Neonatal General
Category: Abstract Submission
Neonatology General 3
370 - Adverse perinatal outcomes associated with increasing maternal obesity
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 370
Publication Number: 370.133
Publication Number: 370.133
matthew nudelman, Marshall University Joan C. Edwards School of Medicine, huntington, WV, United States; Katherine Addicott, Marshall University Joan C. Edwards School of Medicine, Huntington, WV, United States; Krista Putty, Phoenix Children's Hospital, Phoenix, AZ, United States; Priya Prasher, Phoenix Children’s Hospital, Phoenix, AZ, United States; Deborah L. Preston, Marshall University Joan C. Edwards School of Medicine, Huntington, WV, United States; Joseph W. Werthammer, Marshall University Joan C. Edwards School of Medicine, Barboursville, WV, United States
- MN
Matthew Nudelman, MD, MAS
Pediatrics, PGY-2
Marshall University Joan C. Edwards School of Medicine
Huntington, West Virginia, United States
Presenting Author(s)
Background: Obesity incidence in the US continues to increase. In 2019 West Virginia had the 2nd highest rate of adult obesity at 40%. Evidence suggests maternal obesity increases the incidence of adverse perinatal outcomes.
Objective: To determine adverse perinatal outcomes related to pre-conception body mass index (BMI).
Design/Methods: This is a retrospective observational study from single tertiary care perinatal center of women giving birth from 1/1/2015-12/31/2018. The study was based out of Cabell Huntington Hospital in Huntington, West Virginia. Five hundred consecutive mothers with a pre-conception BMI of 18.5-24.9 and 500 additional mothers with a pre-conception BMI >30 were identified. Mother/baby dyads were excluded gestational age < 36 weeks, neonatal congenital anomalies, and maternal substance use. Maternal/newborn metrics are described using descriptive statistics stratified by maternal pre-conception BMI. We used simple-univariable and multivariable logistic regression models to evaluate associations between pre-conception BMI and specific obstetric/neonatal outcomes including cesarean section (CS), pre-eclampsia, gestational diabetes, 5-minute apgar score, and NICU admission. Regression models used continuous (non-stratified) maternal pre-conception BMI. Covariates used in the multivariable logistic regression model included advanced maternal age, pre-existing maternal diabetes, pre-existing maternal hypertension, and infant gestational age.
Results: The study included 861 mother/baby dyads after 139 were excluded. Patient selection flow diagram are presented (figure 1). Maternal and newborn metrics stratified by maternal pre-conception BMI are presented (table 1). Simple univariable logistic regression models demonstrated higher pre-conception BMI was significantly associated with progressively higher rates of CS, pre-eclampsia, gestational diabetes, and NICU admission. These associations remained significant in multivariable logistic models except admission to the NICU (table 2).Conclusion(s): We have demonstrated that obese women (pre-conception BMI >=30) are more likely to have maternal complications and neonatal morbidity when compared to normal weight women (pre-conception BMI 18.5-24.9). Maternal and fetal complications increase with increasing obesity with superobese mothers having more perinatal adverse outcomes when compared to other classes of obesity. It is reasonable to counsel weight loss prior to conception of women with pre-conception BMI >=30 to reduce maternal complications and neonatal morbidity related to pregnancy.
