Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up I
449 - Influence of Multi-Disciplinary Follow-up on Outcomes of Patients with Bronchopulmonary Dysplasia
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 449
Publication Number: 449.121
Publication Number: 449.121
Christine Sugimoto, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Jennifer M. Brady, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Erik Hysinger, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Melissa House, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States

Christine Sugimoto, MD
Staff Physician
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Former premature infants with bronchopulmonary dysplasia (BPD) discharged on home supplemental oxygen therapy have complex care needs and are at increased risk for respiratory compromise, hospital readmissions, growth failure, and neurodevelopmental impairment after neonatal intensive care unit (NICU) discharge. However, limited evidence exists to direct the outpatient care of infants with BPD after discharge from the NICU.
Objective: To compare the respiratory and growth outcomes and resource utilization among patients with BPD discharged after initial birth hospitalization on home supplemental oxygen therapy who were managed in routine neonatal follow-up to patients who were followed in a multi-disciplinary BPD clinic.
Design/Methods: We performed a retrospective study of infants born < 32 weeks who were diagnosed with moderate or severe BPD and discharged with home supplemental oxygen therapy. Infants whose medical and developmental needs were managed in our Neonatal follow-up clinic from 2013-2018 were compared to those who were managed in a multi-disciplinary BPD clinic with collaborative management by Neonatology and Pulmonology from 2018-2020. Outcomes were hospital readmissions, emergency department visits, clinic attendance rates, developmental therapy referrals, respiratory medication prescriptions, and growth trajectory in the 12 months after the first clinic visit. Univariate analyses were used to compare outcomes. A p-value of < 0.05 was considered significant.
Results: The study included 86 infants. Patients enrolled in the multi-disciplinary clinic were born at younger gestation, lower birthweight, and more likely to have pulmonary hypertension (Table 1). There were significantly fewer respiratory-related readmissions over a one-year period when comparing patients with multi-disciplinary follow-up to the neonatology only follow-up group. Emergency department visits and hospital length of stay were similar. Additionally, growth parameters at 12-months corrected gestational age, clinic attendance, duration of home oxygen therapy, and number of respiratory medications were not significantly different between groups (Table 