Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up I
442 - Effect of NICU to home transition care program (NTC) on breast feeding duration.
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 442
Publication Number: 442.121
Publication Number: 442.121
Shruti Gupta, Yale-New Haven Children's Hospital, Westport, CT, United States; Josette Hartnett, Stamford Health, Stamford, CT, United States; Dana Czuczka, Stamford Health, Westport, CT, United States

Shruti Gupta, MD
Medical Director of Neonatalogy, YNHH Greenwich Hospital
Yale-New Haven Children's Hospital
Westport, Connecticut, United States
Presenting Author(s)
Background: Families are often overwhelmed post neonatal intensive care unit (NICU) discharge and often have less support. Infants are discharged home maternal milk feeding but not fully breastfeeding due to oral feeding immaturity. Therefore, the transition to breastfeeding occurs post-NICU discharge. To continue specialized care post-NICU discharge, a unique NICU to home transition care program (NTC) was designed that included visits with a neonatologist and a lactation consultant a few days after discharge. The visit included observation of a breastfeeding session and providing clear feeding instructions for the mother and pediatrician as the infant transitions from bottle feeding to breast feeding. This included adjustment of human milk fortifiers and any other additives infant was discharged home on as infant transitioned to breast feeding.
Objective: To compare duration of breastfeeding in infants that attended the NTC program to infants that did not attend the program.
Design/Methods: For this study only infants who were receiving maternal milk at NICU discharge were included in both groups. Descriptive data were reported for both groups and a group t-test were performed to compare duration of breastfeeding between NTC and non-NTC cohorts with a chi-square test. Mean and standard deviation (SD) were calculated. An a-priori p-value of (p < 0.05) to denote significance was used for both analyses.
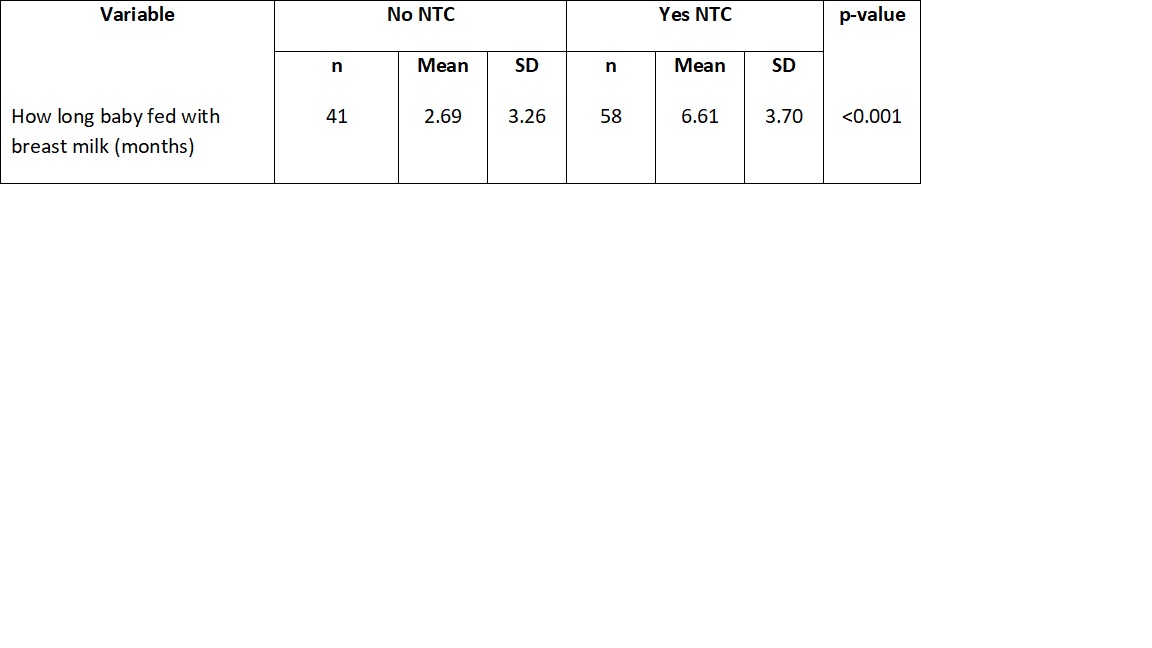
Results: NTC (n = 58) compared to non-NTC participants (n=41) were more preterm at birth but similar in other measures such as multiples, race, ethnicity, and maternal education. NTC participants were statistically more likely to breastfeed longer than non-NTC participants (n=41) (p < 0.001). NTC participants breast-fed on average 6.61 months (SD= 3.70), while their non-NTC counterpart averaged 2.69 months (SD = 3.26) (p-value < 0.001). Participants in NTC were 3.3 times (95% CI 1.6, 6.7) more likely to breastfeed for at least 6 months compared to those who did not attend NTC (58 vs. 17.5%, respectively).
