Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine III
67 - Lumbar Puncture Success Rate in the Pediatric Emergency Department
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 67
Publication Number: 67.105
Publication Number: 67.105
Mara Alexeev, Boston Children's Hospital, Brookline, MA, United States; Assaf Landschaft, Boston Children's Hospital, Bergisch Gladbach, Nordrhein-Westfalen, Germany; Al Ozonoff, Harvard Medical School, Boston, MA, United States; Lise E. Nigrovic, Boston Children's Hospital, Boston, MA, United States; Marvin B. Harper, Harvard Medical School, Boston, MA, United States; Jennifer Kupiec, Boston Children's Hospital, Boston, MA, United States; Amir Kimia, Boston Children's Hospital, Boston, MA, United States

Mara Alexeev, MD, MPH
Clinical Informatics Fellow
Boston Children's Hospital
Brookline, Massachusetts, United States
Presenting Author(s)
Background: The frequency of lumbar punctures (LPs) procedures has declined over the past two decades with uncertain impacts on lumbar puncture competence. Unsuccessful LPs can be challenging to identify using available administrative or self-reported data.
Objective: Our goal was to identify the proportion of attempted LPs that were ultimately unsuccessful.
Design/Methods: We performed a retrospective cross-sectional study of all ED encounters for children 21 years or younger who presented between 2017-2019 to a tertiary care pediatric center, focusing on Lumbar Puncture (LP). We defined an unsuccessful LP as no CSF obtained, CSF culture only, or CSF RBC ≥ 10,000 cells/mm3.
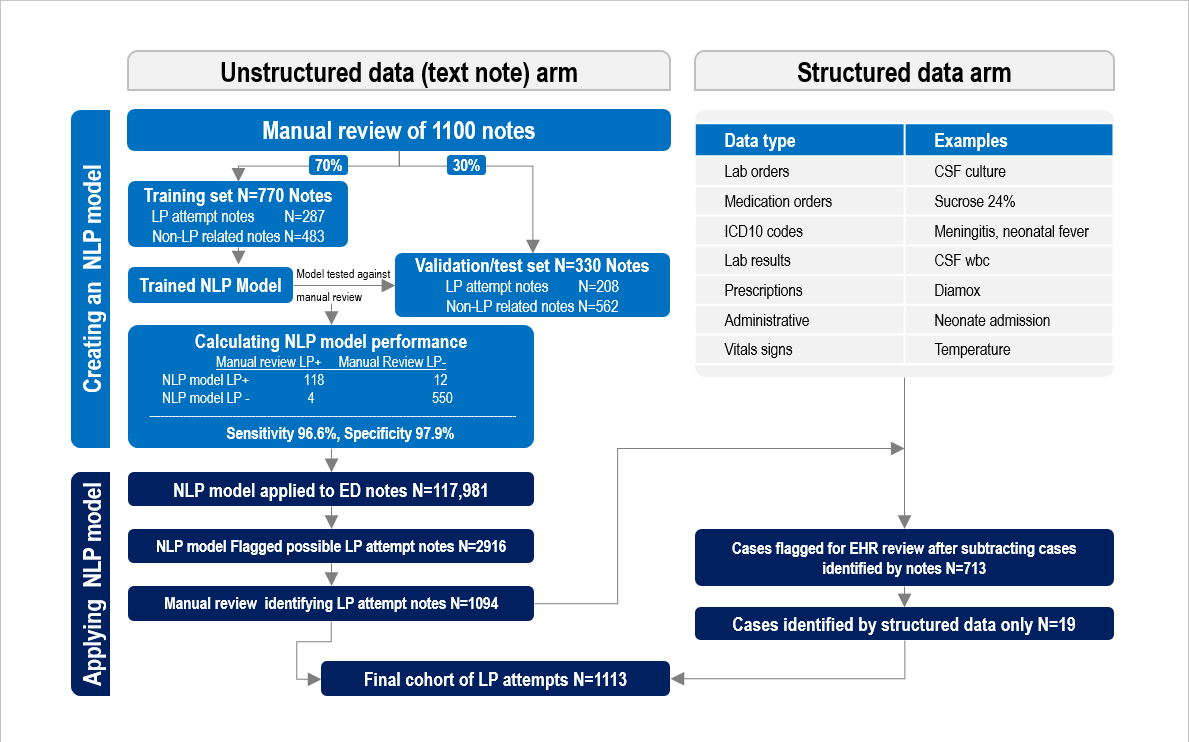
We developed a Natural Language Processing (NLP) model to identify these procedures from unstructured data (clinical note text), using a sample of manually reviewed notes from one year of data. We randomly selected 70% of the notes as a training set, and held aside the remaining 30% of notes as a validation/testing set. We compared NLP model classification to the manual chart review and calculated the sensitivity and specificity of the classifier for identifying notes describing an LP attempt. We then applied the NLP model to all ED notes during the study period and reviewed the output manually.
We also used unstructured data (e.g. physician orders, laboratory results, billing codes) to flag cases for manual review.