Figure 1: Flowchart of patient selection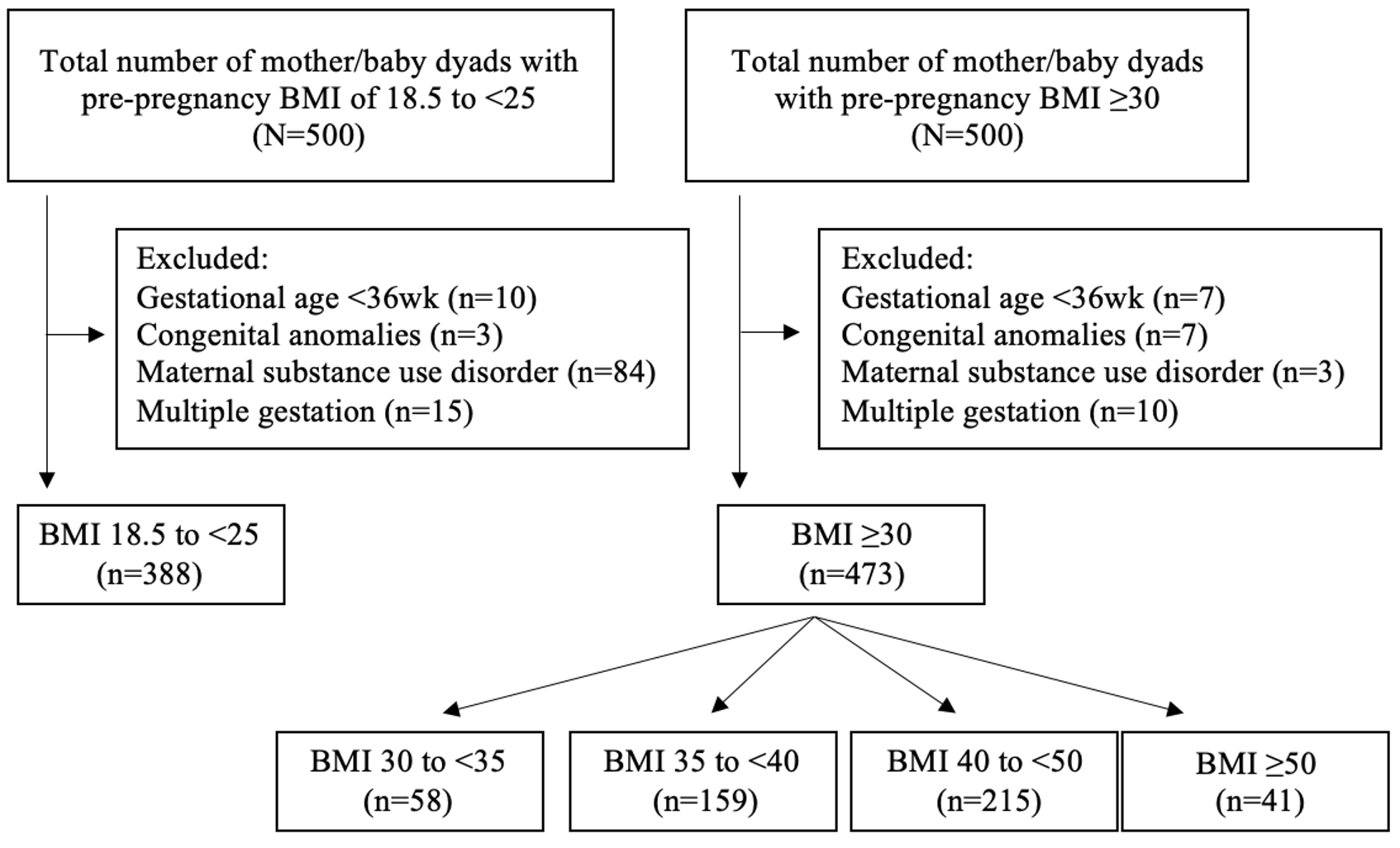
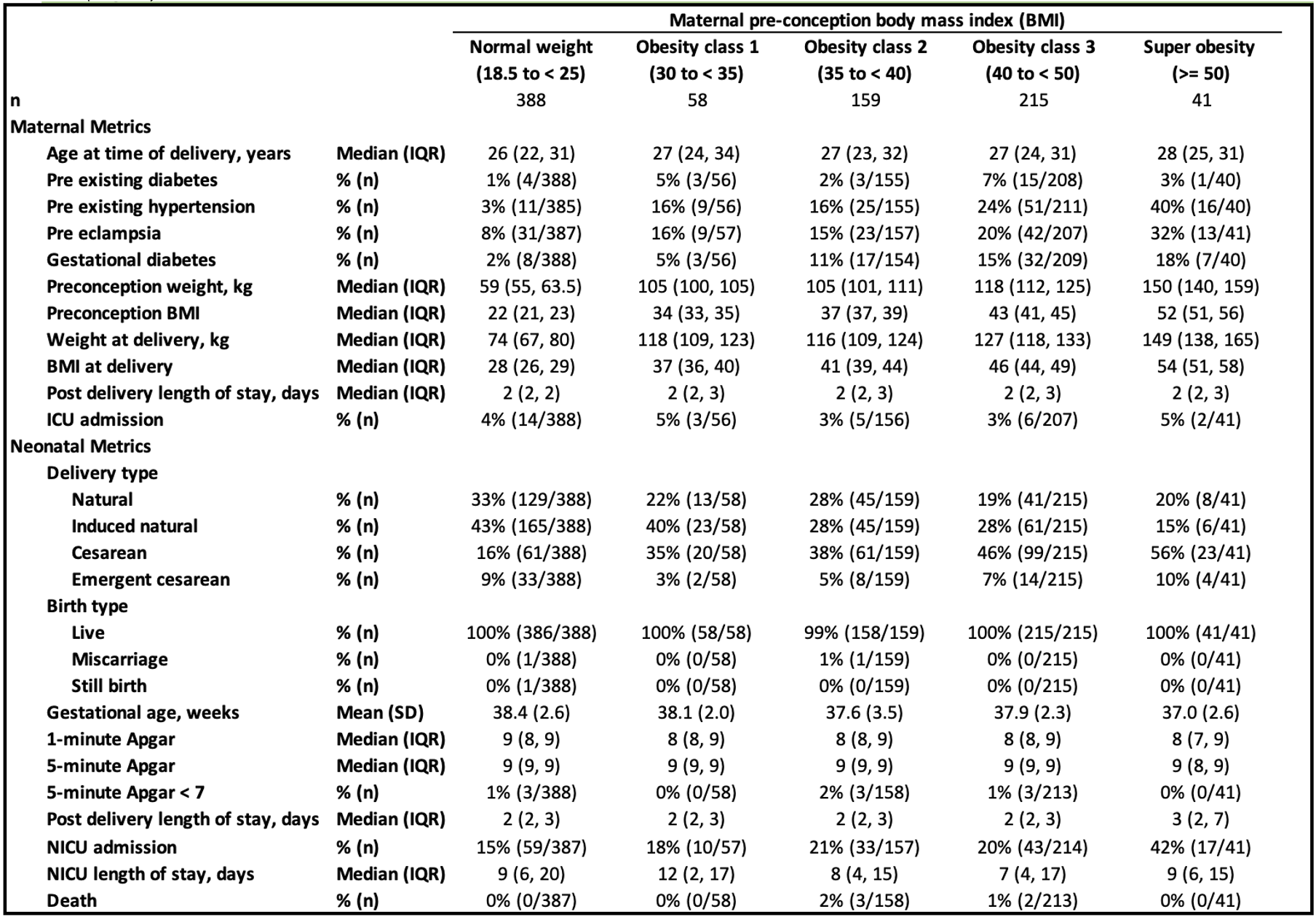
Table 1: Descriptive Statistics of Obstetric/Neonatal Variables and Maternal Pre-conception Body Mass Index (BMI), N = 861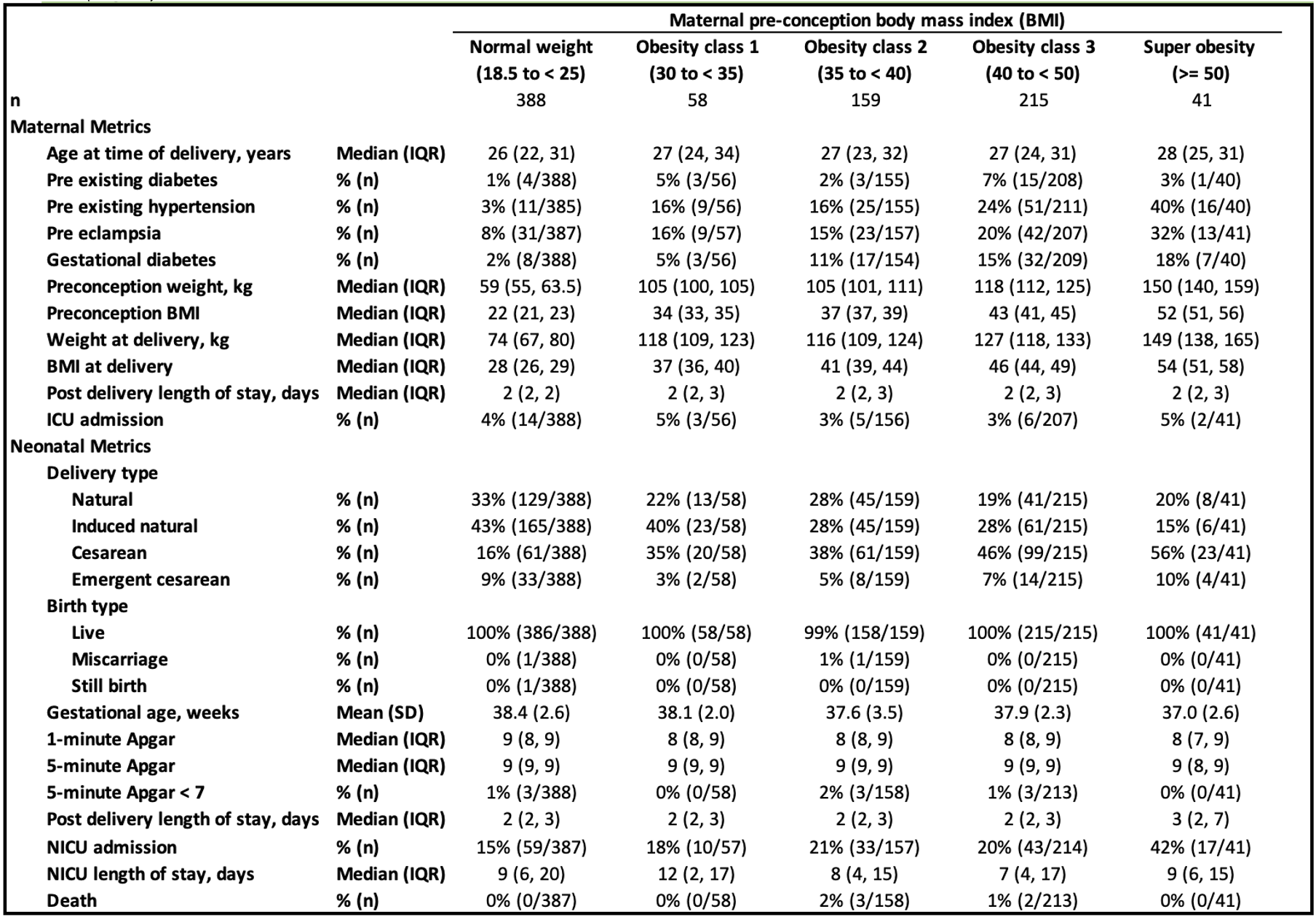
Objective: To determine adverse perinatal outcomes related to pre-conception body mass index (BMI).
Design/Methods: This is a retrospective observational study from single tertiary care perinatal center of women giving birth from 1/1/2015-12/31/2018. The study was based out of Cabell Huntington Hospital in Huntington, West Virginia. Five hundred consecutive mothers with a pre-conception BMI of 18.5-24.9 and 500 additional mothers with a pre-conception BMI >30 were identified. Mother/baby dyads were excluded gestational age < 36 weeks, neonatal congenital anomalies, and maternal substance