Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine IV
76 - Assessing the New Procedural Norm in the Era of Covid-19: A Simulation Study to Assess Pediatric Emergency Medicine Physcian Success in Critical Procedures While Wearing an Air-purifying Respirator
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 76
Publication Number: 76.106
Publication Number: 76.106
Noormah Mehmood, University of Texas Southwestern Medical School, Dallas, TX, United States; Jo-ann Nesiama, University of Texas Southwestern Medical School, Coppell, TX, United States; Kenneth Yen, University of Texas Southwestern Medical School, Dallas, TX, United States; Geoffrey Lowe, University of Texas Southwestern Medical School, Irving, TX, United States

Noormah Mehmood, MD
Fellow
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background:
Healthcare workers (HCWs) caring for patients with COVID-19 are at high risk for contracting the virus and as such significant emphasis has been placed on proper personal protective equipment (PPE) such as a battery powered air-purifying respirator (APR). This is the first study to assess the impact of advanced PPE, specifically APR across four common critical care procedures performed by pediatric emergency medicine (PEM) physicians.
Objective:
To determine the impact of APR on: Endotracheal intubation, Bag-Valve mask ventilation (BMV), Intraosseous (IO) insertion and Lumbar puncture (LP), measured by metrics of procedural success.
Design/Methods:
PEM physicians working in a tertiary, level 1 trauma center performed endotracheal intubation, BMV, LP and IO on a high-fidelity mannequin.
Comparison was drawn between subjects performing an IO and LP with standard (eye protection and mask) precautions versus donning an APR by two consistent observers. Overall success rate, number of attempts, maintenance of sterility for LP and time towards successful completion were recorded.
For Endotracheal intubation and BMV, a direct comparison was drawn between two commonly utilized APRs; powered air-purifying respirator (PAPR) and Controlled air purifying respirator (CAPR) with regards to procedural success and number of attempts towards successful completion.
Results:
