Neonatal General
Category: Abstract Submission
Neonatology General 7: ROP - Endocrine
432 - Corticosteroid use and adrenal suppression risk in very low birth weight (VLBW) neonates.
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 432
Publication Number: 432.137
Publication Number: 432.137
Samuel E. Hagman, University of South Dakota, Sanford School of Medicine, sioux falls, SD, United States; Maya R. Gogoi, University of South Dakota Sanford School of Medicine, Libertyville, IL, United States; Sarah Jackson, Mayo clinic, Rochester, MN, United States; Michelle L. Baack, University of South Dakota, Sanford School of Medicine, Sioux Falls, SD, United States; Jacquelyn E. Grev, Sanford Children's Hospital, Sioux Falls, SD, United States

Samuel E. Hagman, DO
Resident
University of South Dakota, Sanford School of Medicine
sioux falls, South Dakota, United States
Presenting Author(s)
Background: Adrenal insufficiency (AI), or inability to make endogenous steroids, can be life threatening and requires stress dosing during acute stress. Chronic use of systemic corticosteroids (SCS) can suppress the normal hypothalamic-pituitary-adrenal (HPA) axis, causing iatrogenic AI. Unfortunately, very low birth weight (VLBW) infants often require SCS and/or inhaled corticosteroids (ICS) in order to survive. There is an urgent need to uncover exposure-related risk factors to guide judicial steroid use and identify those that need stress dose education prior to discharge.
Objective: Identify attributable risks of AI in VLBW infants ready for discharge from the NICU.
Design/Methods: This single center, retrospective, case-control study collected Electronic Medical Record (EMR) data to correlate the association of steroid exposure and AI diagnosis in VLBW infants. The study included VLBW infants, < 1500g, admitted to Sanford Boekelheide NICU between January 1, 2015 and December 31, 2020. Cases had