Global Neonatal & Children's Health
Category: Abstract Submission
Global Child and Adolescent Health I
136 - Characterizing Empiric Antimicrobials Among Newborns in Tertiary Centers in Sub-Saharan Africa
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 136
Publication Number: 136.111
Publication Number: 136.111
Grace Rushton, Indiana University School of Medicine, Indianapolis, IN, United States; Osayame A. Ekhaguere, Indiana University School of Medicine, Carmel, IN, United States

Grace E. Rushton, BS
Fourth-year medical student
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Antimicrobial resistance has become a rising public health concern in low and middle-income countries; however, data on the patterns of drug utilization in these countries remains limited.
Objective: Characterizing first-line antimicrobial usage in newborns managed in low-resource settings to provide insight into current and subsequent antimicrobial resistance.
Design/Methods: Retrospective analysis on prospectively collected clinical data on pregnancy, delivery and neonatal intensive care (NICU) from all newborns admitted to three tertiary center NICUs in Nigeria from July 2017 to May 2021. We provide summary statistics on the first line antimicrobials used after birth or admission.
Results: There were 6,186 NICU admissions, 4,471 (72%) underwent a sepsis work-up and 4,264 (95%) were started on antimicrobials. The most commonly prescribed agents were Amikacin (49%), Gentamycin (40%), Ampicillin/Sulbactam (36%), Amoxicillin/Clavulanic acid (31%), and Cefotaxime (26%). Antifungal agents were prescribed to 6.3% and anti-malarial agents to 9.1%. The median length of antimicrobial course was 6 days (IQR = 3—9).
Of those who had a sepsis work-up, only 398 (8.9%) had a positive culture with a total of 434 organisms identified. The most common organisms were Staphylococcus aureus (27%), coagulase negative Staphylococcus (11%), Klebsiella pneumoniae (8%), Escherichia coli (6%), and Pseudomonas aeruginosa (3%). There were 19 fungal isolates (4%). 400 newborns were tested for malaria during the sepsis evaluation with a 54% positive rate, all with Falciparum.
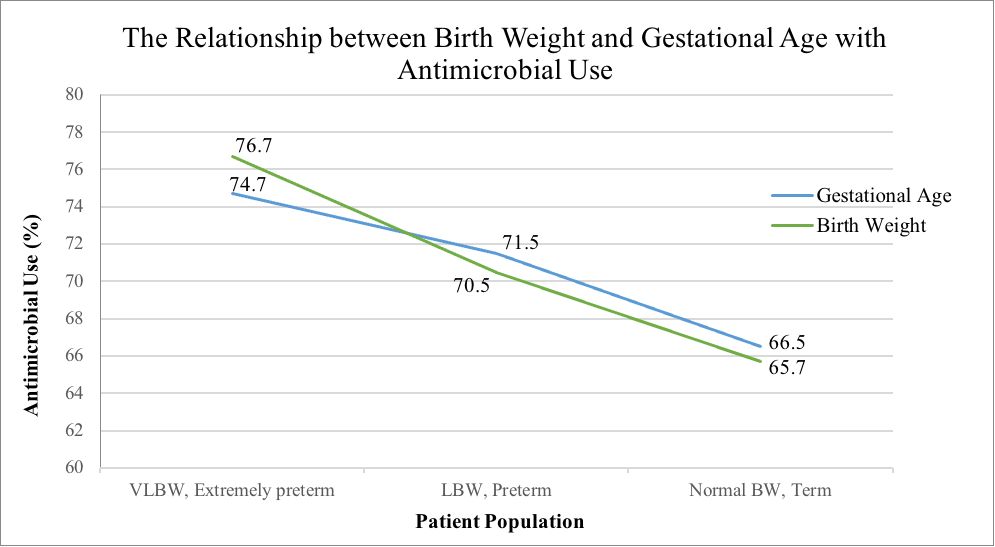
Analysis of gestational age and birth weight both revealed populations with increased rates of antimicrobial use. There was a linear, inverse relationship between birth weight and antimicrobial usage with 76.8% of VLBW neonates, 70.5% of LBW neonates, and 65.7% of normal birth weight neonates started on antimicrobials. There was similarly a linear inverse relationship between gestational age and antimicrobial usage with 74.7% of extremely preterm neonates, 71.5% of preterm neonates, and 66.5% of term neonates started on antimicrobials. Both of these trends were statistically significant with p < .001.Conclusion(s): Empiric antimicrobials among newborns born or admitted into tertiary centers in Nigeria include antibiotics, antifungals and antimalarials. Despite culture positivity being low, antibiotic exposure is high, and the empiric antibiotics used in this sub-Saharan African country would constitute second or third-line antibiotics in high-income countries. Research on the antimicrobial resistance pattern will inform the required antibiotic stewardship.