Satisfaction with the NTC program was very high among participants. The majority of NTC participants described the program as useful when transitioning home (96.5%) and as helpful in sustaining breastfeeding or pumping especially when they wanted to stop or give up (87.93%). In addition, 99.1% described it as useful to have a neonatologist present at the NTC visits. Conclusion(s): Programmatic post discharge help was positively received and related to significantly increased breastfeeding post-NICU discharge.
Breast feeding Duration in both NTC and Non NTC groups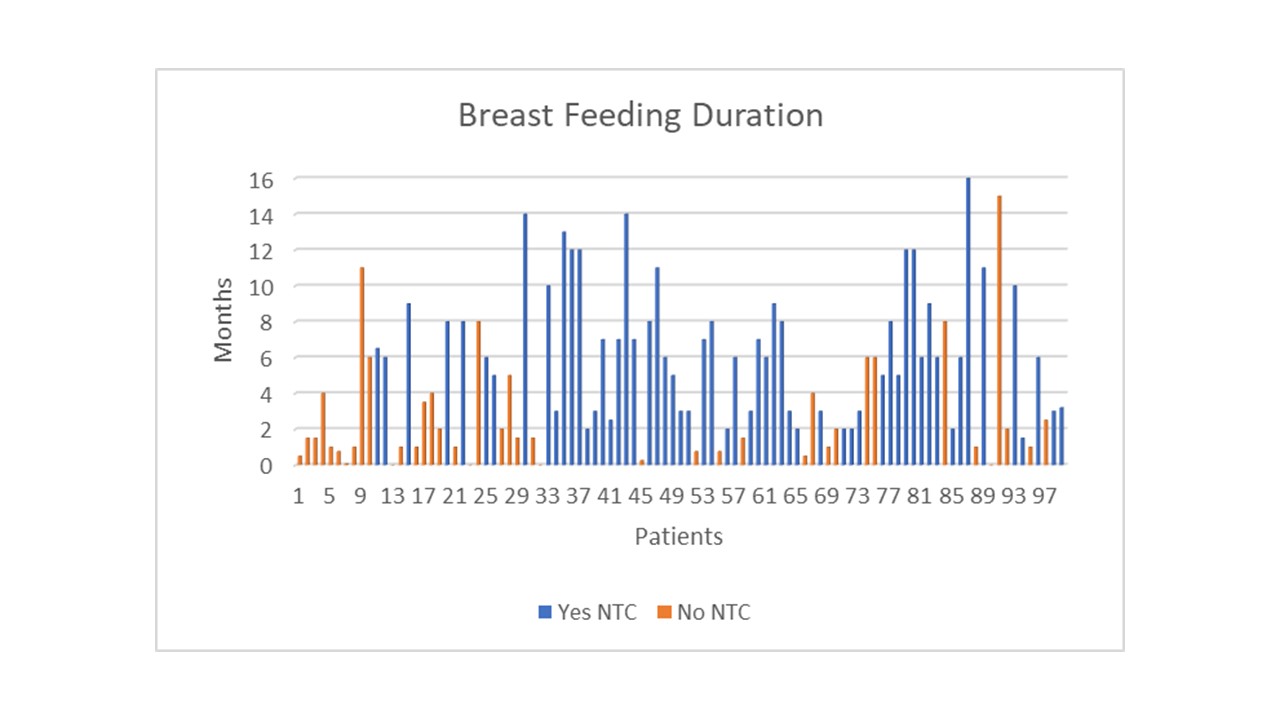