2).Conclusion(s): Patients followed in the multi-disciplinary clinic had fewer respiratory hospitalizations despite increased comorbidities. Our results suggest the potential benefits of a multi-disciplinary follow-up clinic in reducing health care utilization among a high-risk patient population with BPD. Further studies with a larger sample may better support the value of interdisciplinary outpatient follow-up for infants with moderate to severe BPD.
Table 1. Characteristics of the study population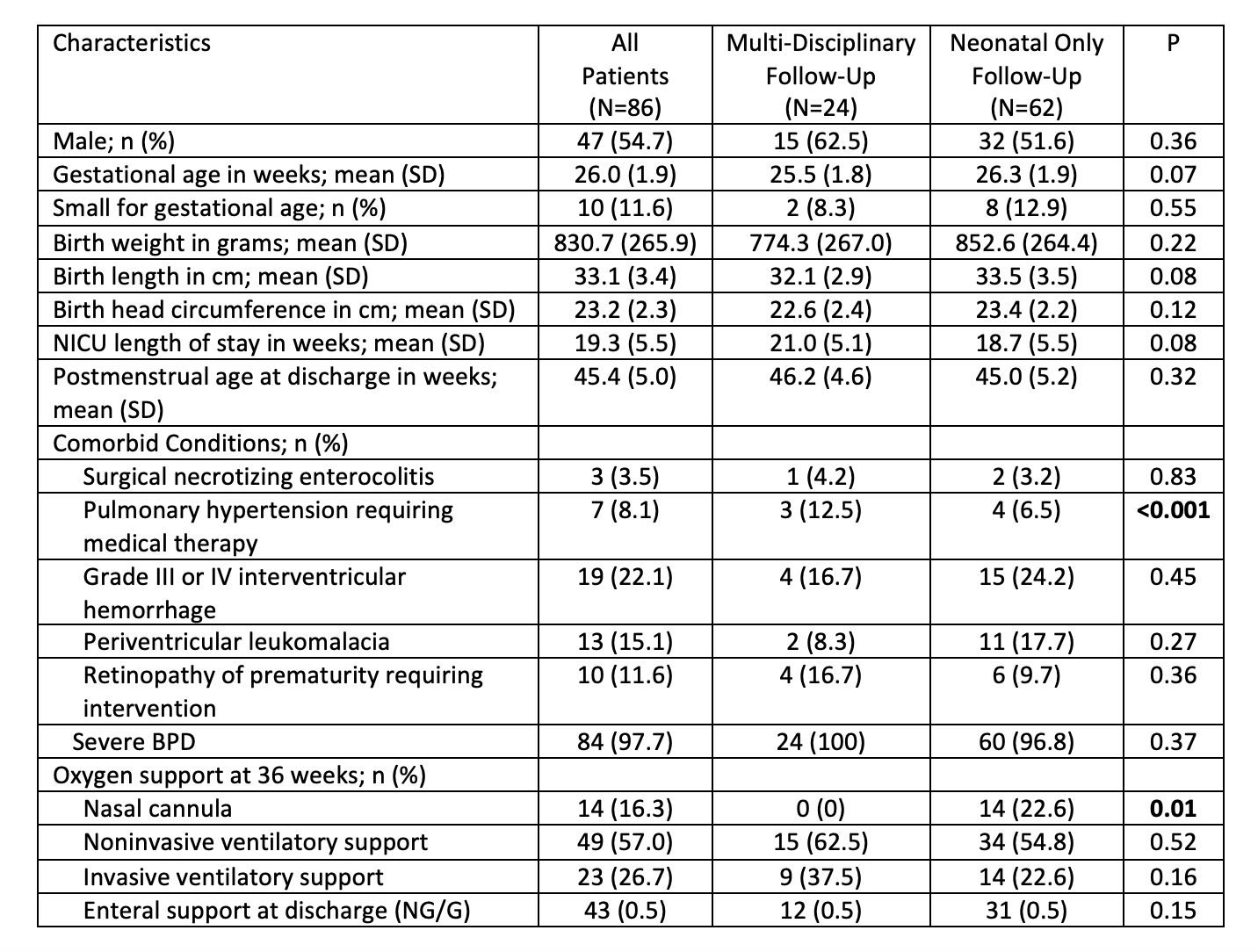
Table 2. Outcomes of patients followed in multi-disciplinary follow-up vs neonatal only follow-up.png)
Objective: To compare the respiratory and growth outcomes and resource utilization among patients with BPD discharged after initial birth hospitalization on home supplemental oxygen therapy who were managed in routine neonatal follow-up to patients who were followed in a multi-disciplinary BPD clinic.
Design/Methods: We performed a retrospective study of infants born < 32 weeks who were diagnosed with moderate or severe BPD and discharged with home supplemental oxygen therapy. Infants whose medical and developmental needs were managed in our Neonatal follow-up clinic from 2013-2018 were compared to those who were managed in a multi-disciplinary BPD clinic with collaborative management by Neonatology and Pulmonology from 2018-2020. Outcomes were hospital readmissions, emergency department visits, clinic attendance rates, developmental therapy referrals, respiratory medication prescriptions, and growth trajectory in the 12 months after the first clinic visit. Univariate analyses were used to compare outcomes. A p-value of < 0.05 was considered significant.
Results: The study included 86 infants. Patients enrolled in the multi-disciplinary clinic were born at younger gestation, lower birthweight, and more likely to have pulmonary hypertension (Table 1). There were significantly fewer respiratory-related readmissions over a one-year period when comparing patients with multi-disciplinary follow-up to the neonatology only follow-up group. Emergency department visits and hospital length of stay were similar. Additionally, growth parameters at 12-months corrected gestational age, clinic attendance, duration of home oxygen therapy, and number of respiratory medications were not significantly different between groups (Table 2).Conclusion(s): Patients followed in the multi-disciplinary clinic had fewer respiratory hospitalizations despite increased comorbidities. Our results suggest the potential benefits of a multi-disciplinary follow-up clinic in reducing health care utilization among a high-risk patient population with BPD. Further studies with a larger sample may better support the value of interdisciplinary outpatient follow-up for infants with moderate to severe BPD.
