Pediatric Neurology
Category: Abstract Submission
Neurology 1: Clinical Pediatric & Neonatal Neurology
537 - Effects of antiepileptic medications with carbonic anhydrase activity on the ketogenic diet.
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 537
Publication Number: 537.139
Publication Number: 537.139
Ayman Abdelmoity, Children's Mercy Hospitals and Clinics, Overland Park, KS, United States; Janelle Noel-MacDonnell, Children’s Mercy Hospital, Kansas City, MO, United States; Jean-Baptiste Le Pichon, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Ahmed Abdelmoity, Children's Mercy Hospitals and Clinics, Overland Park, KS, United States

Jean-Baptiste Le Pichon, MD, PhD
Professor of Pediatrics
Children's Mercy Hospitals and Clinics
Kansas City, Missouri, United States
Presenting Author(s)
Background: The ketogenic diet (KGD) is a well-established treatment for epilepsy. While taking a KGD, patients enter ketosis and frequently develop metabolic acidosis. Zonisamide (ZNS) and topiramate (TPM) are two broad spectrum anti-seizure medications that have proven effective in the management of epilepsy. Both medications have carbonic anhydrase activity and can cause metabolic acidosis. The safety profile of combining ZNS and/or TPM with the KGD remains unclear.
Objective: This study was designed to ascertain the effects of ZNS and/or TPM on patients taking a KGD. Our goal was to determine if either medication affect ketosis, metabolic acidosis, or bone density. Beta-hydroxybutyrate (BHB) and bicarbonate (HCO3) serum levels were used as a proxy for ketosis and metabolic acidosis respectively. Bone density was assessed by DEXA-scans.
Design/Methods: This is a cohort study of 135 patients taking a KGD. Of those 78 were treated with a carbonic anhydrase (TPM and/or ZNS) and made up our KGD+ group. Basic demographics were collected, including age at enrolment, age at seizure onset, age at diet onset, antiepileptic medications used over time, serum BHB levels, HCO3 levels, and DEXA scans. All study individuals were summarized descriptively. Overall serum HCO3 and serum BHB levels were aggregated for each study arm and time taking KGD. Osteopenia prevalence was compared between groups (KGD only vs. KGD+).
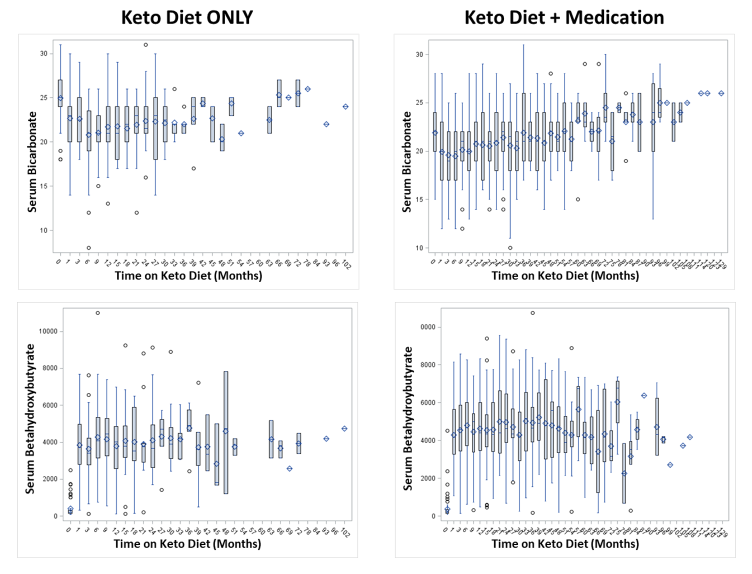
Results: Average age at seizure onset was 0.42 years (IRQ 0.25-1.1) for the patients taking ZNS and/or TPM versus 0.67 years (IRQ 0.25-3.0) for those taking KGD only. Age at KGD onset was 2.6 years (IRQ 1.10-5.67) for KGD+ and 4.04 years (IRQ 1.67-6.58) for those taking a KGD only. The mean bicarbonate and BHB levels across all visits were 20.89 mEq/L and 4225 mMol/L respectively in the KGD+ group versus 22.44 mEq/L and 3440 mMol/L in the group taking a KGD only (Figure1). Variations between tested serum levels across time on KGD were also compared (Figure 2). When we assessed for osteopenia by comparing DEXA-scans, the prevalence was 66.7% in KGD+, only slightly higher than those taking a KGD only, but not statistically different (p=0.424).Conclusion(s): While there was a statistical difference in BHB and bicarbonate serum levels between the two groups, these differences are not clinically significant. When we assessed the DEXA-scans we did not find significant differences between the two groups. We conclude that it is safe to use TPM and/or ZNS in children taking a KGD. This result has important implications for children starting the KGD and considering treatment with either carbonic anhydrase medication.