20 participants performed IO and LP using an APR and standard precautions.IO insertion had a 100% success rate with a median attempt of 1 for both groups (p= 0.56).Mean average time using standard precautions vs APR was 26.6s and 23.8s respectfully (p=0.6).
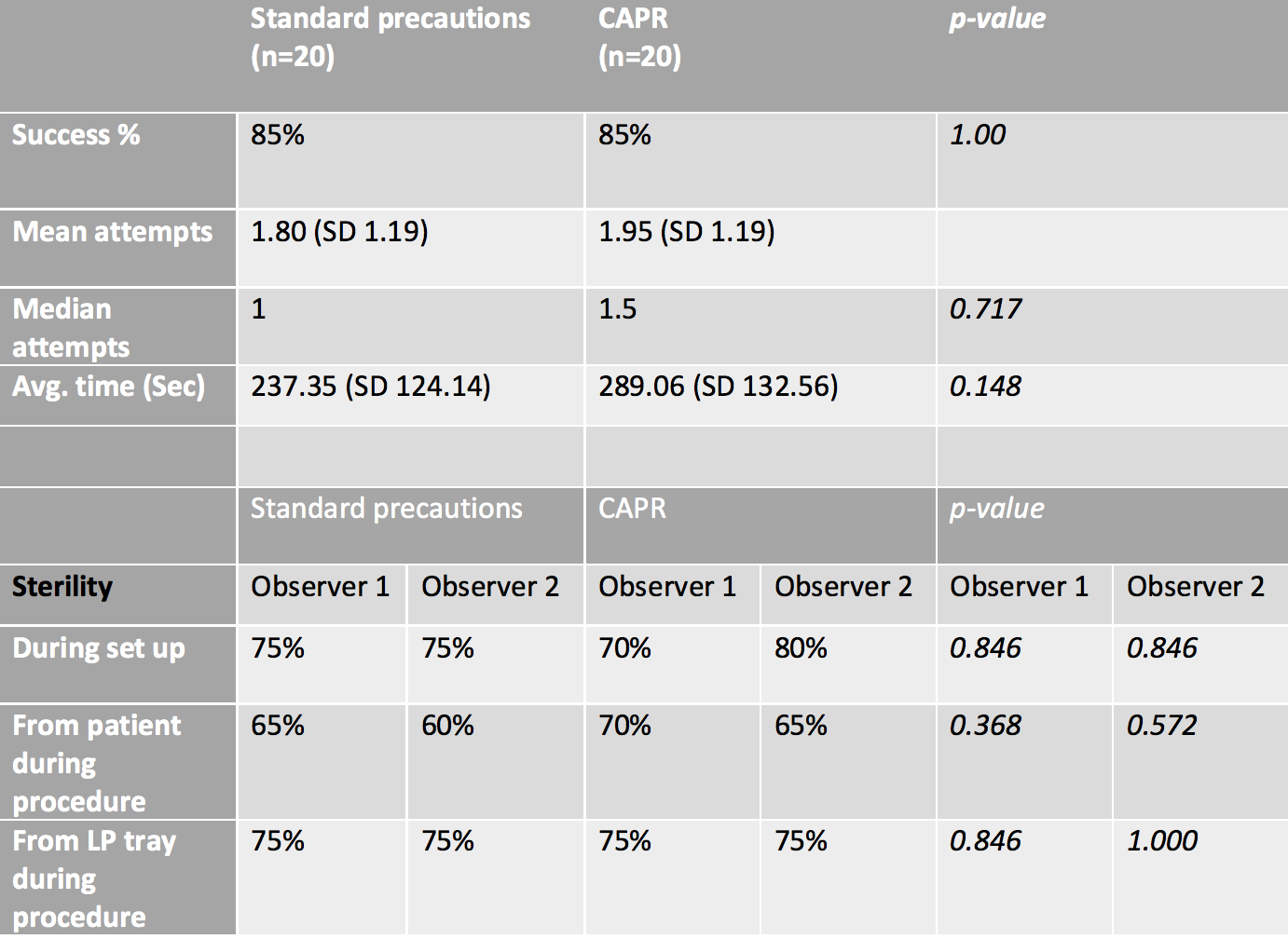
LP was successful 85% of times in both arms, with median attempts of 1 in standard precautions versus 1.5 in the APR group (p=0.71).The mean average time using standard precautions was 237s versus 289s for the APR group (p=0.15).There was no statistically significant difference in observed sterility during set up or performance of the procedure.
20 total participants, divided across PAPR and CAPR groups performed Intubation and BMV for comparison. Success rate for both procedures across the two groups was 100% with a similar median of 1 (p=1.0).
Conclusion(s):
No statistically significant difference was found in overall procedure success when utilizing advanced versus standard PPE. The type of APR used (CAPR versus PAPR) also did not have a statistically significant impact on the metrics of overall procedure success in this pilot simulation study. Wearing increased levels of PPE did not impact procedural success in our study. During the pandemic, HCWs should be encouraged to wear appropriate PPE.
CV Noormah Mehmood 2021.pdf
Table shows comparison between metrics of Lumbar puncture, including success rate, mean and median number of attempts with standard deviation (SD) between the Controlled air purifying respirator (CAPR) and standard precautions group. Measures of sterility with two consistent observers is also shown.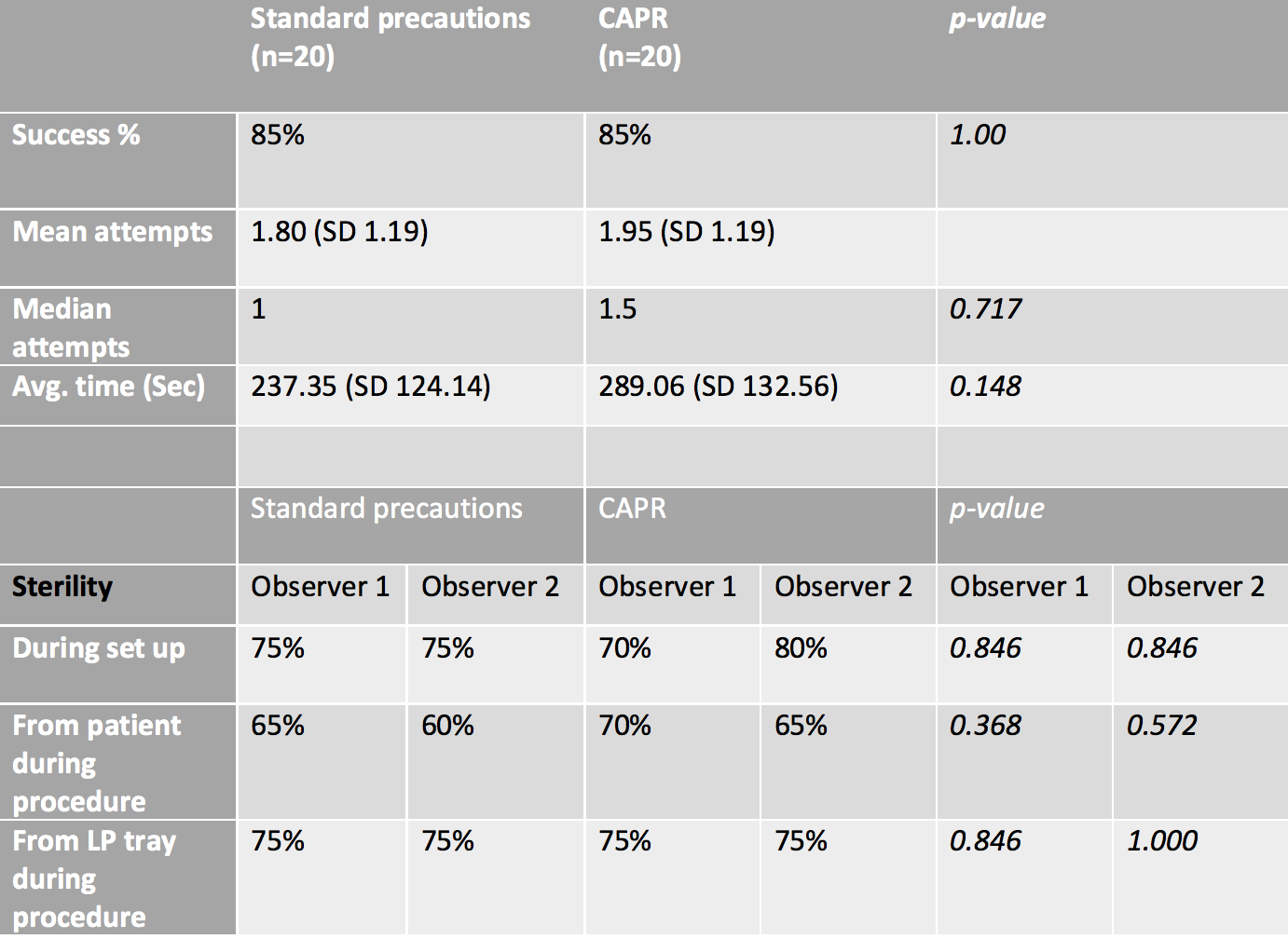
Healthcare workers (HCWs) caring for patients with COVID-19 are at high risk for contracting the virus and as such significant emphasis has been placed on proper personal protective equipment (PPE) such as a battery powered air-purifying respirator (APR). This is the first study to assess the impact of advanced PPE, specifically APR across four common critical care procedures performed by pediatric emergency medicine (PEM) physicians.
Objective:
To determine the impact of APR on: Endotracheal intubation, Bag-Valve mask ventilation (BMV), Intraosseous (IO) insertion and Lumbar puncture (LP), measured by metrics of procedural success.
Design/Methods:
PEM physicians working in a tertiary, level 1 trauma center performed endotracheal intubation, BMV, LP and IO on a high-fidelity mannequin.
Comparison was drawn between subjects performing an IO and LP with standard (eye protection and mask) precautions versus donning an APR by two consistent observers. Overall success rate, number of attempts, maintenance of sterility for LP and time towards successful completion were recorded.
For Endotracheal intubation and BMV, a direct comparison was drawn between two commonly utilized APRs; powered air-purifying respirator (PAPR) and Controlled air purifying respirator (CAPR) with regards to procedural success and number of attempts towards successful completion.
Results:
20 participants performed IO and LP using an APR and standard precautions.IO insertion had a 100% success rate with a median attempt of 1 for both groups (p= 0.56).Mean average time using standard precautions vs APR was 26.6s and 23.8s respectfully (p=0.6).
LP was successful 85% of times in both arms, with median attempts of 1 in standard precautions versus 1.5 in the APR group (p=0.71).The mean average time using standard precautions was 237s versus 289s for the APR group (p=0.15).There was no statistically significant difference in observed sterility during set up or performance of the procedure.
20 total participants, divided across PAPR and CAPR groups performed Intubation and BMV for comparison. Success rate for both procedures across the two groups was 100% with a similar median of 1 (p=1.0).
Conclusion(s):
No statistically significant difference was found in overall procedure success when utilizing advanced versus standard PPE. The type of APR used (CAPR versus PAPR) also did not have a statistically significant impact on the metrics of overall procedure success in this pilot simulation study. Wearing increased levels of PPE did not impact procedural success in our study. During the pandemic, HCWs should be encouraged to wear appropriate PPE.
CV Noormah Mehmood 2021.pdf
Table shows comparison between metrics of Lumbar puncture, including success rate, mean and median number of attempts with standard deviation (SD) between the Controlled air purifying respirator (CAPR) and standard precautions group. Measures of sterility with two consistent observers is also shown.