Neonatal General
Category: Abstract Submission
Neonatology General 7: ROP - Endocrine
430 - Associations of receipt of packed red blood cell transfusions and oral iron supplementation with the development of retinopathy of prematurity.
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 430
Publication Number: 430.137
Publication Number: 430.137
Bharath Srivatsa, Northside Hospital, Atlanta, GA, United States; Claire Pearson, Northside Hospital, Atlanta, GA, United States; Joseph Hagan, Baylor College of Medicine, Houston, TX, United States
- BS
Bharath Srivatsa, MD
Attending Neonatologist
Northside Hospital
Atlanta, Georgia, United States
Presenting Author(s)
Background: Exposure to exogenous iron in the form of iron supplementation or packed red cell (PRBC) transfusions has been implicated in the etiopathogenesis of retinopathy of prematurity (ROP). However, there are no recent studies examining this association. Despite instituting exclusive human milk feeding and strict oxygen targeting and titration practices, the occurrence of severe ROP in our NICU has not been eliminated. This prompted us to examine our oral iron supplementation and PRBC transfusion practices to see if any changes could be implemented to further decrease our low ROP rates.
Objective: The objective of this retrospective case-control analysis is to study the associations of oral iron supplementation and receipt of PRBC transfusions with retinopathy of prematurity.
Design/Methods: This retrospective study examined the receipt of oral iron and PRBC transfusions during the first two postnatal months among extremely low birth weight infants (birthweight < 1000 grams) born between January 1, 2016 - December 31, 2020, who survived to have an eye exam.
The study population was divided into three groups. Group 1 No ROP. Group 2 Mild (Stage 1 and 2) ROP. Group 3 consisted of babies who developed severe (Stage 3) ROP.The Institutional Review Board (IRB) at Northside Hospital approved this study.
ROP screening was performed as per AAP guidelines. Standard statistical tests were used to determine normality of data and compare differences between groups in univariate and multivariate models.
Results: Among the 101 study infants, 53 did not develop ROP, 33 developed mild ROP and 15 developed severe ROP including 6 who required treatment. There were baseline differences in the study population (Table 1).
There were differences in the cumulative dose of oral iron and number of PRBC transfusions in the sudy population (Figure 1). Patients with no ROP received significantly fewer PRBC Txs than patients with mild ROP (p < 0.001) and severe ROP (p < 0.001). Patients with no ROP received significantly higher cumulative iron doses than patients with mild ROP (p=0.026). After controlling for birth weight, gestational age, race, ethnicity, 5-minute Apgar score, and ventilator days, the differences in the number of PBRC Txs (p < 0.001) remained statistically significant but the difference in cumulative iron dose was no longer significant (p=0.252). (Table 2)Conclusion(s): In contrast to prior literature, ROP was not associated with the cumulative dose of oral iron in our study. We did find a positive correlation between the occurrence of ROP and number of PRBC transfusions.