Figure 1. Bicarbonate and BHB levels across all visits and all patients.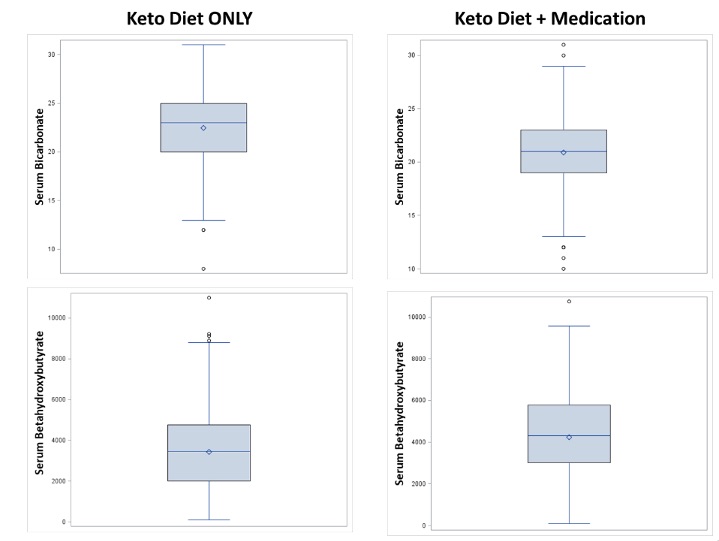
Figure 2. Bicarbonate and BHB levels over time.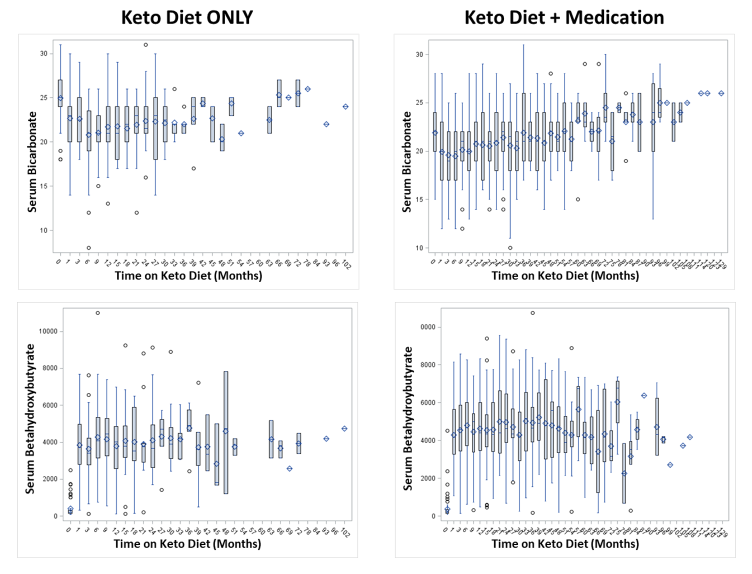
Objective: This study was designed to ascertain the effects of ZNS and/or TPM on patients taking a KGD. Our goal was to determine if either medication affect ketosis, metabolic acidosis, or bone density. Beta-hydroxybutyrate (BHB) and bicarbonate (HCO3) serum levels were used as a proxy for ketosis and metabolic acidosis respectively. Bone density was assessed by DEXA-scans.
Design/Methods: This is a cohort study of 135 patients taking a KGD. Of those 78 were treated with a carbonic anhydrase (TPM and/or ZNS) and made up our KGD+ group. Basic demographics were collected, including age at enrolment, age at seizure onset, age at diet onset, antiepileptic medications used over time, serum BHB levels, HCO3 levels, and DEXA scans. All study individuals were summarized descriptively. Overall serum HCO3 and serum BHB levels were aggregated for each study arm and time taking KGD. Osteopenia prevalence was compared between groups (KGD only vs. KGD+).
Results: Average age at seizure onset was 0.42 years (IRQ 0.25-1.1) for the patients taking ZNS and/or TPM versus 0.67 years (IRQ 0.25-3.0) for those taking KGD only. Age at KGD onset was 2.6 years (IRQ 1.10-5.67) for KGD+ and 4.04 years (IRQ 1.67-6.58) for those taking a KGD only. The mean bicarbonate and BHB levels across all visits were 20.89 mEq/L and 4225 mMol/L respectively in the KGD+ group versus 22.44 mEq/L and 3440 mMol/L in the group taking a KGD only (Figure1). Variations between tested serum levels across time on KGD were also compared (Figure 2). When we assessed for osteopenia by comparing DEXA-scans, the prevalence was 66.7% in KGD+, only slightly higher than those taking a KGD only, but not statistically different (p=0.424).Conclusion(s): While there was a statistical difference in BHB and bicarbonate serum levels between the two groups, these differences are not clinically significant. When we assessed the DEXA-scans we did not find significant differences between the two groups. We conclude that it is safe to use TPM and/or ZNS in children taking a KGD. This result has important implications for children starting the KGD and considering treatment with either carbonic anhydrase medication.
Figure 1. Bicarbonate and BHB levels across all visits and all patients.
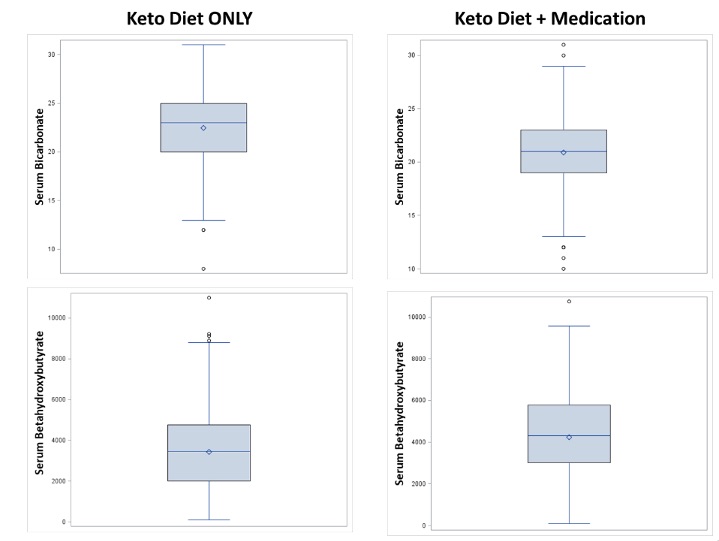
Figure 2. Bicarbonate and BHB levels over time.