an ICD 9 or ICD10 code of AI. Controls were GA-matched infants without the recorded diagnosis. Non-viable infants, infants with congenital adrenal hyperplasia, or HPA axis pathology were excluded. Deidentified data was systematically collected to a REDCAP data base and GraphPad PRISM8 Software was used to compute group differences by Student’s T-Test, odd’s ratios (OR) by Chi-squared or Fisher’s exact test and likelihood ratios (LR) by Wilson-Brown method; significance was set at p < 0.05.
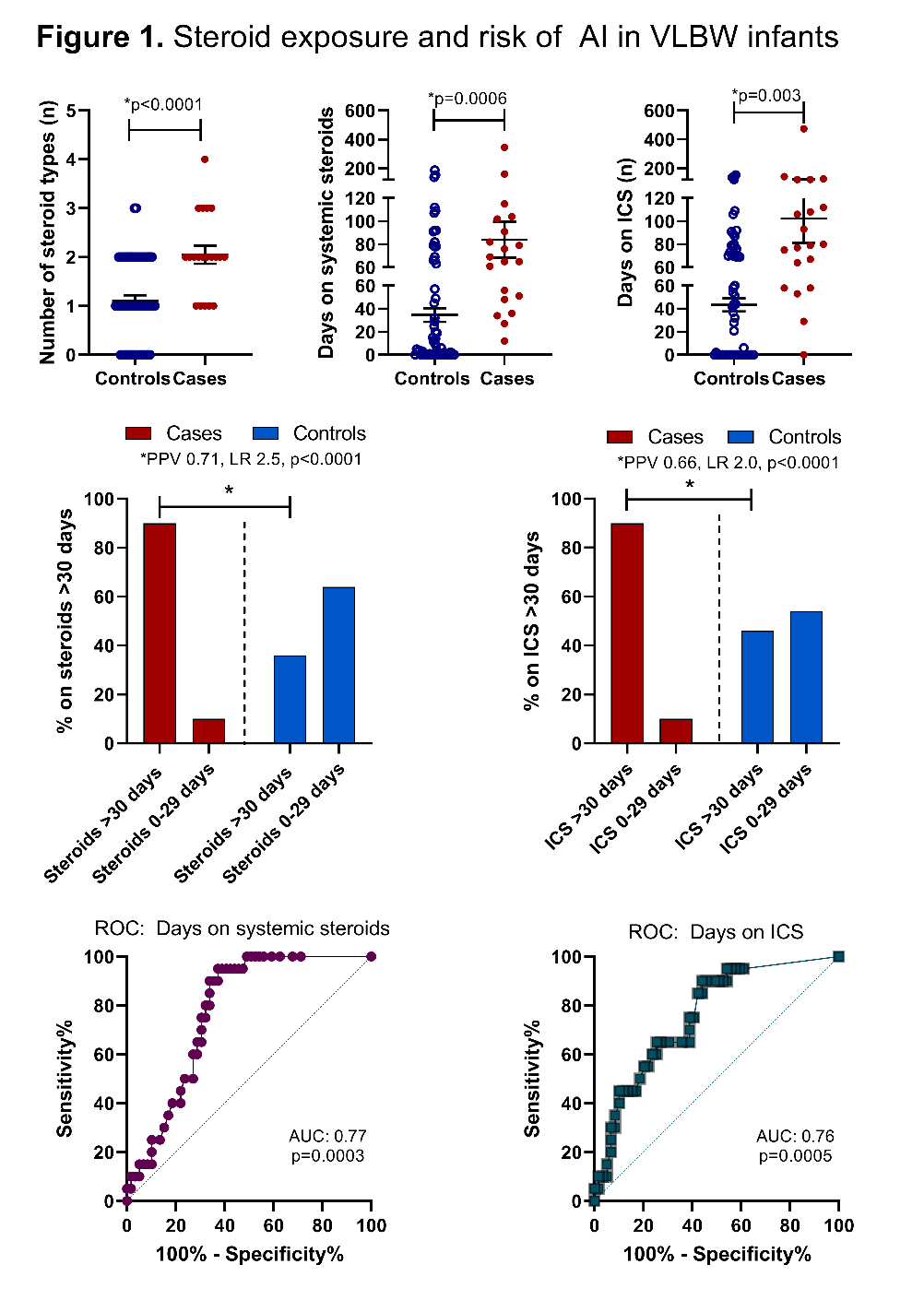
Results: A total of 79 infants were studied, 20 cases and 59 controls. With GA-matching, demographic factors (sex, birthweight, race/ethnicity, IUGR, APGARs) were not different between groups, but non-white infants had a trend to higher risk of AI (OR 3.2, p=0.08). Both SCS and ICS exposure increased the risk of AI as shown in Table 1 and Figure 1. Specifically, days on SCS and ICS were higher in cases and the likelihood of AI increased with treatment for hypotension and steroid use >30 days (sensitivity 0.90, specificity 0.64, LR 2.5, p < 0.0001 for SCS; sensitivity 0.90, specificity 0.54, LR 1.97, p < 0.0005 for ICS). Being on high-dose Flovent, hydrocortisone, methylprednisone, or multiple SCS increased odds of AI, but antenatal corticosteroids, prednisolone or dexamathasone exposure did not.Conclusion(s): While further prospective studies, especially surrounding systemic absorption of ICS are needed, VLBW infants on SCS or high-dose ICS > 30 days seem to be at the highest risk for AI and should be screened by ACTH stimulation test prior to discharge.
PDF Current Hagman CV With Explanations.pdf
Steroid exposure and risk of AI in VLBW infants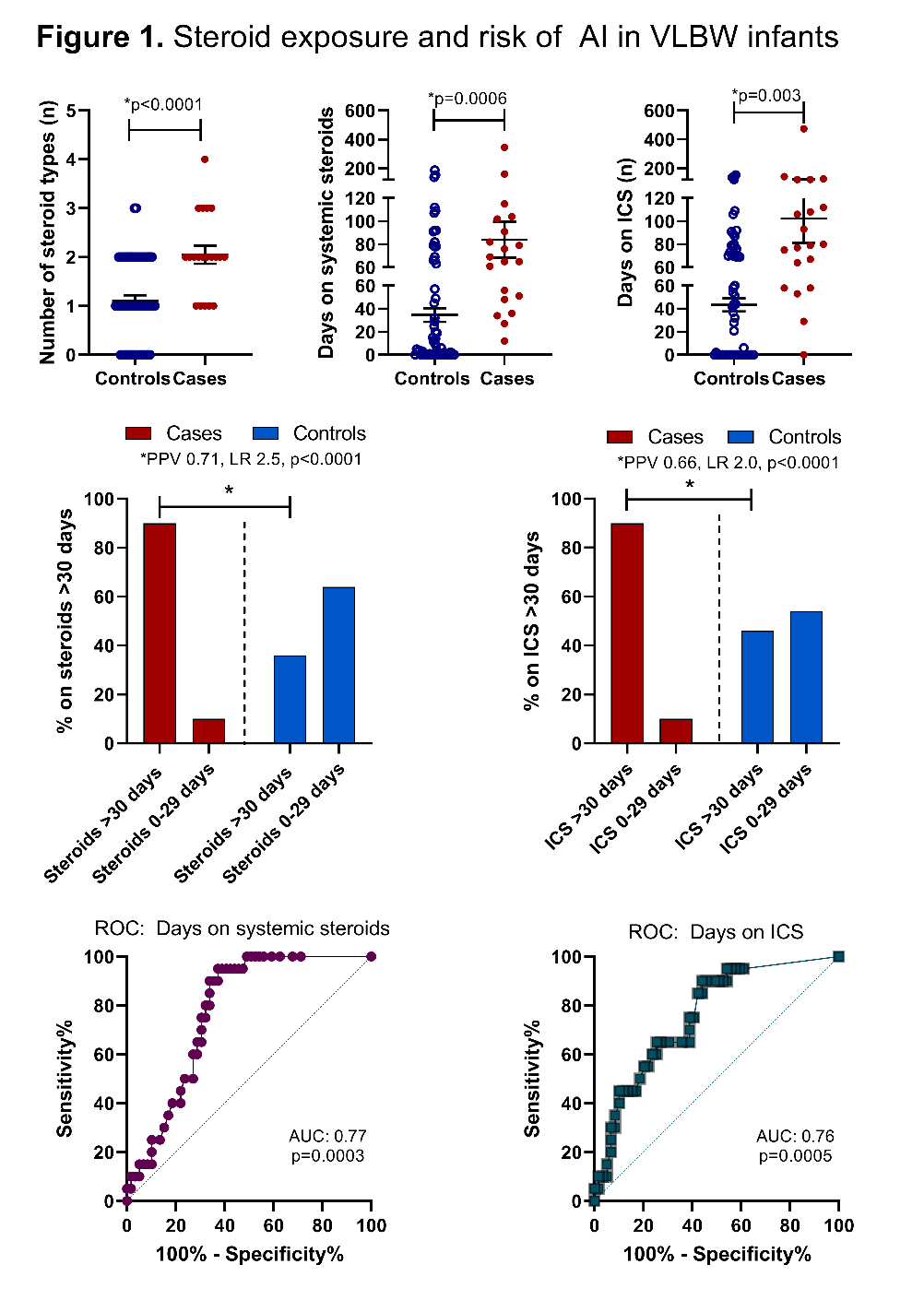
Objective: Identify attributable risks of AI in VLBW infants ready for discharge from the NICU.