Table 1. Demographic and clinical characteristics of the study infants.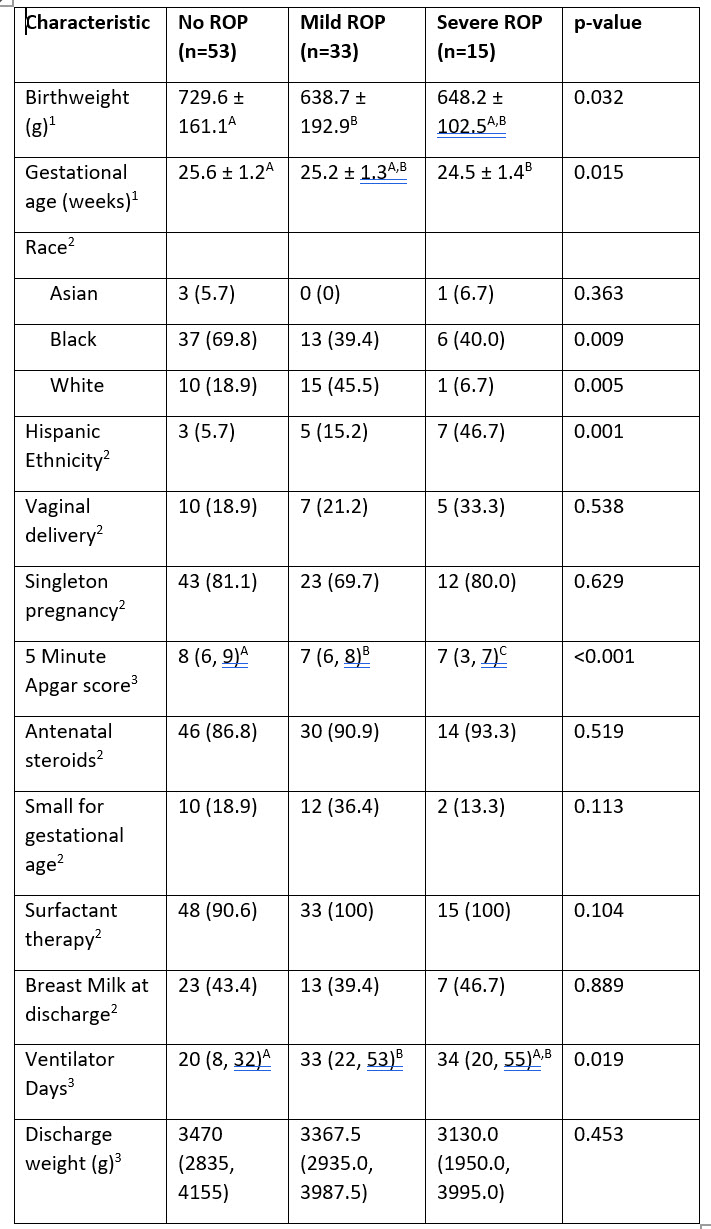 1. Mean ± standard deviation, ANOVA p-value. Groups with different superscript letters are significantly different (Tukey’s HSD test p < 0.05).
1. Mean ± standard deviation, ANOVA p-value. Groups with different superscript letters are significantly different (Tukey’s HSD test p < 0.05).
2. Frequency (%), Fisher’s exact test p-value
3. Median (inter-quartile range), Kruskal-Wallis test p-value. Groups with different letters are significantly different (Tukey’s HSD test p < 0.05).
Figure 1. Number of PRBC transfusions and cumulative iron dose among the study infants during first 2 postnatal months..jpg)
Objective: The objective of this retrospective case-control analysis is to study the associations of oral iron supplementation and receipt of PRBC transfusions with retinopathy of prematurity.
Design/Methods: This retrospective study examined the receipt of oral iron and PRBC transfusions during the first two postnatal months among extremely low birth weight infants (birthweight < 1000 grams) born between January 1, 2016 - December 31, 2020, who survived to have an eye exam.
The study population was divided into three groups. Group 1 No ROP. Group 2 Mild (Stage 1 and 2) ROP. Group 3 consisted of babies who developed severe (Stage 3) ROP.The Institutional Review Board (IRB) at Northside Hospital approved this study.
ROP screening was performed as per AAP guidelines. Standard statistical tests were used to determine normality of data and compare differences between groups in univariate and multivariate models.
Results: Among the 101 study infants, 53 did not develop ROP, 33 developed mild ROP and 15 developed severe ROP including 6 who required treatment. There were baseline differences in the study population (Table 1).
There were differences in the cumulative dose of oral iron and number of PRBC transfusions in the sudy population (Figure 1). Patients with no ROP received significantly fewer PRBC Txs than patients with mild ROP (p < 0.001) and severe ROP (p < 0.001). Patients with no ROP received significantly higher cumulative iron doses than patients with mild ROP (p=0.026). After controlling for birth weight, gestational age, race, ethnicity, 5-minute Apgar score, and ventilator days, the differences in the number of PBRC Txs (p < 0.001) remained statistically significant but the difference in cumulative iron dose was no longer significant (p=0.252). (Table 2)Conclusion(s): In contrast to prior literature, ROP was not associated with the cumulative dose of oral iron in our study. We did find a positive correlation between the occurrence of ROP and number of PRBC transfusions.
Table 1. Demographic and clinical characteristics of the study infants.
 1. Mean ± standard deviation, ANOVA p-value. Groups with different superscript letters are significantly different (Tukey’s HSD test p < 0.05).
1. Mean ± standard deviation, ANOVA p-value. Groups with different superscript letters are significantly different (Tukey’s HSD test p < 0.05). 2. Frequency (%), Fisher’s exact test p-value
3. Median (inter-quartile range), Kruskal-Wallis test p-value. Groups with different letters are significantly different (Tukey’s HSD test p < 0.05).
Figure 1. Number of PRBC transfusions and cumulative iron dose among the study infants during first 2 postnatal months.
.jpg)