Table 1. Characteristics of the study population
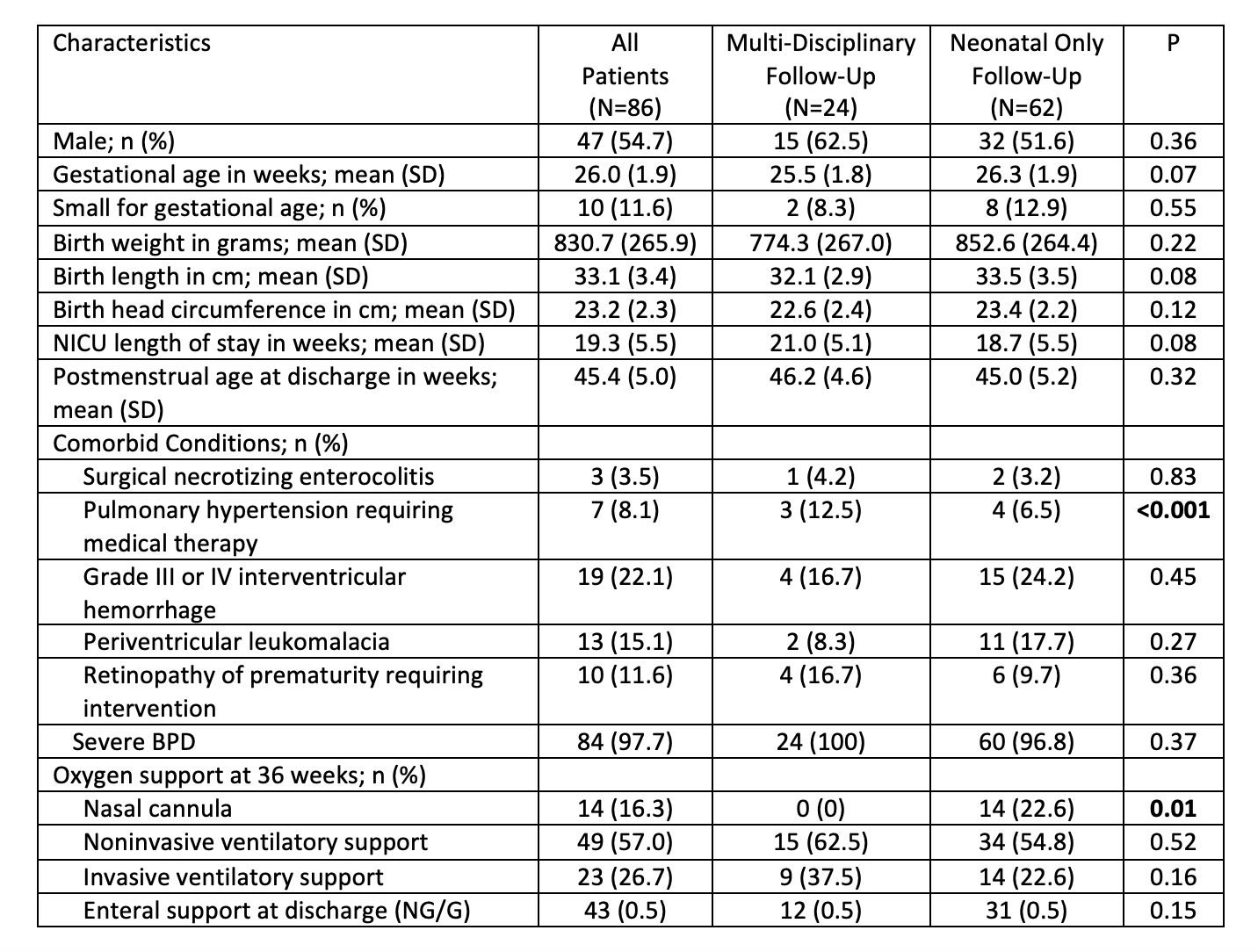
Table 2. Outcomes of patients followed in multi-disciplinary follow-up vs neonatal only follow-up
.png)
