Neonatal Pulmonology
Category: Abstract Submission
Neonatal Pulmonology III: Molecular Markers and Clinical Prediction Models/Outcomes
Sequelae associated with ‘systemic’ hypertension in infants with severe bronchopulmonary dysplasia
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 452B
Publication Number: 452B.431
Publication Number: 452B.431
Arvind Sehgal, Monash Children’s Hospital, Melbourne, Victoria, Australia; Kristy L. Elsayed, Monash Children's Hospital, Hampton, Victoria, Australia; Matilda E. Nugent, Monash Health, Melbourne, Victoria, Australia; Suraj K. Varma, MonashHeart, Monash Health, Melbourne, Victoria, Australia

Arvind Sehgal, PhD (he/him/his)
Neonatologist
Monash Children's Hospital
MELBOURNE, Victoria, Australia
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) literature has almost exclusively focussed on ‘pulmonary’ hypertension; information on the clinical relevance of ‘systemic’ hypertension is lacking. Data from more than two decades back noted an incidence of 7-43%, used BPD definition as O2 dependancy at 28 days & varied blood pressure (BP) criteria. The 2017 Clinical Practice Guideline on Childhood Hypertension (AAP) recommends the use of derived BP centiles based on post-menstrual age (PMA), providing 95th & 99th centiles.
Objective: To ascertain the incidence & clinical relevance of systemic hypertension amongst preterm infants with ‘severe’ BPD.
Design/Methods: Retrospective study of six-year data was performed for preterm infants who survived until 36 weeks PMA. Infants with BPD were compared with twice the number of gestation matched subsequent admissions with no BPD. 7-day morning BP (36+0-36+6 week) was compared with published 95th centile cut-offs and correlated with sequelae.
Results: 57 infants with ‘severe’ BPD were compared with 114 infants with no BPD. The GA and BW between the groups and the use of antenatal steroids, surfactant and UAC were comparable (Table 1). The number of infants having multiple readings ≥95th centile during the 7-day period between 36+0-36+6 weeks PMA was significantly higher in the BPD cohort vs no BPD infants (systolic BP, 23/57 [40%] vs 3/114 [2.6%], p < 0.001 & mean BP, 26/57 [46%] vs 3/114 [2.6%], p < 0.001). Six infants (10.5%) had 7-day systolic BP average ≥95th centile while nine (16%) had 7-day mean BP average ≥95th centile. Table 2 compares systolic & mean BP during the study period. The 7-day average systolic & mean BP was significantly higher in infants with BPD compared to infants with no BPD (median [range], 72mm Hg [54-96] vs 63 [56-84], p < 0.001 and 54 mm Hg [40-73] vs 45 mm Hg [39-67], p < 0.001), respectively. The significance persisted after adjusting for GA and BW separately, and combined. Table 3 compares BPD infants with systolic BP ≥95th centile and < 95th centile. Higher BP was associated with significantly greater odds (3.5 [95% CI, 0.7, 16] for discharge with home oxygen and longer duration of respiratory support. Seven of 23 (30.4%) BPD infants with hypertension were administered captopril (none in the no BPD group).Conclusion(s): The contribution of systemic circulation towards BPD pathophysiology is not particularly appreciated. Systemic hypertension seems to be a significant issue in infants with BPD, with important implications for management as well as prognosis.
