Endocrinology: Type 2 Diabetes (T2 DM)
Category: Abstract Submission
Endocrinology I
524 - Implementation of 2020 ADA Recommendations for the Initial Management of Overweight and Obese Pediatric Patients with New Onset Diabetes
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 524
Publication Number: 524.107
Publication Number: 524.107
Atima Huria, Brody School of Medicine at East Carolina University, Greenville, NC, United States; Jennifer Sutter, Brody School of Medicine at East Carolina University, Greenville, NC, United States; Kaitlin Hamilton, ECU Physicians, Greenville, NC, United States; Mindy Saenz, BSOM at ECU, Pediatrics, Greenville, NC, United States

Atima Huria, MS-4
Medical Student
Brody School of Medicine at East Carolina University
Greenville, North Carolina, United States
Presenting Author(s)
Background: The 2020 American Diabetes Association (ADA) Standard of Medical Care in Diabetes for Children and Adolescents recommends that initial therapy for overweight/obese patients with new onset diabetes appropriately address metabolic derangements. The guidelines also suggest that, for a subset of patients, less intensive therapy initiated in the outpatient setting may achieve target HgbA1c. Historically, our center hospitalized most patients with new onset diabetes and initiated full basal/bolus (intensive) insulin regardless of initial labs and likelihood of Type 2 Diabetes (T2D).
Objective: We implemented a standardized protocol for the initial management of overweight/obese patients 10 to 17 years of age with new onset diabetes to align our practice with the 2020 ADA recommendations, with the goal of decreasing hospital admission rates and use of intensive insulin.
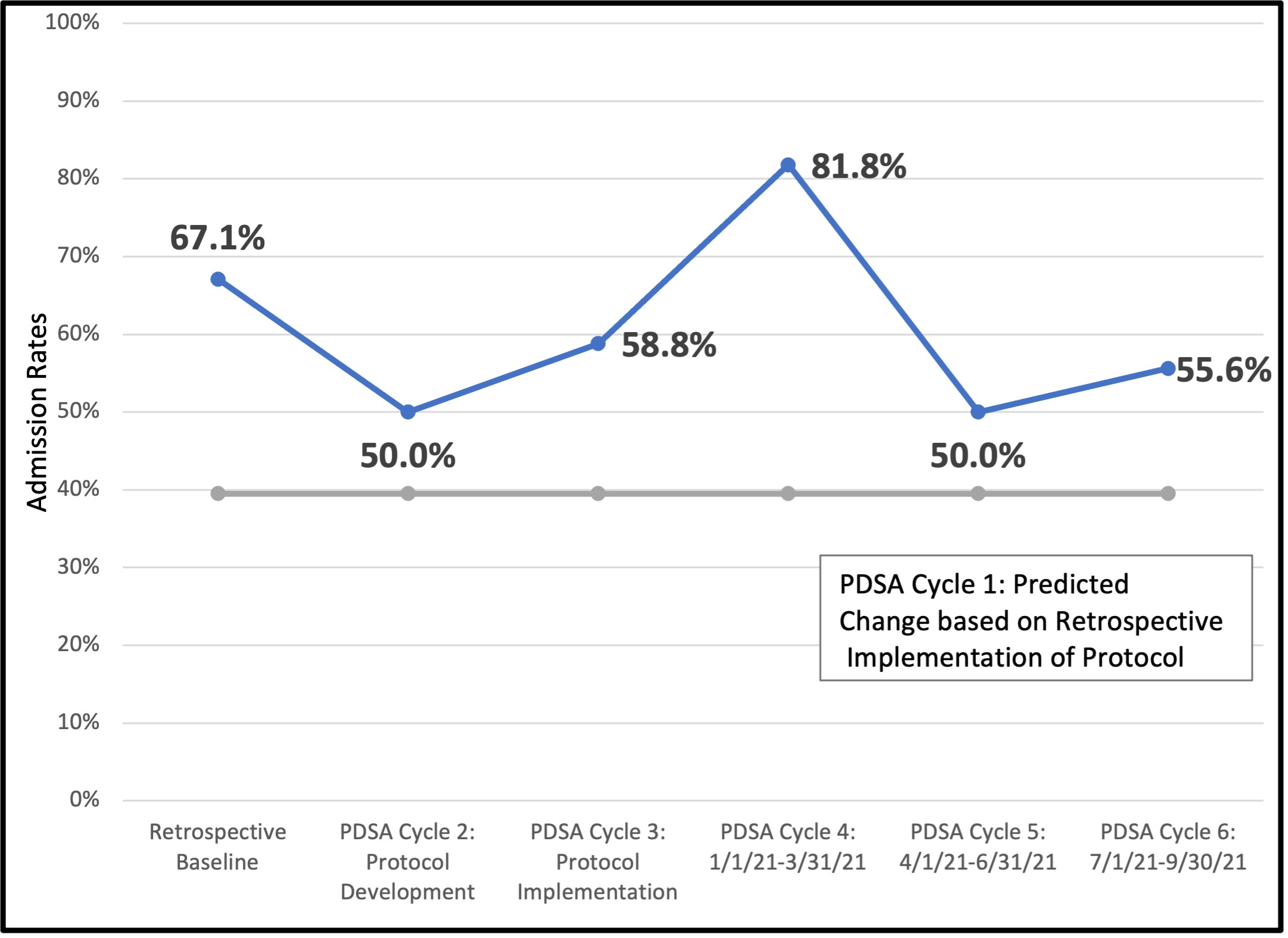
