Critical Care
Category: Abstract Submission
Critical Care I
23 - Differences in Hemostatic Sampling and Trauma-induced Coagulopathy by Pediatric Age Groups
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 23
Publication Number: 23.102
Publication Number: 23.102
Shyam J. Deshpande, University of Washington School of Medicine, Seattle, WA, United States; Hamilton C. Tsang, University Of Washington, Seattle, WA, United States; Jimmy Phuong, University of Washington School of Medicine, Seattle, WA, United States; Rida Hasan, University of Washington, Seattle, WA, United States; John R. Hess, University of Washington School of Medicine, Seattle, WA, United States; Monica S. Vavilala, Harborview Injury prevention and Resesarch Center, Seattle, WA, United States; Lynn G. Stansbury, U W Harborview Injury Prev and Research, SEATTLE, WA, United States
- SD
Shyam J. Deshpande, MD, FAAP
Resident in Anesthesiology & Pain Medicine
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background: Coagulopathy occurs in pediatric trauma, including in those with isolated traumatic brain injury (TBI). Developmental hemostasis occurs through childhood, but how developmental differences affect trauma-induced coagulopathy (TIC) among various age groups is unclear. Although older children have been reported to have the highest frequency of TIC, phenotyping across age groups historically uses a single reference range and poorly controlled for injury severity.
Objective: Comparative analysis of hemostatic sampling and TIC variations by pediatric age-group
Design/Methods: A retrospective cohort study of all trauma admissions age < 18y to a large, regional Level 1 pediatric trauma center, 2015–2020. We evaluated INR, aPTT, platelet count, and fibrinogen at two time intervals (trauma center admission; over first 72h) with Trauma Registry demographic and injury severity (ISS) data. We grouped results by ages < 1, 1-4, 5-9, 10-14, and 15-17y. Frequency of coagulopathy was determined using published age-specific laboratory reference ranges. A subgroup analysis of patients with isolated TBI was performed.
Results: 2604 patients met primary inclusion criteria, 331 (12.7%) of whom had isolated TBI. Admission results for INR, aPTT, platelet count, and fibrinogen were available for 74%, 72%, 83%, and 7% of patients. Children < 1y were least likely to be tested for TIC even among the most injured (INR-32%, aPTT-32%, platelet count-50%, fibrinogen 3%) and those 15-17y were the most likely to be tested (INR-85%, aPTT-83%, platelet count-91%, fibrinogen-11%). For all patients, higher ISS was associated with worse coagulation results at both time intervals. The average difference between ISS >25 and < 9 was INR 0.43, aPTT 9s, and platelet count -40k. Younger children had higher frequency of coagulopathy than older children at both time intervals, even within injury severity group (i.e. coagulopathy by platelet count: < 1y 8%, 1-4y 20%, 5-9y 24% vs 10-14y 10%, 15-17y 4%).Conclusion(s): Contrary to prior work, this study shows a higher frequency of coagulopathy in younger pediatric age groups compared to older children. However, we demonstrate that there is significant sampling bias in clinical data collection, particularly in the youngest children, acquisition of fibrinogen measurements, and variations related to injury severity. Recommendations for hemostatic sampling and treatments are needed in pediatric trauma.
Figure 1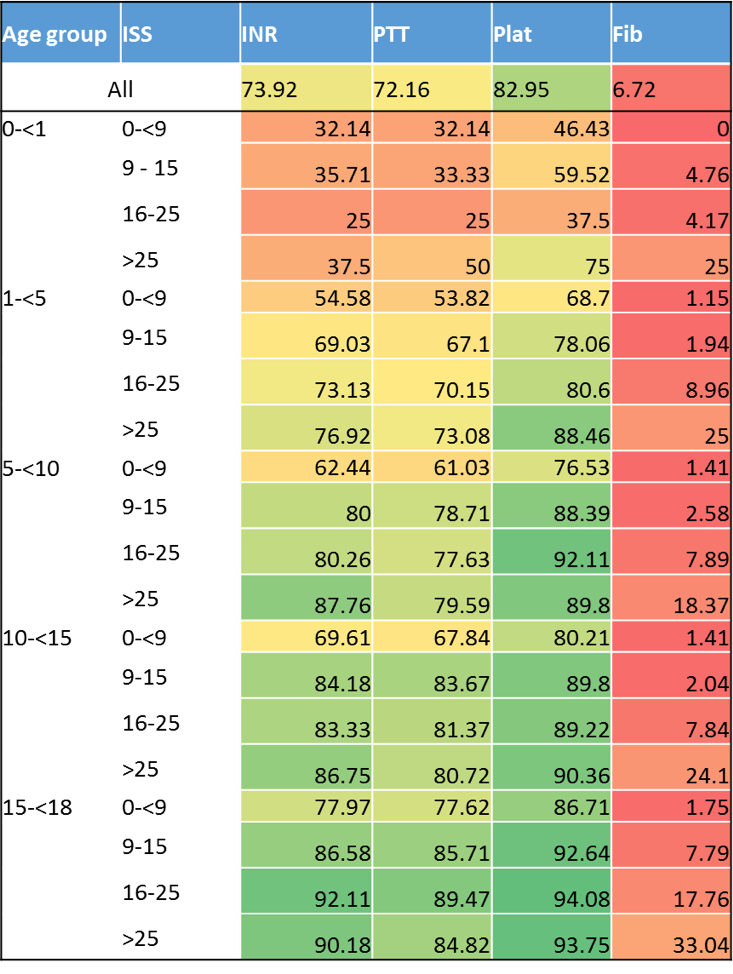 Laboratory study data availability at the time of trauma admission by age group and ISS group, demonstrating the relative infrequency of study acquisition in the youngest age group, as well as the paucity of fibrinogen values obtain. Cell color fill scaled by percentage, with green cells representing the highest data availability and red cells representing the lowest data availability.