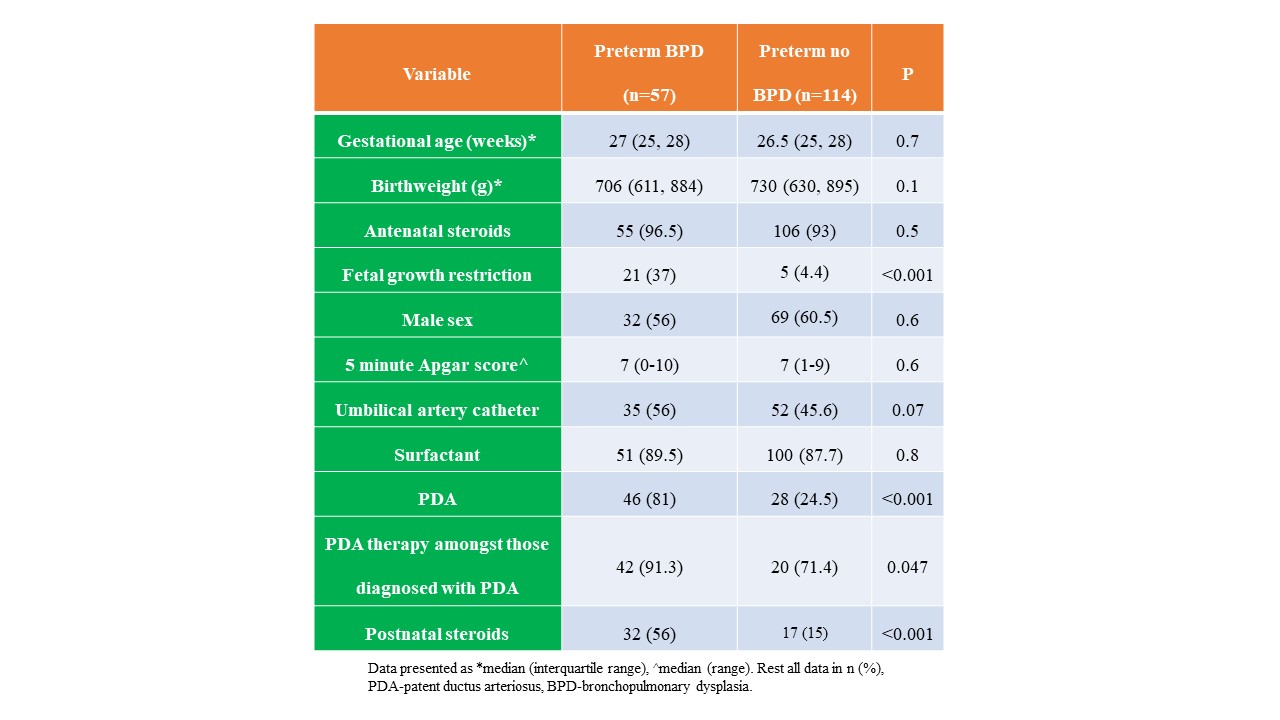
Demographic and clinical data of the study population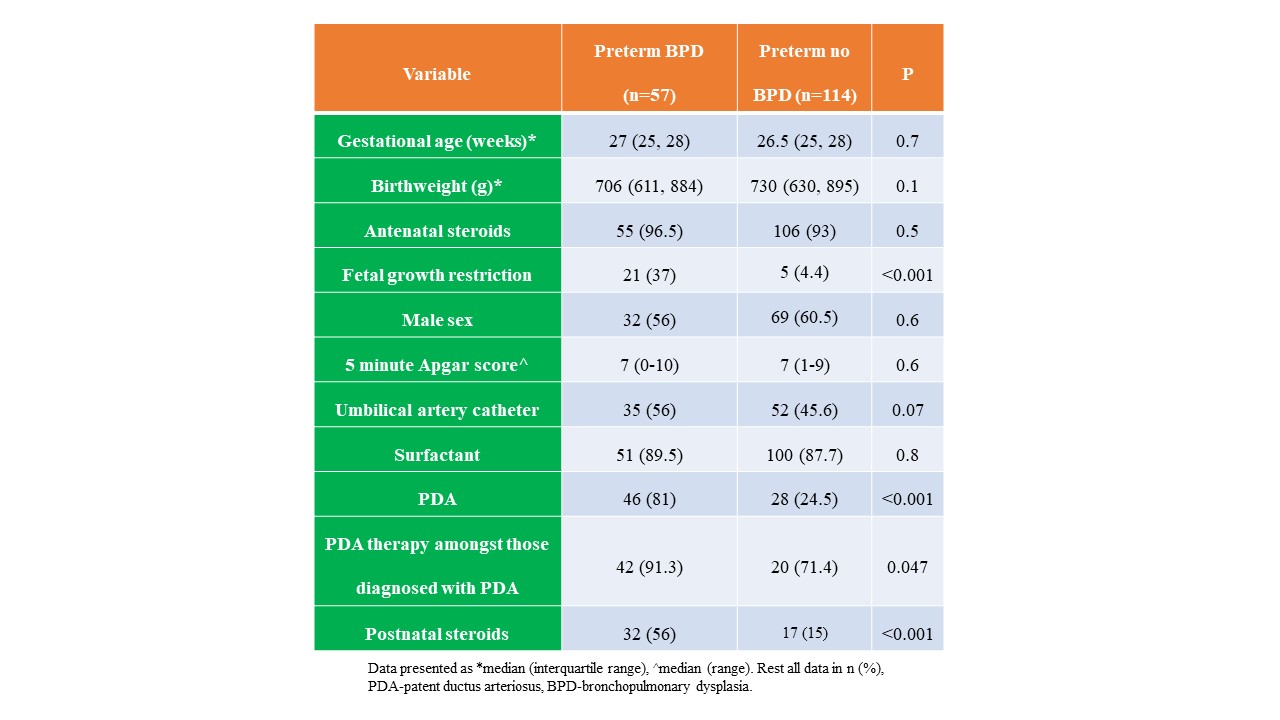
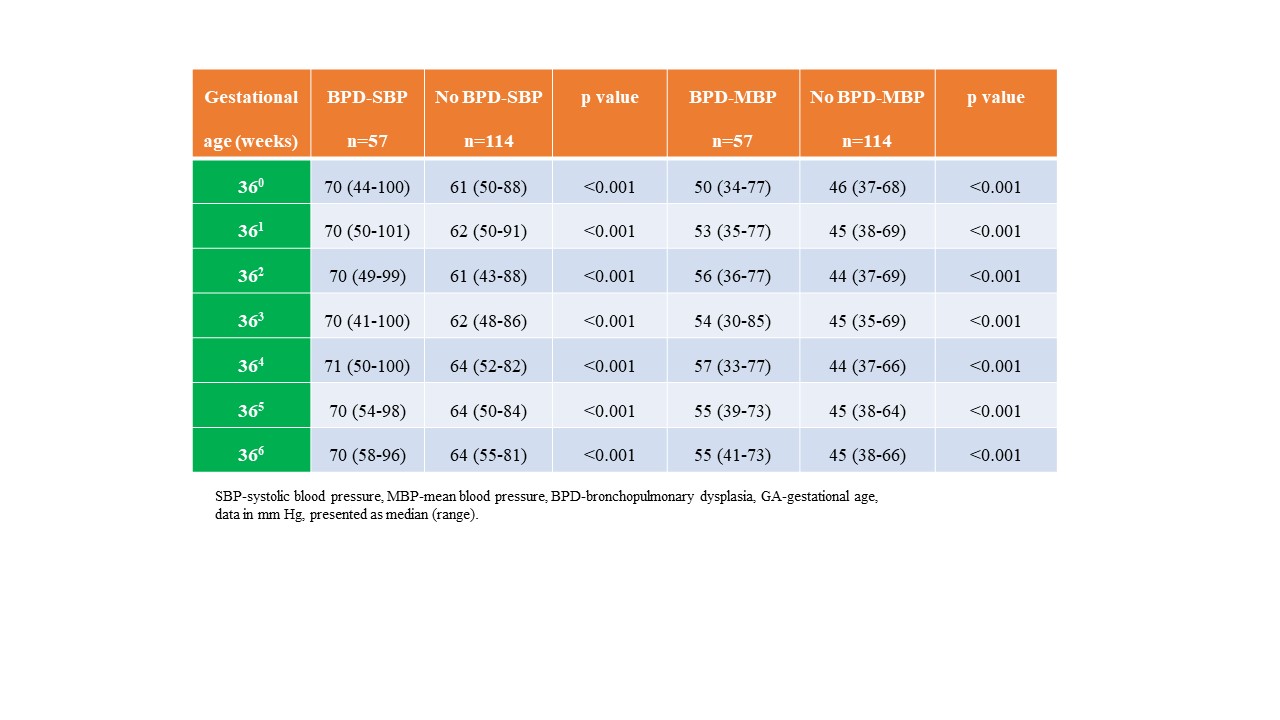
Systolic and mean blood pressure data of the cohort (36+0-36+6 weeks post-menstrual age)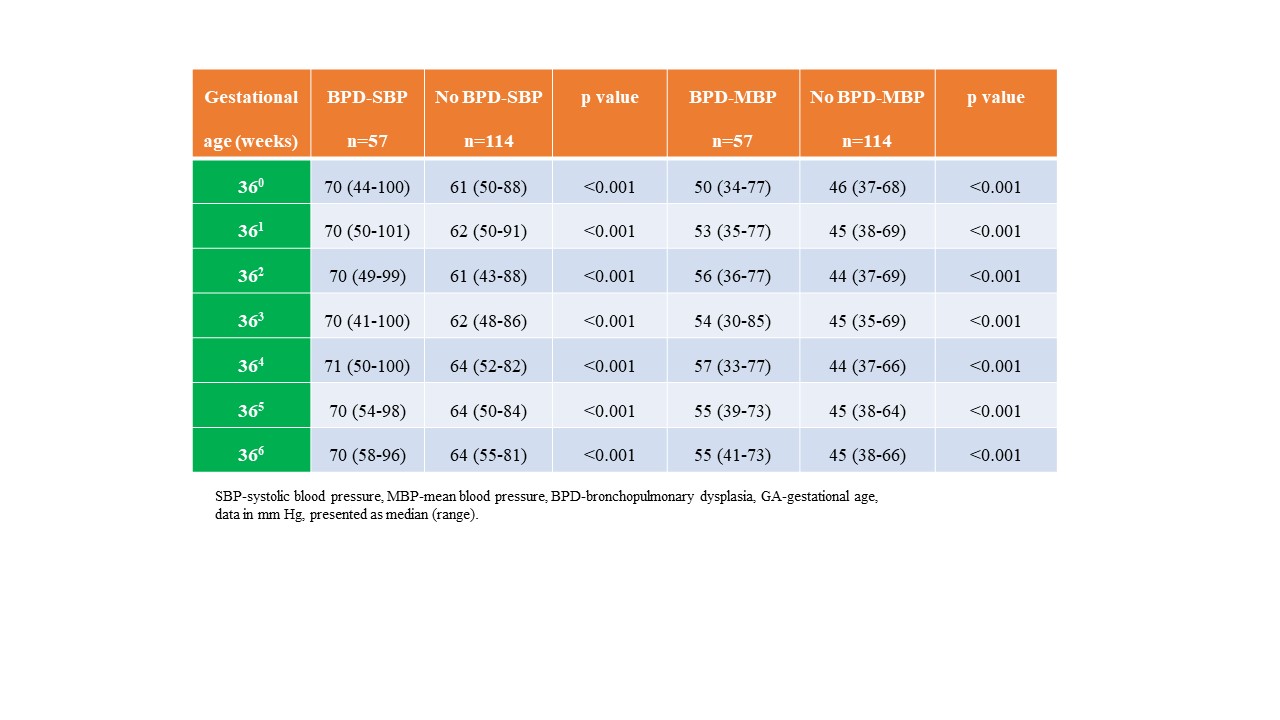
Objective: To ascertain the incidence & clinical relevance of systemic hypertension amongst preterm infants with ‘severe’ BPD.
Design/Methods: Retrospective study of six-year data was performed for preterm infants who survived until 36 weeks PMA. Infants with BPD were compared with twice the number of gestation matched subsequent admissions with no BPD. 7-day morning BP (36+0-36+6 week) was compared with published 95th centile cut-offs and correlated with sequelae.