use. Maternal/newborn metrics are described using descriptive statistics stratified by maternal pre-conception BMI. We used simple-univariable and multivariable logistic regression models to evaluate associations between pre-conception BMI and specific obstetric/neonatal outcomes including cesarean section (CS), pre-eclampsia, gestational diabetes, 5-minute apgar score, and NICU admission. Regression models used continuous (non-stratified) maternal pre-conception BMI. Covariates used in the multivariable logistic regression model included advanced maternal age, pre-existing maternal diabetes, pre-existing maternal hypertension, and infant gestational age.
Results: The study included 861 mother/baby dyads after 139 were excluded. Patient selection flow diagram are presented (figure 1). Maternal and newborn metrics stratified by maternal pre-conception BMI are presented (table 1). Simple univariable logistic regression models demonstrated higher pre-conception BMI was significantly associated with progressively higher rates of CS, pre-eclampsia, gestational diabetes, and NICU admission. These associations remained significant in multivariable logistic models except admission to the NICU (table 2).Conclusion(s): We have demonstrated that obese women (pre-conception BMI >=30) are more likely to have maternal complications and neonatal morbidity when compared to normal weight women (pre-conception BMI 18.5-24.9). Maternal and fetal complications increase with increasing obesity with superobese mothers having more perinatal adverse outcomes when compared to other classes of obesity. It is reasonable to counsel weight loss prior to conception of women with pre-conception BMI >=30 to reduce maternal complications and neonatal morbidity related to pregnancy.
