Neonatal General
Category: Abstract Submission
Neonatology General 1: GI - Growth - Nutrition
261 - Developing a Multivariable Prediction Model for Postnatal Growth Failure in Preterm Neonates
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 261
Publication Number: 261.131
Publication Number: 261.131
Dara Azuma, Tufts Medical Center, Boston, MA, United States; Jaclyn Boulais, Tufts Childrens Hospital, Jamaica Plain, MA, United States; Caryn Hamilton, Tufts Childrens Hospital, Boston, MA, United States
- DA
Dara Azuma, MD
Neonatologist
Tufts Medical Center
Boston, Massachusetts, United States
Presenting Author(s)
Background: Up to half of all VLBW infants admitted to the NICU develop postnatal growth failure (PGF). PGF has been associated with neurodevelopmental delay and long term cardiometabolic morbidities.
Objective: We aimed to develop a multivariable prediction model identifying preterm infants at risk for PGF using prenatal characteristics as well as clinical data from the first 3 days of life.
Design/Methods: Infants born between 24 0/7 weeks and 34 6/7 weeks gestation admitted to Tufts Medical Center NICU within the first month of life from 2010-2020 were included in our study. The outcome of the model was PGF, defined as a discharge weight < 10th percentile for PMA using the INTERGROWTH-21 project postnatal growth curves. Variables considered for model inclusion were birth weight in