Design/Methods: This single center, retrospective, case-control study collected Electronic Medical Record (EMR) data to correlate the association of steroid exposure and AI diagnosis in VLBW infants. The study included VLBW infants, < 1500g, admitted to Sanford Boekelheide NICU between January 1, 2015 and December 31, 2020. Cases had an ICD 9 or ICD10 code of AI. Controls were GA-matched infants without the recorded diagnosis. Non-viable infants, infants with congenital adrenal hyperplasia, or HPA axis pathology were excluded. Deidentified data was systematically collected to a REDCAP data base and GraphPad PRISM8 Software was used to compute group differences by Student’s T-Test, odd’s ratios (OR) by Chi-squared or Fisher’s exact test and likelihood ratios (LR) by Wilson-Brown method; significance was set at p < 0.05.
Results: A total of 79 infants were studied, 20 cases and 59 controls. With GA-matching, demographic factors (sex, birthweight, race/ethnicity, IUGR, APGARs) were not different between groups, but non-white infants had a trend to higher risk of AI (OR 3.2, p=0.08). Both SCS and ICS exposure increased the risk of AI as shown in Table 1 and Figure 1. Specifically, days on SCS and ICS were higher in cases and the likelihood of AI increased with treatment for hypotension and steroid use >30 days (sensitivity 0.90, specificity 0.64, LR 2.5, p < 0.0001 for SCS; sensitivity 0.90, specificity 0.54, LR 1.97, p < 0.0005 for ICS). Being on high-dose Flovent, hydrocortisone, methylprednisone, or multiple SCS increased odds of AI, but antenatal corticosteroids, prednisolone or dexamathasone exposure did not.Conclusion(s): While further prospective studies, especially surrounding systemic absorption of ICS are needed, VLBW infants on SCS or high-dose ICS > 30 days seem to be at the highest risk for AI and should be screened by ACTH stimulation test prior to discharge.
PDF Current Hagman CV With Explanations.pdf
Steroid exposure and risk of AI in VLBW infants