Laboratory study data availability at the time of trauma admission by age group and ISS group, demonstrating the relative infrequency of study acquisition in the youngest age group, as well as the paucity of fibrinogen values obtain. Cell color fill scaled by percentage, with green cells representing the highest data availability and red cells representing the lowest data availability.
Figure 2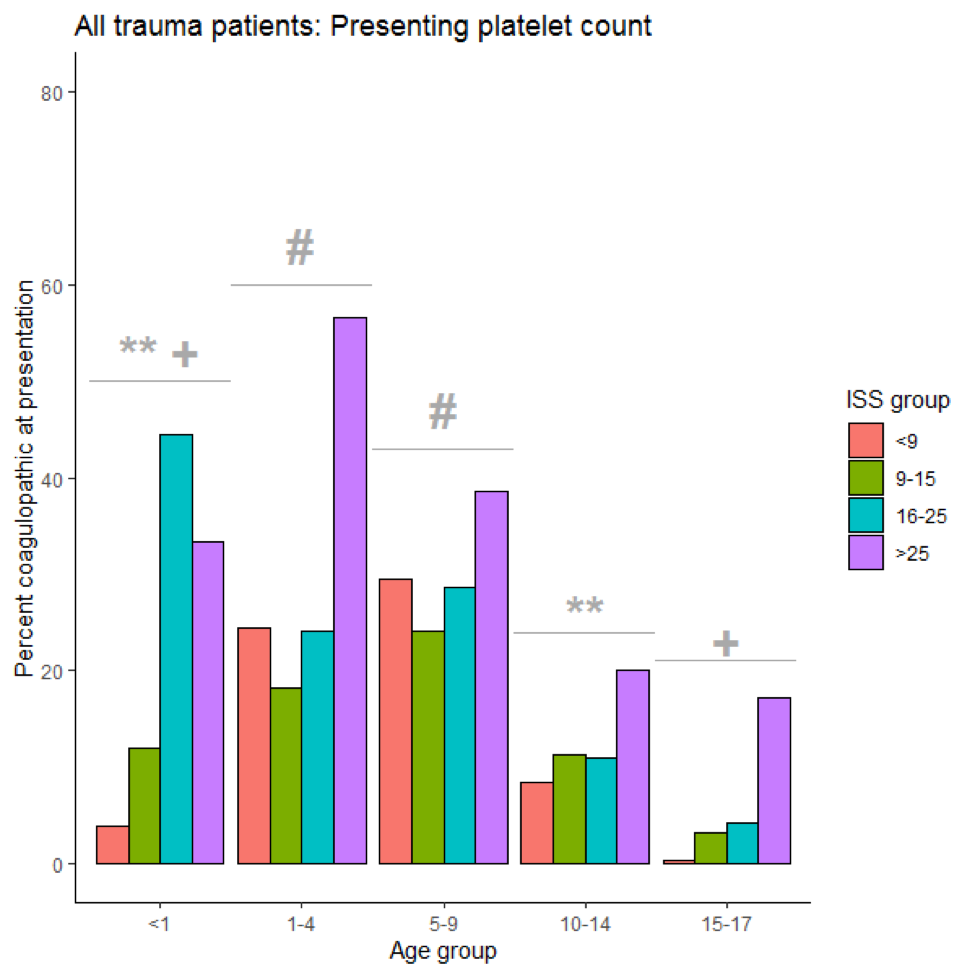 Frequency of coagulopathy defined by platelet count below age-specific reference ranges at the time of trauma admission by pediatric age group and ISS group, demonstrating higher frequency of coagulopathy in younger children compared to older children. Symbols above age groups represent statistically unique groups in frequency of coagulopathy (eg. frequency of coagulopathy for 1-4 is statistically higher than < 1y, 10-14y, and 15-17y and not statistically different from 5-9y).