grams, birth weight percentile, infant sex, gestational age at birth, multiple gestations, antenatal steroids, 5 minute APGAR, intubation required in the delivery room, early onset sepsis, maternal race, and surfactant administration. We used multivariable logistic regression to develop a model to predict PGF. A backwards elimination variable selection strategy was used to identify predictors included in the final model using Akaike information criterion. Internal validation of the model building procedure was performed using 500 bootstrap samples. Uniform shrinkage was performed to avoid overfitting.
Results: Of the 2248 eligible infants, 24.5% developed PGF. Variables selected for inclusion in our model were birth weight percentile, infant sex, gestational age at birth, multiple gestation, intubation during initial resuscitation, and early onset sepsis. The final model had a corrected C-statistic of 0.926. Internal validation of the model building procedure yielded an identical model. The final model after validation and uniform shrinkage is as follows: Logit (PGF)= 5.299- 0.010(BW percentile)+0.826(Infant sex)-0.017(Gestational age at birth in days)+ 0.218(Multiple gestation)+0.393(Required intubation in delivery room)-1.454(Early onset bacterial sepsis). Conclusion(s): We were able to develop a model to accurately predict PGF in premature neonates. Prior studies have demonstrated the importance of early nutrition on growth velocity in the NICU so we believe this model will be helpful in identifying infants that would benefit most from optimal nutrition during their hospitalization and possibly improve outcomes if nutrition is maximized and prioritized from the first week of life.
Table 1. Patient Characteristics By Outcome of Postnatal Growth Failure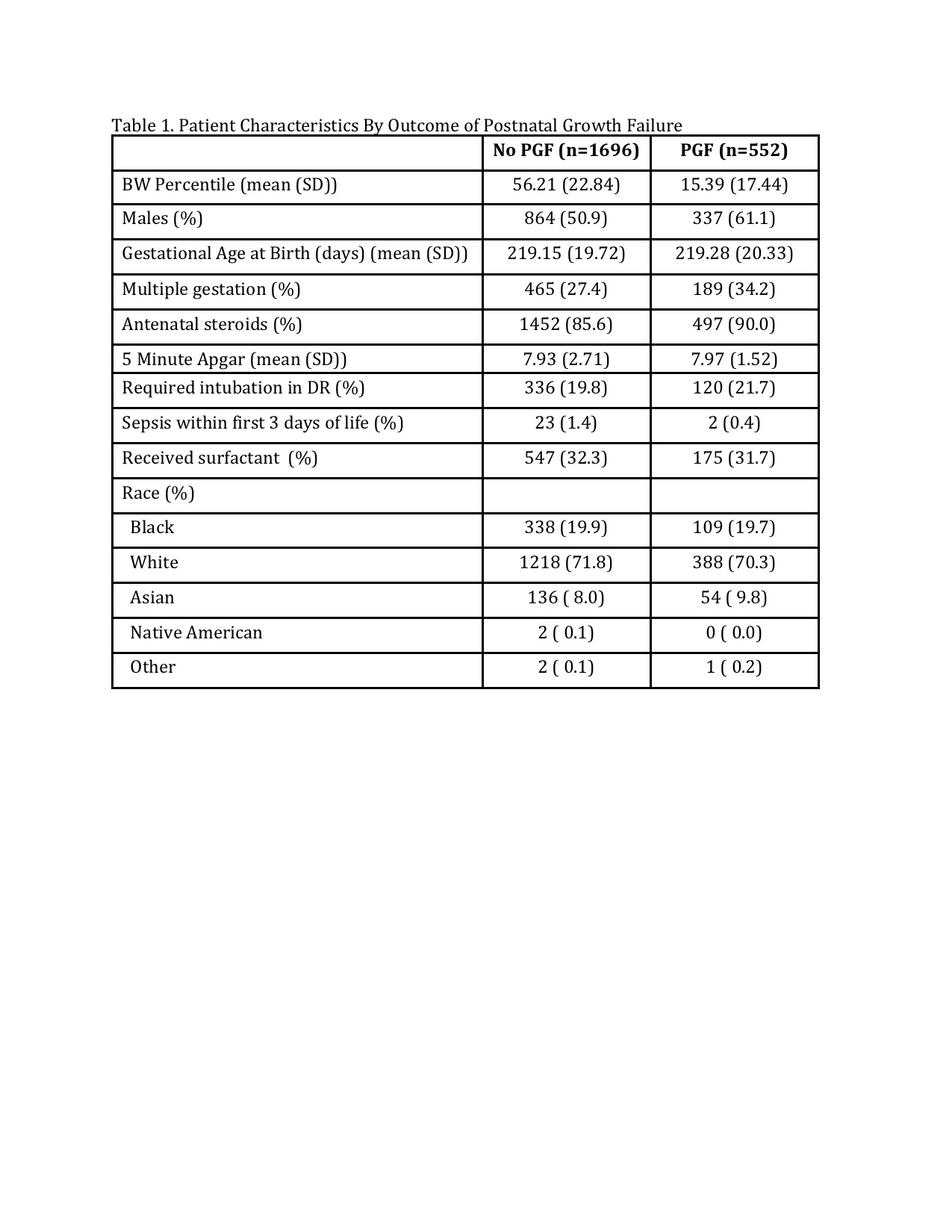
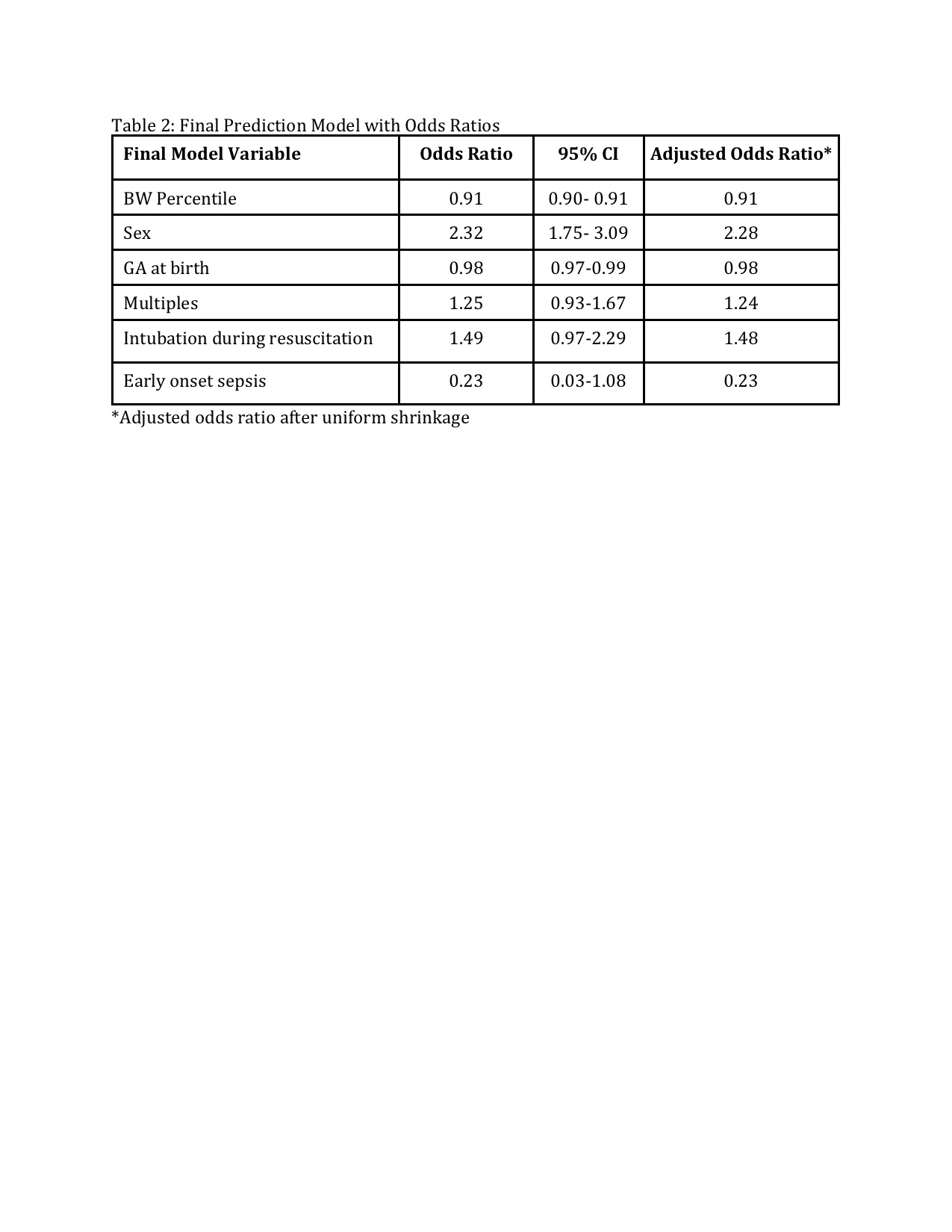
Table 2: Final Prediction Model with Odds Ratios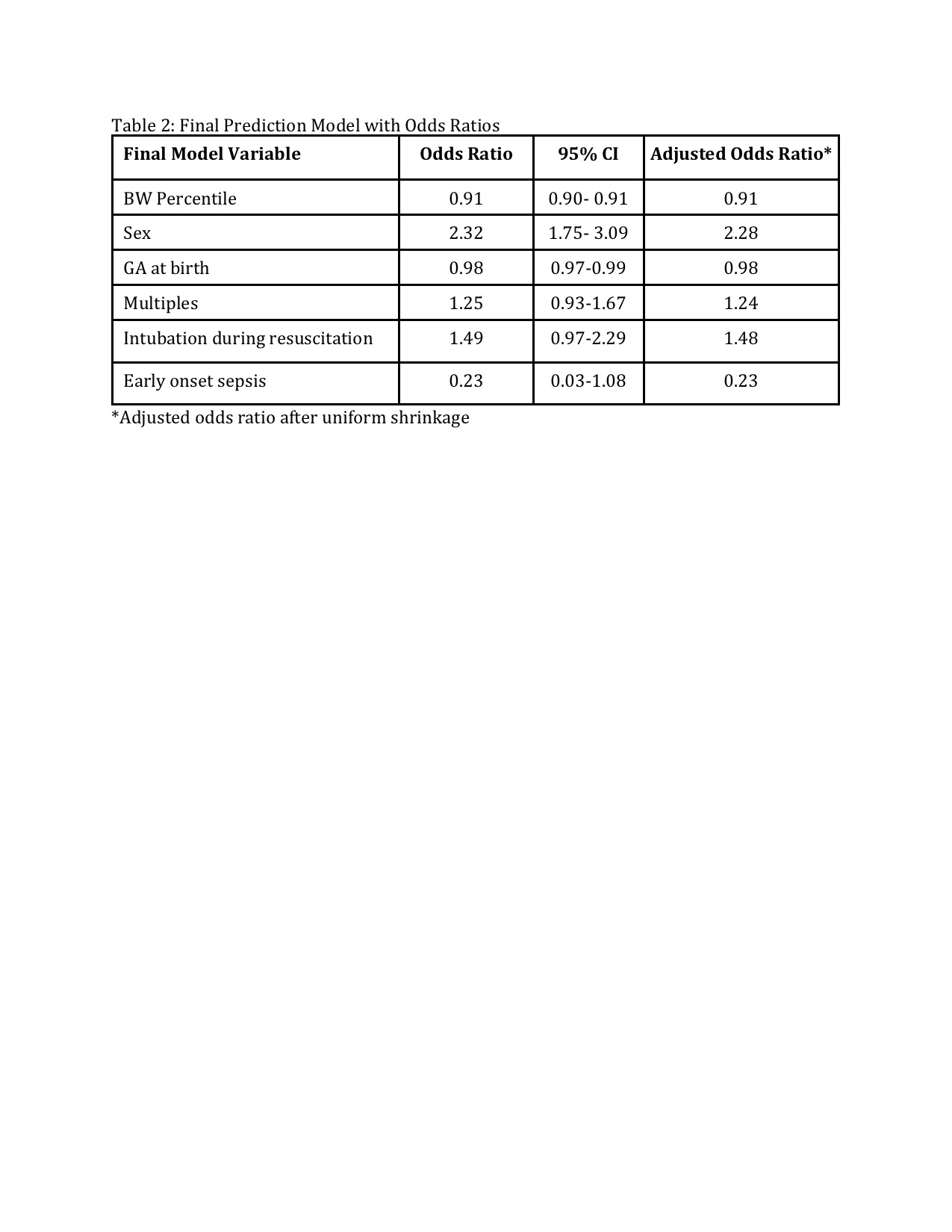
Objective: We aimed to develop a multivariable prediction model identifying preterm infants at risk for PGF using prenatal characteristics as well as clinical data from the first 3 days of life.
Design/Methods: Infants born between 24 0/7 weeks and 34 6/7 weeks gestation admitted to Tufts Medical Center NICU within the first month of life from 2010-2020 were included in our study. The outcome of the model was PGF, defined as a discharge weight < 10th percentile for PMA using the INTERGROWTH-21 project postnatal growth curves. Variables considered for model inclusion were birth weight in grams, birth weight percentile, infant sex, gestational age at birth, multiple gestations, antenatal steroids, 5 minute APGAR, intubation required in the delivery room, early onset sepsis, maternal race, and surfactant administration. We used multivariable logistic regression to develop a model to predict PGF. A backwards elimination variable selection strategy was used to identify predictors included in the final model using Akaike information criterion. Internal validation of the model building procedure was performed using 500 bootstrap samples. Uniform shrinkage was performed to avoid overfitting.
Results: Of the 2248 eligible infants, 24.5% developed PGF. Variables selected for inclusion in our model were birth weight percentile, infant sex, gestational age at birth, multiple gestation, intubation during initial resuscitation, and early onset sepsis. The final model had a corrected C-statistic of 0.926. Internal validation of the model building procedure yielded an identical model. The final model after validation and uniform shrinkage is as follows: Logit (PGF)= 5.299- 0.010(BW percentile)+0.826(Infant sex)-0.017(Gestational age at birth in days)+ 0.218(Multiple gestation)+0.393(Required intubation in delivery room)-1.454(Early onset bacterial sepsis). Conclusion(s): We were able to develop a model to accurately predict PGF in premature neonates. Prior studies have demonstrated the importance of early nutrition on growth velocity in the NICU so we believe this model will be helpful in identifying infants that would benefit most from optimal nutrition during their hospitalization and possibly improve outcomes if nutrition is maximized and prioritized from the first week of life.