Design/Methods: A treatment protocol was developed based on initial labs (Fig 1). The protocol was retrospectively applied to patients with T2D seen in clinic to determine the expected change in admission rates and use of intensive insulin. Beginning June 2020, Plan-Do-Study-Act cycles were utilized to implement the protocol prospectively, while monitoring admission rates at diagnosis and the percentage of patients initially managed by one of five treatment regimens defined by escalation of insulin therapy.
Results: Our retrospective review revealed a 67% admission rate at T2D diagnosis with 66% of patients receiving intensive insulin. In this cohort, the new protocol would have implied a reduction in admission rates to 40% and intensive insulin use to 20%. Following implementation of the protocol with adherence rates improving from 68% to 94%, the median quarterly admission rate between June 2020 and September 2021 was 56%, with 49% of patients receiving intensive insulin therapy (Fig 2 and 3). Preliminary data review suggests that more patients treated with rapid and long-acting insulin reach target HgbA1c within 6 months of diagnosis (85%) when compared to diet and lifestyle management, metformin, or long-acting insulin alone (68%).Conclusion(s): While not meeting predicted targets despite improved adherence to our protocol, we decreased hospital admission rates at diagnosis by 16% and intensive insulin use by 26%. A higher rate of diabetic ketoacidosis, ketosis, and severe hyperglycemia at diagnosis during the project period likely impacted the results. Additional follow-up is needed to determine the impact of this protocol on short- and long-term diabetes control.
Atima Huria CVHuria A CV 1-22.pdf
Figure 2: Admission Rates at the Time of Diagnosis for Overweight and Obese Patients (10 to 17 Years) Ultimately Diagnosed with Type 2 Diabetes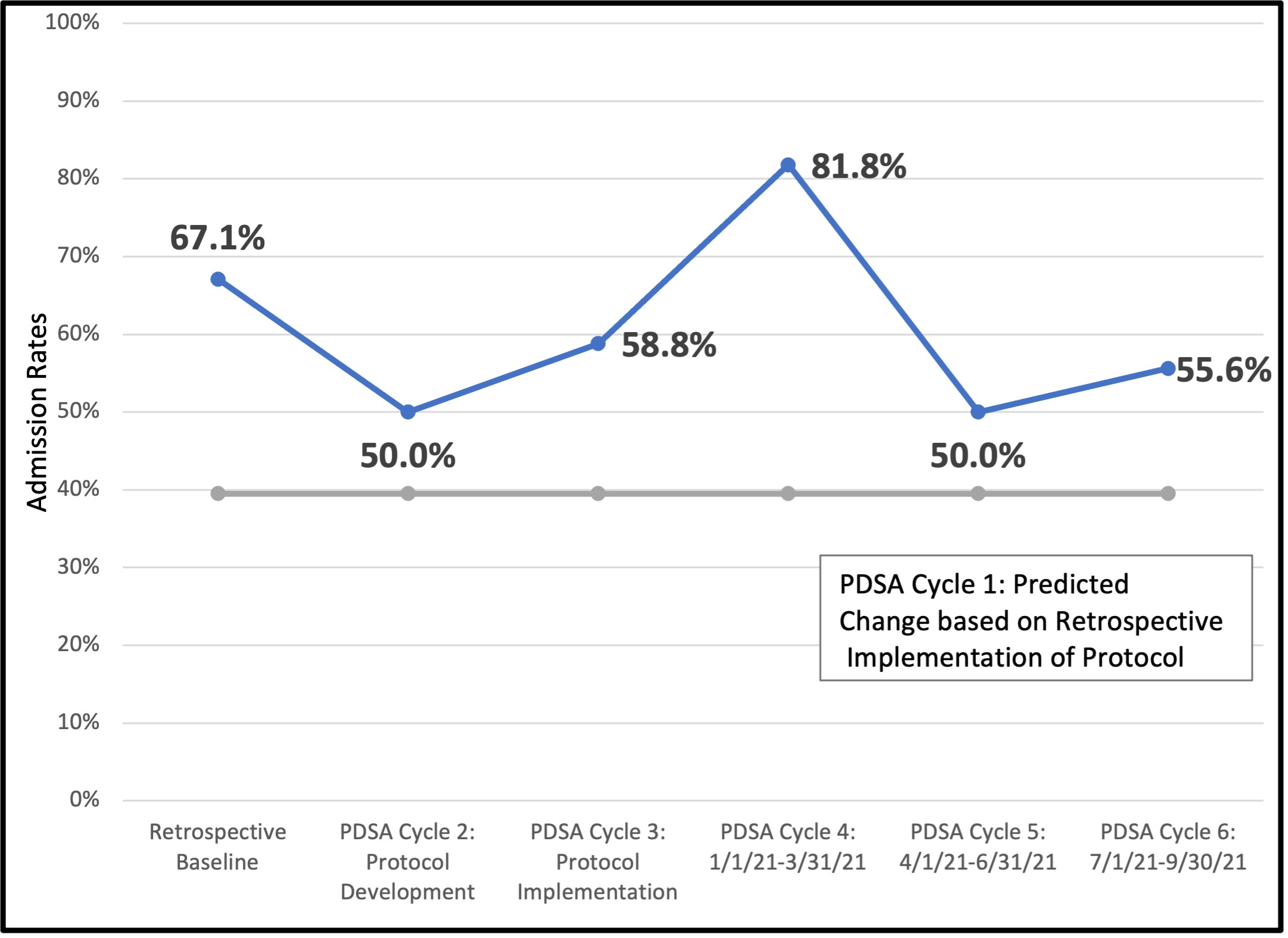
Objective: We implemented a standardized protocol for the initial management of overweight/obese patients 10 to 17 years of age with new onset diabetes to align our practice with the 2020 ADA recommendations, with the goal of decreasing hospital admission rates and use of intensive insulin.