Frequency of coagulopathy defined by platelet count below age-specific reference ranges at the time of trauma admission by pediatric age group and ISS group, demonstrating higher frequency of coagulopathy in younger children compared to older children. Symbols above age groups represent statistically unique groups in frequency of coagulopathy (eg. frequency of coagulopathy for 1-4 is statistically higher than < 1y, 10-14y, and 15-17y and not statistically different from 5-9y).
Objective: Comparative analysis of hemostatic sampling and TIC variations by pediatric age-group
Design/Methods: A retrospective cohort study of all trauma admissions age < 18y to a large, regional Level 1 pediatric trauma center, 2015–2020. We evaluated INR, aPTT, platelet count, and fibrinogen at two time intervals (trauma center admission; over first 72h) with Trauma Registry demographic and injury severity (ISS) data. We grouped results by ages < 1, 1-4, 5-9, 10-14, and 15-17y. Frequency of coagulopathy was determined using published age-specific laboratory reference ranges. A subgroup analysis of patients with isolated TBI was performed.
Results: 2604 patients met primary inclusion criteria, 331 (12.7%) of whom had isolated TBI. Admission results for INR, aPTT, platelet count, and fibrinogen were available for 74%, 72%, 83%, and 7% of patients. Children < 1y were least likely to be tested for TIC even among the most injured (INR-32%, aPTT-32%, platelet count-50%, fibrinogen 3%) and those 15-17y were the most likely to be tested (INR-85%, aPTT-83%, platelet count-91%, fibrinogen-11%). For all patients, higher ISS was associated with worse coagulation results at both time intervals. The average difference between ISS >25 and < 9 was INR 0.43, aPTT 9s, and platelet count -40k. Younger children had higher frequency of coagulopathy than older children at both time intervals, even within injury severity group (i.e. coagulopathy by platelet count: < 1y 8%, 1-4y 20%, 5-9y 24% vs 10-14y 10%, 15-17y 4%).Conclusion(s): Contrary to prior work, this study shows a higher frequency of coagulopathy in younger pediatric age groups compared to older children. However, we demonstrate that there is significant sampling bias in clinical data collection, particularly in the youngest children, acquisition of fibrinogen measurements, and variations related to injury severity. Recommendations for hemostatic sampling and treatments are needed in pediatric trauma.
Figure 1
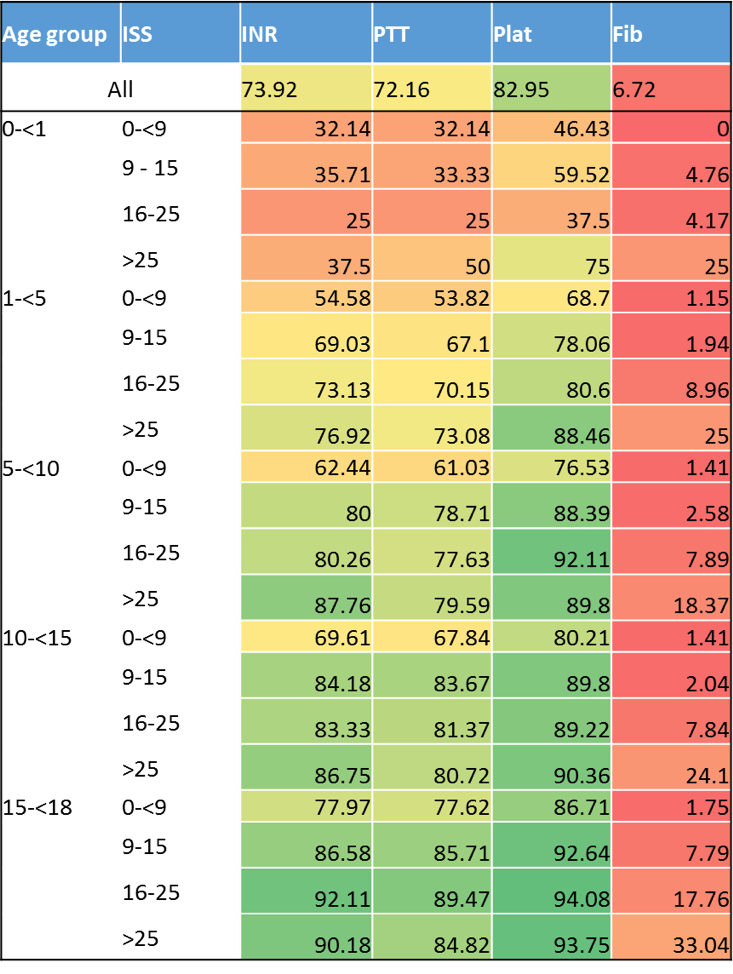 Laboratory study data availability at the time of trauma admission by age group and ISS group, demonstrating the relative infrequency of study acquisition in the youngest age group, as well as the paucity of fibrinogen values obtain. Cell color fill scaled by percentage, with green cells representing the highest data availability and red cells representing the lowest data availability.