Grace Rushton CVGR Curriculum Vitae 2021.pdf
The Relationship between Birth Weight and Gestational Age with Antimicrobial Use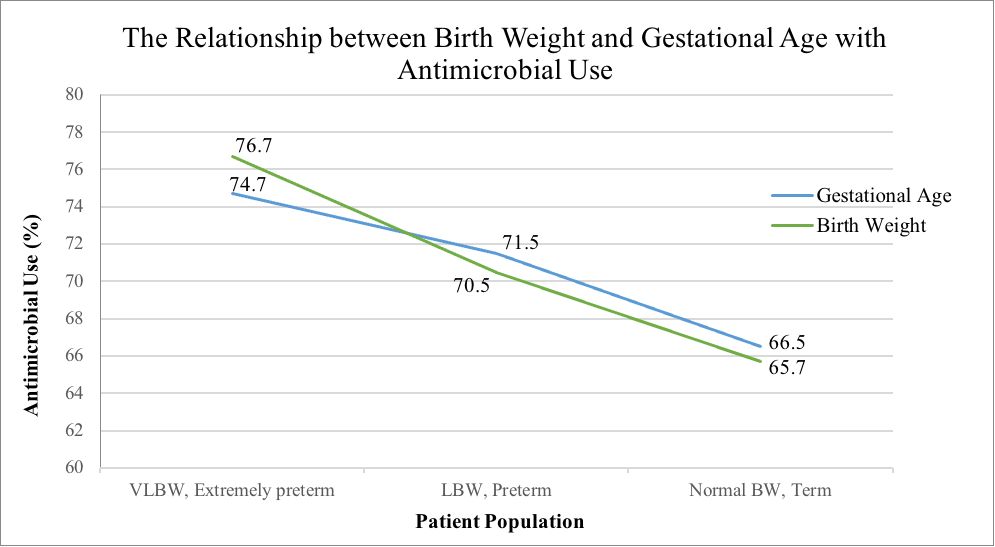
Objective: Characterizing first-line antimicrobial usage in newborns managed in low-resource settings to provide insight into current and subsequent antimicrobial resistance.
Design/Methods: Retrospective analysis on prospectively collected clinical data on pregnancy, delivery and neonatal intensive care (NICU) from all newborns admitted to three tertiary center NICUs in Nigeria from July 2017 to May 2021. We provide summary statistics on the first line antimicrobials used after birth or admission.
Results: There were 6,186 NICU admissions, 4,471 (72%) underwent a sepsis work-up and 4,264 (95%) were started on antimicrobials. The most commonly prescribed agents were Amikacin (49%), Gentamycin (40%), Ampicillin/Sulbactam (36%), Amoxicillin/Clavulanic acid (31%), and Cefotaxime (26%). Antifungal agents were prescribed to 6.3% and anti-malarial agents to 9.1%. The median length of antimicrobial course was 6 days (IQR = 3—9).
Of those who had a sepsis work-up, only 398 (8.9%) had a positive culture with a total of 434 organisms identified. The most common organisms were Staphylococcus aureus (27%), coagulase negative Staphylococcus (11%), Klebsiella pneumoniae (8%), Escherichia coli (6%), and Pseudomonas aeruginosa (3%). There were 19 fungal isolates (4%). 400 newborns were tested for malaria during the sepsis evaluation with a 54% positive rate, all with Falciparum.
Analysis of gestational age and birth weight both revealed populations with increased rates of antimicrobial use. There was a linear, inverse relationship between birth weight and antimicrobial usage with 76.8% of VLBW neonates, 70.5% of LBW neonates, and 65.7% of normal birth weight neonates started on antimicrobials. There was similarly a linear inverse relationship between gestational age and antimicrobial usage with 74.7% of extremely preterm neonates, 71.5% of preterm neonates, and 66.5% of term neonates started on antimicrobials. Both of these trends were statistically significant with p < .001.Conclusion(s): Empiric antimicrobials among newborns born or admitted into tertiary centers in Nigeria include antibiotics, antifungals and antimalarials. Despite culture positivity being low, antibiotic exposure is high, and the empiric antibiotics used in this sub-Saharan African country would constitute second or third-line antibiotics in high-income countries. Research on the antimicrobial resistance pattern will inform the required antibiotic stewardship.
Grace Rushton CVGR Curriculum Vitae 2021.pdf
The Relationship between Birth Weight and Gestational Age with Antimicrobial Use