Difference in duration of Breast feeding in both NTC and non NTC groups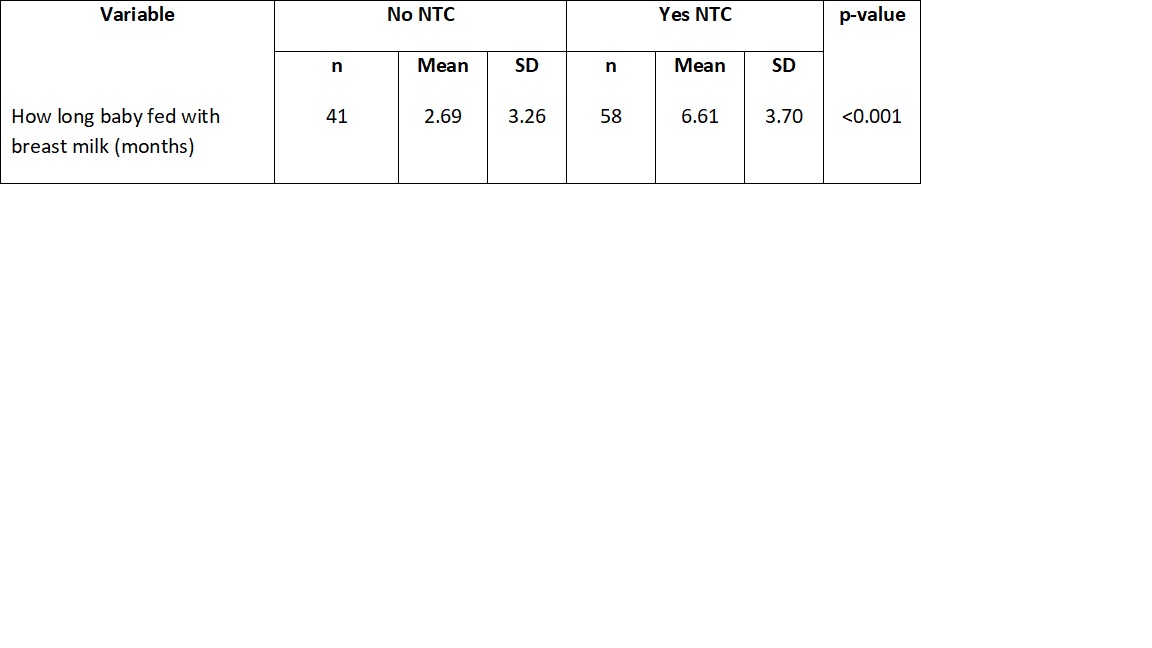
Objective: To compare duration of breastfeeding in infants that attended the NTC program to infants that did not attend the program.
Design/Methods: For this study only infants who were receiving maternal milk at NICU discharge were included in both groups. Descriptive data were reported for both groups and a group t-test were performed to compare duration of breastfeeding between NTC and non-NTC cohorts with a chi-square test. Mean and standard deviation (SD) were calculated. An a-priori p-value of (p < 0.05) to denote significance was used for both analyses.