Laboratory study data availability at the time of trauma admission by age group and ISS group, demonstrating the relative infrequency of study acquisition in the youngest age group, as well as the paucity of fibrinogen values obtain. Cell color fill scaled by percentage, with green cells representing the highest data availability and red cells representing the lowest data availability.Figure 2
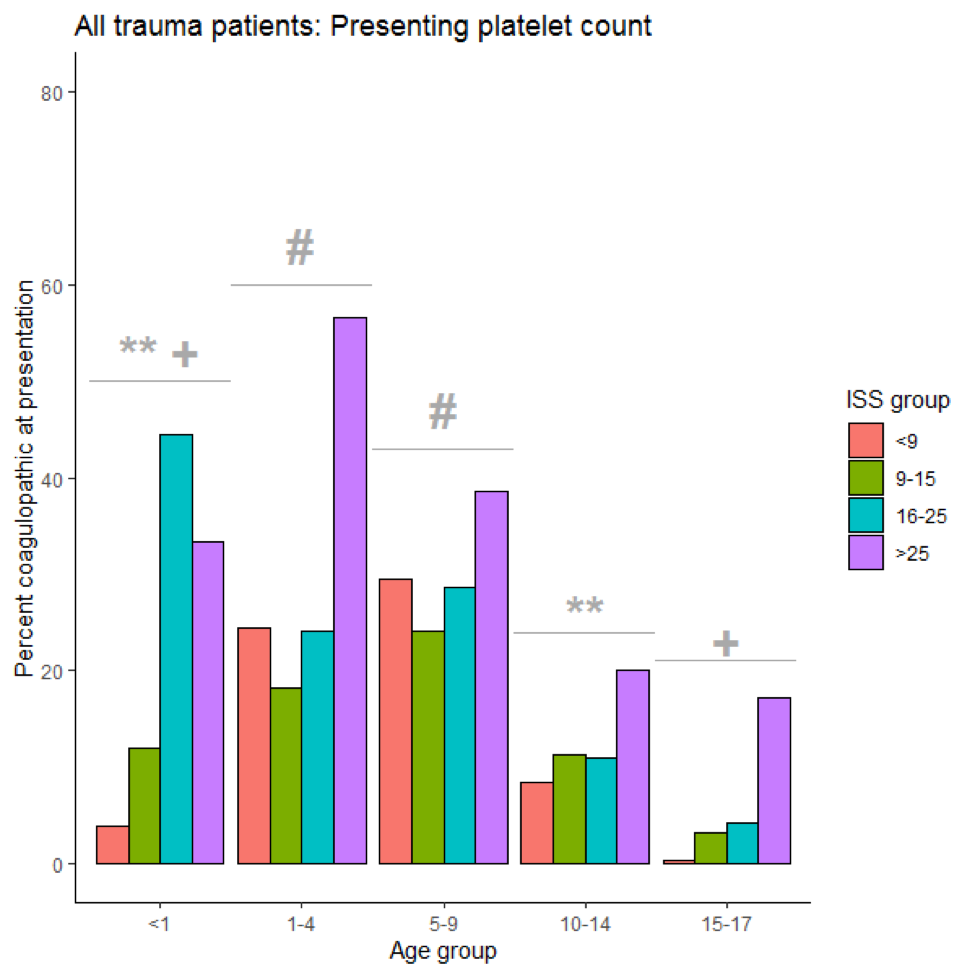 Frequency of coagulopathy defined by platelet count below age-specific reference ranges at the time of trauma admission by pediatric age group and ISS group, demonstrating higher frequency of coagulopathy in younger children compared to older children. Symbols above age groups represent statistically unique groups in frequency of coagulopathy (eg. frequency of coagulopathy for 1-4 is statistically higher than < 1y, 10-14y, and 15-17y and not statistically different from 5-9y).
Frequency of coagulopathy defined by platelet count below age-specific reference ranges at the time of trauma admission by pediatric age group and ISS group, demonstrating higher frequency of coagulopathy in younger children compared to older children. Symbols above age groups represent statistically unique groups in frequency of coagulopathy (eg. frequency of coagulopathy for 1-4 is statistically higher than < 1y, 10-14y, and 15-17y and not statistically different from 5-9y).