Medical Education: Resident
Category: Abstract Submission
Medical Education 2 - Medical Education: Resident I - Hot Topics
568 - Improving Resident and Faculty Wellness by Development, Implementation and Evaluation of a Physician Wellness Curriculum
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 568
Publication Number: 568.116
Publication Number: 568.116
Suleiman Essoh, RUMC, Staten Island, NY, United States; Santosh Parab, Richmond University Medical Center, Staten Island, NY, United States; Jiliu Xu, Richmond University Medical Center, Staten Island, NY, United States; Ishita Kharode, Richmond University Medical Center, Staten Island, NY, United States; Ana V. Mendez, Richmond University Medical Center, Bronx, NY, United States; Melissa Grageda, Richmond University Medical Center, Staten Island, NY, United States

Suleiman Essoh, MD
Resident Physician
RUMC
Staten Island, New York, United States
Presenting Author(s)
Background: The overall physician burnout rate in the United States in 2020 was 42%, with 79% of physicians stating that their burnout began before the onset of the COVID-19 pandemic in March 2020. In residents, burnout rates have ranged from 41 to 90%. To address these concerning facts, our residency program sought to strengthen our physician wellness initiative through development, implementation and evaluation of a formal wellness curriculum.
Objective: The primary objective was to improve pediatric resident and faculty physician wellness at our community based residency program by achieving a wellness score above 80% over 3 years. The secondary goal was to describe the program’s experience while developing and refining the physician wellness curriculum.
Design/Methods: The project timeline was set at 3 years, with 2019 as the baseline year. The curriculum was designed by the clinical competency committee of our residency program at a suburban community-based hospital. Core competencies that were addressed included: professionalism, interpersonal and communication skills, system-based practice, practice-based learning and improvement. Curriculum development, implementation and evaluation were performed in concert with regular PDSA meetings comprised by resident and faculty focus groups to identify gaps or opportunities for improvement, and develop action plans. The outcome measure was the annual average score from the wellness survey sent by the Accreditation Council for Graduate Medical Education (ACGME) to 18 resident and 15 faculty physicians.
Results: Survey response rates were 100% for residents, and 79-92% for faculty physicians. Monthly wellness sessions during the first year focused on resident burnout recognition and prevention. Activities included workshops for relaxation, cardiovascular exercise, and team-building. Additional topics identified through PDSA meetings included: optimizing shift work hours, time management, financial wellness, nutrition, physical fitness, sleep hygiene, dealing with challenging situations at work, and how to cope when litigation arises. During the COVID-19 pandemic (year 1), frequency of wellness sessions were increased from monthly to weekly. During year 2, faculty participation was mandated and significantly increased. The average wellness score increased over 2 years, from 34 to 65% for residents, and 62 to 76% for faculty.Conclusion(s): Implementation and ongoing development of a regular wellness curriculum was associated with improved average wellness scores of resident and faculty physicians in a suburban community-based pediatric residency program.
Image 1. Run Chart of Resident and Faculty Wellness Scores.png) Run chart showing outcomes of interventions expressed as average wellness scores, which increased for both residents and faculty physicians over 2 years.
Run chart showing outcomes of interventions expressed as average wellness scores, which increased for both residents and faculty physicians over 2 years.
Table 1. ACGME Wellness Survey Scores of Pediatric Residents and Faculty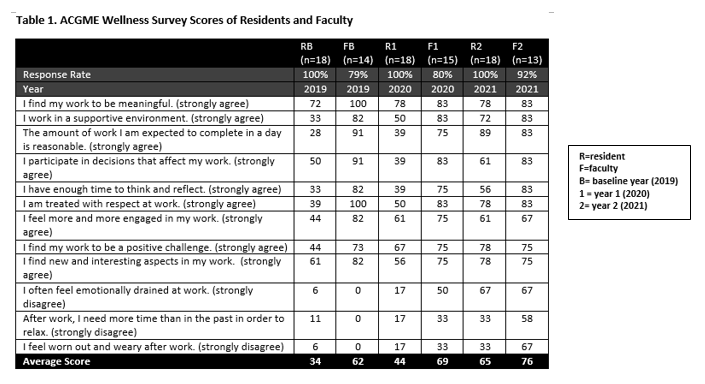 Response rates and wellness survey scores of resident and faculty physicians.
Response rates and wellness survey scores of resident and faculty physicians.
Objective: The primary objective was to improve pediatric resident and faculty physician wellness at our community based residency program by achieving a wellness score above 80% over 3 years. The secondary goal was to describe the program’s experience while developing and refining the physician wellness curriculum.
Design/Methods: The project timeline was set at 3 years, with 2019 as the baseline year. The curriculum was designed by the clinical competency committee of our residency program at a suburban community-based hospital. Core competencies that were addressed included: professionalism, interpersonal and communication skills, system-based practice, practice-based learning and improvement. Curriculum development, implementation and evaluation were performed in concert with regular PDSA meetings comprised by resident and faculty focus groups to identify gaps or opportunities for improvement, and develop action plans. The outcome measure was the annual average score from the wellness survey sent by the Accreditation Council for Graduate Medical Education (ACGME) to 18 resident and 15 faculty physicians.
Results: Survey response rates were 100% for residents, and 79-92% for faculty physicians. Monthly wellness sessions during the first year focused on resident burnout recognition and prevention. Activities included workshops for relaxation, cardiovascular exercise, and team-building. Additional topics identified through PDSA meetings included: optimizing shift work hours, time management, financial wellness, nutrition, physical fitness, sleep hygiene, dealing with challenging situations at work, and how to cope when litigation arises. During the COVID-19 pandemic (year 1), frequency of wellness sessions were increased from monthly to weekly. During year 2, faculty participation was mandated and significantly increased. The average wellness score increased over 2 years, from 34 to 65% for residents, and 62 to 76% for faculty.Conclusion(s): Implementation and ongoing development of a regular wellness curriculum was associated with improved average wellness scores of resident and faculty physicians in a suburban community-based pediatric residency program.
Image 1. Run Chart of Resident and Faculty Wellness Scores
.png) Run chart showing outcomes of interventions expressed as average wellness scores, which increased for both residents and faculty physicians over 2 years.
Run chart showing outcomes of interventions expressed as average wellness scores, which increased for both residents and faculty physicians over 2 years.Table 1. ACGME Wellness Survey Scores of Pediatric Residents and Faculty
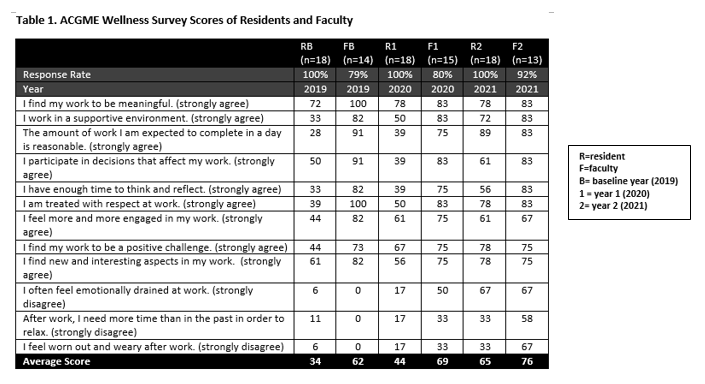 Response rates and wellness survey scores of resident and faculty physicians.
Response rates and wellness survey scores of resident and faculty physicians.