Results: 57 infants with ‘severe’ BPD were compared with 114 infants with no BPD. The GA and BW between the groups and the use of antenatal steroids, surfactant and UAC were comparable (Table 1). The number of infants having multiple readings ≥95th centile during the 7-day period between 36+0-36+6 weeks PMA was significantly higher in the BPD cohort vs no BPD infants (systolic BP, 23/57 [40%] vs 3/114 [2.6%], p < 0.001 & mean BP, 26/57 [46%] vs 3/114 [2.6%], p < 0.001). Six infants (10.5%) had 7-day systolic BP average ≥95th centile while nine (16%) had 7-day mean BP average ≥95th centile. Table 2 compares systolic & mean BP during the study period. The 7-day average systolic & mean BP was significantly higher in infants with BPD compared to infants with no BPD (median [range], 72mm Hg [54-96] vs 63 [56-84], p < 0.001 and 54 mm Hg [40-73] vs 45 mm Hg [39-67], p < 0.001), respectively. The significance persisted after adjusting for GA and BW separately, and combined. Table 3 compares BPD infants with systolic BP ≥95th centile and < 95th centile. Higher BP was associated with significantly greater odds (3.5 [95% CI, 0.7, 16] for discharge with home oxygen and longer duration of respiratory support. Seven of 23 (30.4%) BPD infants with hypertension were administered captopril (none in the no BPD group).Conclusion(s): The contribution of systemic circulation towards BPD pathophysiology is not particularly appreciated. Systemic hypertension seems to be a significant issue in infants with BPD, with important implications for management as well as prognosis.
Demographic and clinical data of the study population
Systolic and mean blood pressure data of the cohort (36+0-36+6 weeks post-menstrual age)