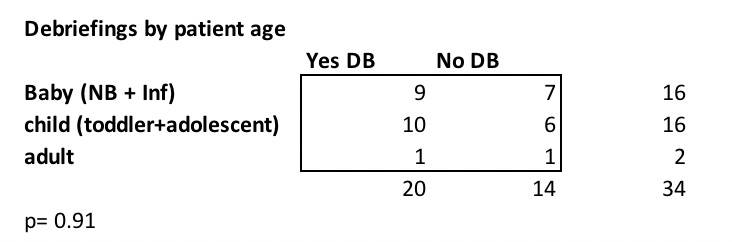 Team debriefings conducted based on patient age categorization (infant, child, adult)
Team debriefings conducted based on patient age categorization (infant, child, adult)Debriefings by Quality Perceived
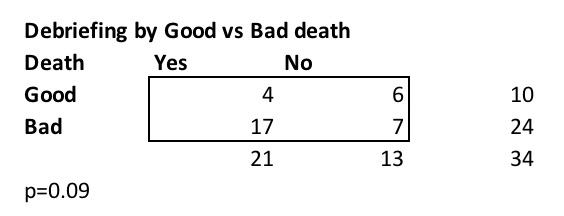 Team debriefings conducted based on RN perception of quality of patient death (good vs bad)
Team debriefings conducted based on RN perception of quality of patient death (good vs bad)