Figure 1: Flowchart of patient selection
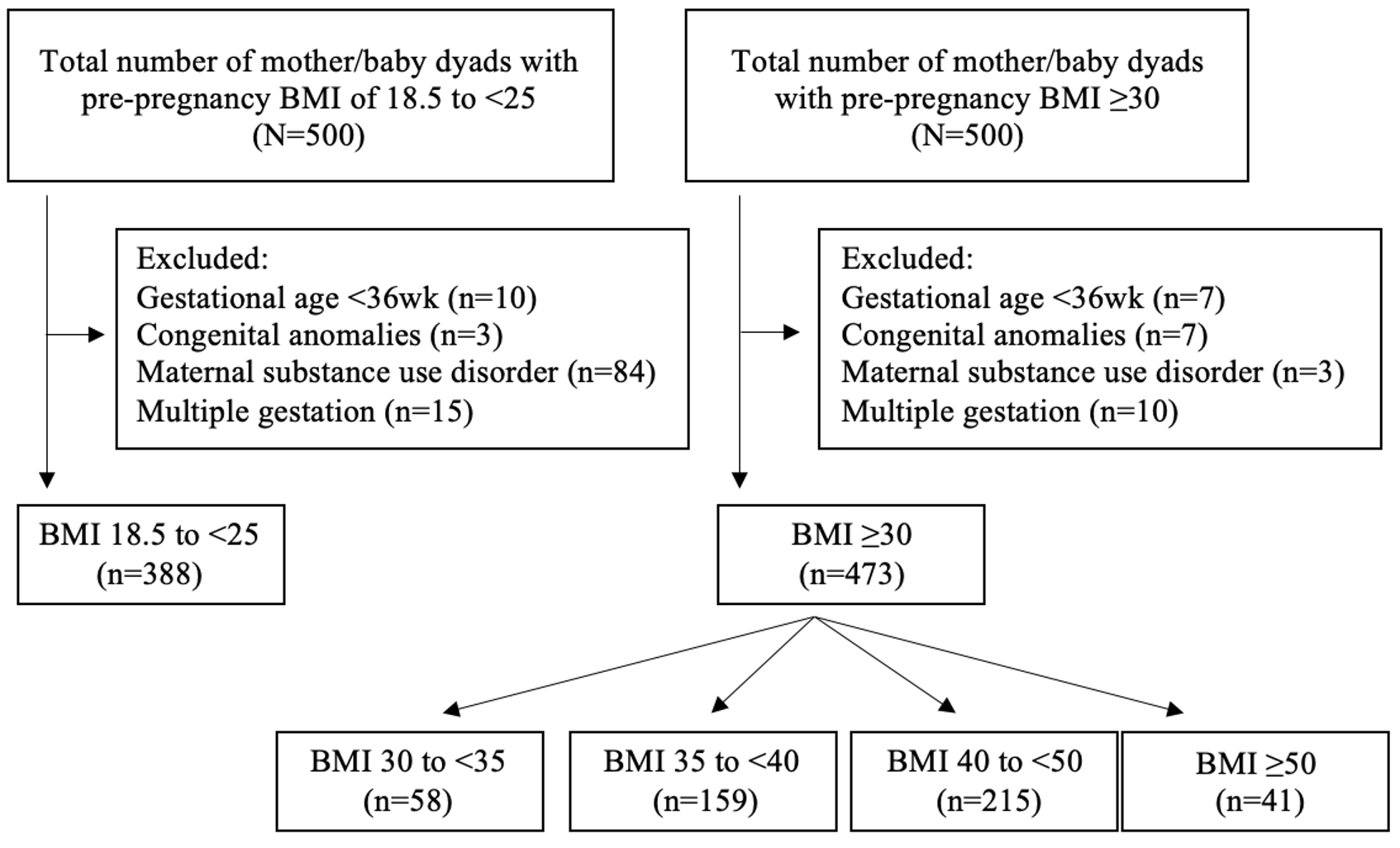
Table 1: Descriptive Statistics of Obstetric/Neonatal Variables and Maternal Pre-conception Body Mass Index (BMI), N = 861