Table 1. Patient Characteristics By Outcome of Postnatal Growth Failure
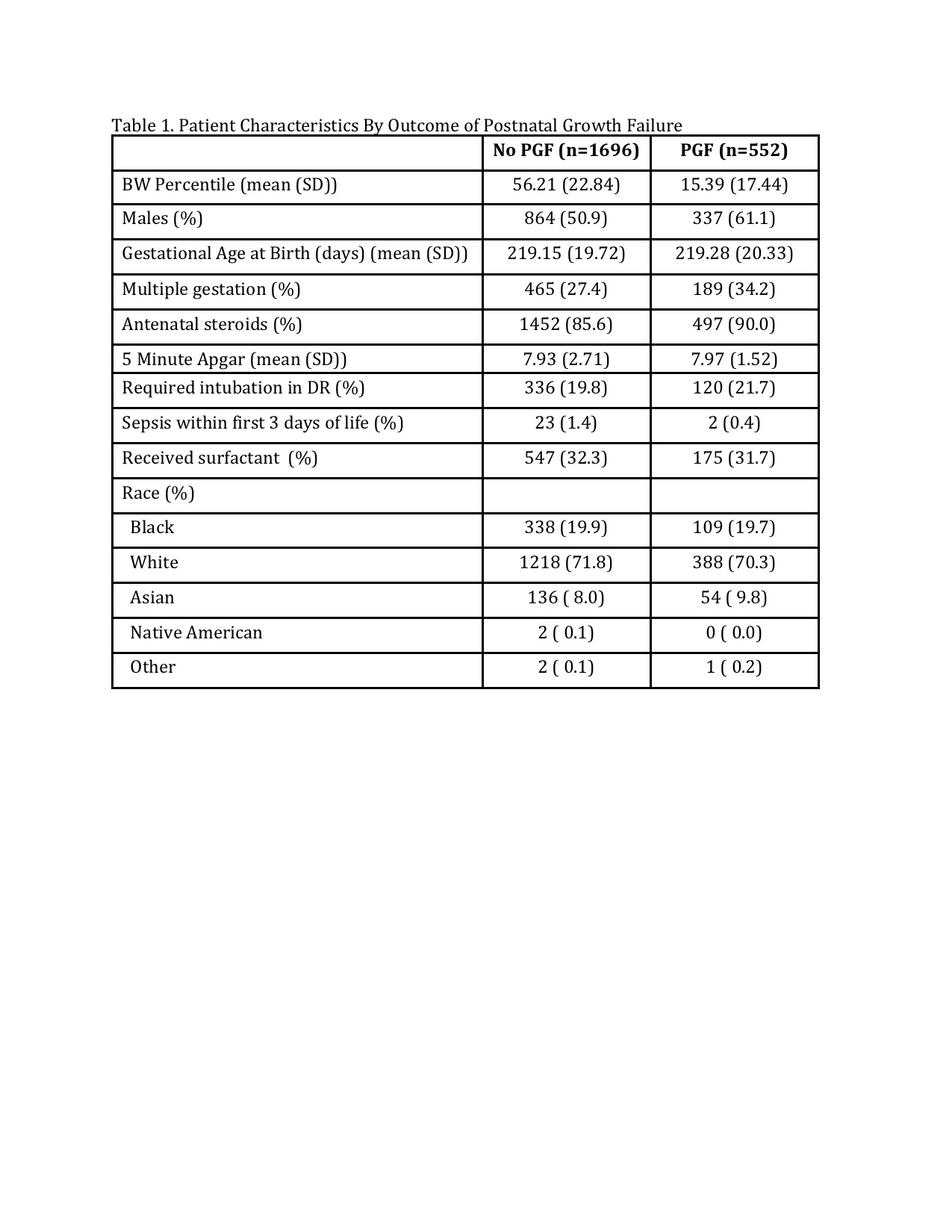
Table 2: Final Prediction Model with Odds Ratios