Results: NTC (n = 58) compared to non-NTC participants (n=41) were more preterm at birth but similar in other measures such as multiples, race, ethnicity, and maternal education. NTC participants were statistically more likely to breastfeed longer than non-NTC participants (n=41) (p < 0.001). NTC participants breast-fed on average 6.61 months (SD= 3.70), while their non-NTC counterpart averaged 2.69 months (SD = 3.26) (p-value < 0.001). Participants in NTC were 3.3 times (95% CI 1.6, 6.7) more likely to breastfeed for at least 6 months compared to those who did not attend NTC (58 vs. 17.5%, respectively).
Satisfaction with the NTC program was very high among participants. The majority of NTC participants described the program as useful when transitioning home (96.5%) and as helpful in sustaining breastfeeding or pumping especially when they wanted to stop or give up (87.93%). In addition, 99.1% described it as useful to have a neonatologist present at the NTC visits. Conclusion(s): Programmatic post discharge help was positively received and related to significantly increased breastfeeding post-NICU discharge.
Breast feeding Duration in both NTC and Non NTC groups
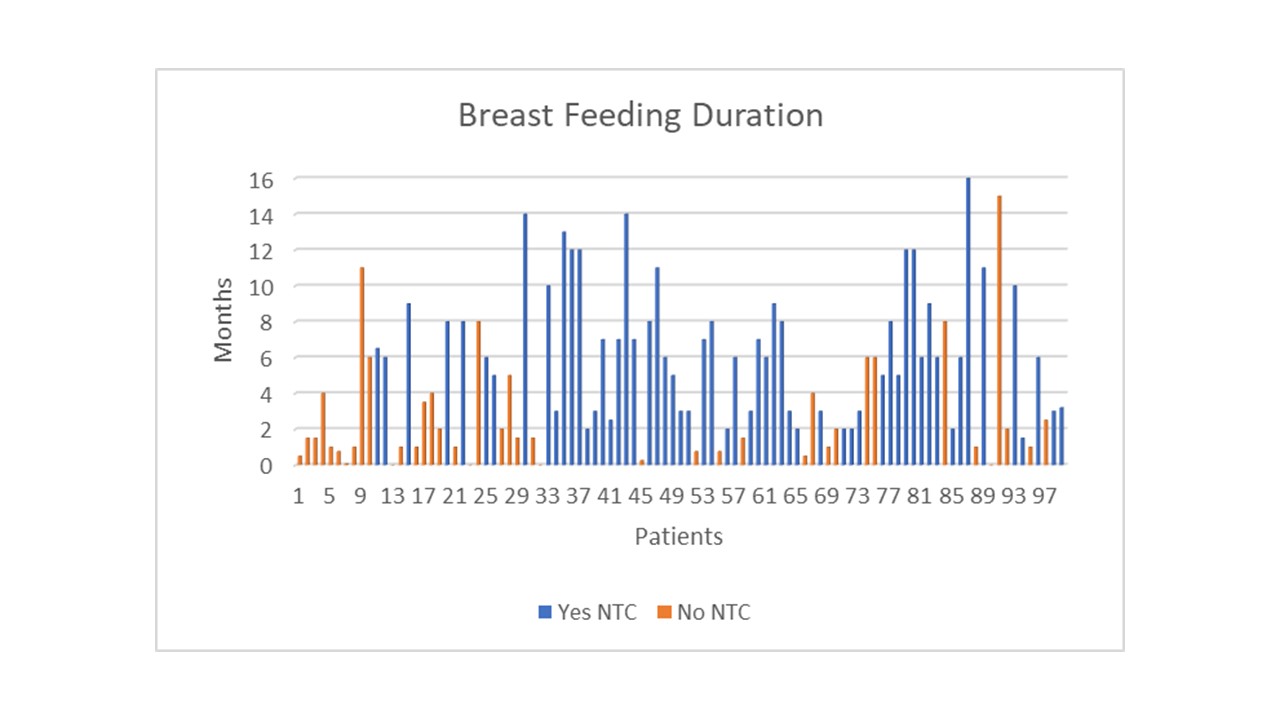
Difference in duration of Breast feeding in both NTC and non NTC groups