Results: In the validation cohort, the NLP model identified 118 of the 122 LPs identified by medical records review: sensitivity 96.6% (95% CI 93.4-99.9%) and specificity 97.9% (95% CI 96.4-99.3%). The NLP model was then applied to 117,981 ED encounters during the study period and the NLP classifier output provided 2916 notes for manual review, of which we identified 1,094 notes describing an LP attempted. Screening an additional 713 cases flagged by structured data, identified an additional 19 cases, for an overall 1113 ED encounters with LP attempts (0.63% of encounters) (see figure 1.) Unsuccessful LPs occurred in 226/1113 (20.3%). Of these, fluid was not obtained in 104 (9.3%), LP sent for culture only in 53 (4.8%), and LP with ≥ 10,000 CSF RBC cells/mm3 in 69 (6.2%). Conclusion(s): Failure rates are much higher than previously published data. NLP provides a novel method to improve the identification of attempted LPs, which may not be captured by structured data.
Flowchart of lumbar puncture cases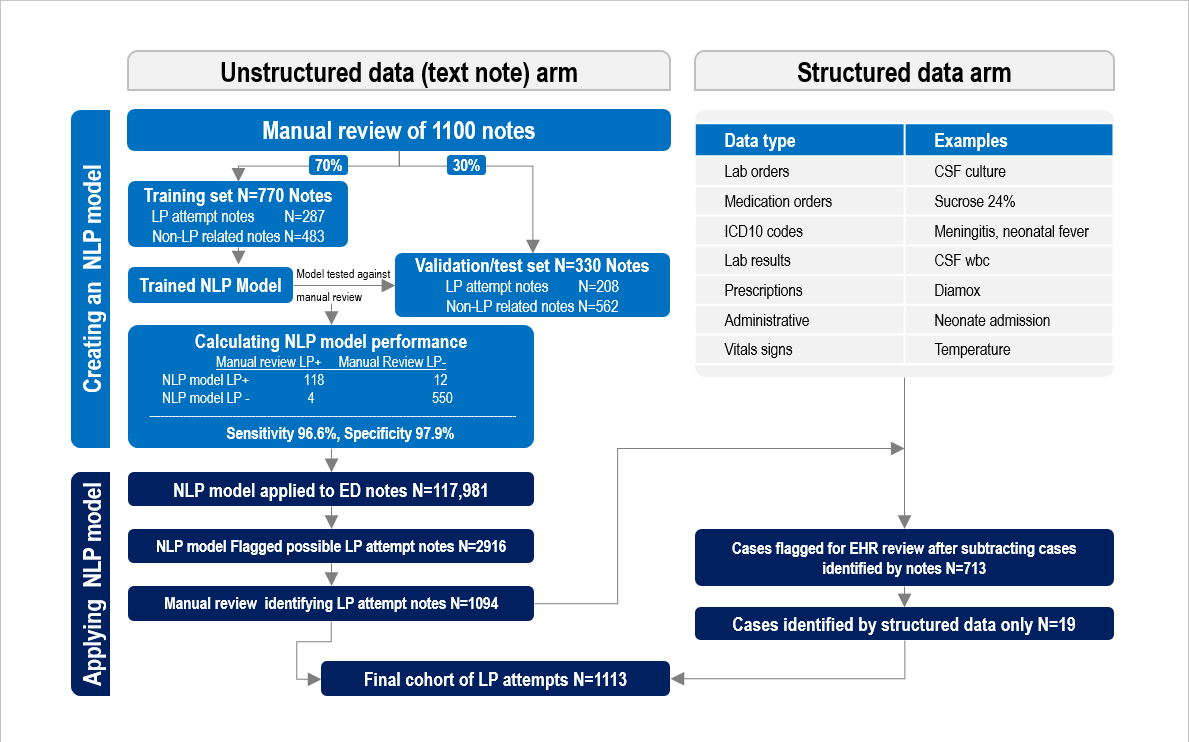
Objective: Our goal was to identify the proportion of attempted LPs that were ultimately unsuccessful.
Design/Methods: We performed a retrospective cross-sectional study of all ED encounters for children 21 years or younger who presented between 2017-2019 to a tertiary care pediatric center, focusing on Lumbar Puncture (LP). We defined an unsuccessful LP as no CSF obtained, CSF culture only, or CSF RBC ≥ 10,000 cells/mm3.
We developed a Natural Language Processing (NLP) model to identify these procedures from unstructured data (clinical note text), using a sample of manually reviewed notes from one year of data. We randomly selected 70% of the notes as a training set, and held aside the remaining 30% of notes as a validation/testing set. We compared NLP model classification to the manual chart review and calculated the sensitivity and specificity of the classifier for identifying notes describing an LP attempt. We then applied the NLP model to all ED notes during the study period and reviewed the output manually.
We also used unstructured data (e.g. physician orders, laboratory results, billing codes) to flag cases for manual review.
Results: In the validation cohort, the NLP model identified 118 of the 122 LPs identified by medical records review: sensitivity 96.6% (95% CI 93.4-99.9%) and specificity 97.9% (95% CI 96.4-99.3%). The NLP model was then applied to 117,981 ED encounters during the study period and the NLP classifier output provided 2916 notes for manual review, of which we identified 1,094 notes describing an LP attempted. Screening an additional 713 cases flagged by structured data, identified an additional 19 cases, for an overall 1113 ED encounters with LP attempts (0.63% of encounters) (see figure 1.) Unsuccessful LPs occurred in 226/1113 (20.3%). Of these, fluid was not obtained in 104 (9.3%), LP sent for culture only in 53 (4.8%), and LP with ≥ 10,000 CSF RBC cells/mm3 in 69 (6.2%). Conclusion(s): Failure rates are much higher than previously published data. NLP provides a novel method to improve the identification of attempted LPs, which may not be captured by structured data.
Flowchart of lumbar puncture cases