Design/Methods: A treatment protocol was developed based on initial labs (Fig 1). The protocol was retrospectively applied to patients with T2D seen in clinic to determine the expected change in admission rates and use of intensive insulin. Beginning June 2020, Plan-Do-Study-Act cycles were utilized to implement the protocol prospectively, while monitoring admission rates at diagnosis and the percentage of patients initially managed by one of five treatment regimens defined by escalation of insulin therapy.
Results: Our retrospective review revealed a 67% admission rate at T2D diagnosis with 66% of patients receiving intensive insulin. In this cohort, the new protocol would have implied a reduction in admission rates to 40% and intensive insulin use to 20%. Following implementation of the protocol with adherence rates improving from 68% to 94%, the median quarterly admission rate between June 2020 and September 2021 was 56%, with 49% of patients receiving intensive insulin therapy (Fig 2 and 3). Preliminary data review suggests that more patients treated with rapid and long-acting insulin reach target HgbA1c within 6 months of diagnosis (85%) when compared to diet and lifestyle management, metformin, or long-acting insulin alone (68%).Conclusion(s): While not meeting predicted targets despite improved adherence to our protocol, we decreased hospital admission rates at diagnosis by 16% and intensive insulin use by 26%. A higher rate of diabetic ketoacidosis, ketosis, and severe hyperglycemia at diagnosis during the project period likely impacted the results. Additional follow-up is needed to determine the impact of this protocol on short- and long-term diabetes control.
Atima Huria CVHuria A CV 1-22.pdf
Figure 2: Admission Rates at the Time of Diagnosis for Overweight and Obese Patients (10 to 17 Years) Ultimately Diagnosed with Type 2 Diabetes