Neonatal General
Category: Abstract Submission
Neonatology General 3
376 - Machine Learning Algorithm for Prediction of Neonatal Mortality in Zambia
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 376
Publication Number: 376.133
Publication Number: 376.133
Albert Manasyan, University of Alabama School of Medicine, Birmingham, AL, United States; Katayoun Taghavi, UNIVERSITY OF BERN, Bern, Bern, Switzerland; Miquel Duran-Frigola, Ersilia Open Source Initiative, Cambridge, England, United Kingdom; Herbert Kapesa, Center For Infectiouse Disease Research in Zambia, Lusaka, Lusaka, Zambia; Martha A. Mwendafilumba, CIDRZ, Lusaka, Lusaka, Zambia; Nobutu Muttau, Centre for Infectious Disease Research in Zambia (CIDRZ), Lusaka, Lusaka, Zambia; Tamara Mulenga Willows, University of Oxford, Oxford, England, United Kingdom; Vivek V. Shukla, University of Alabama at Birmingham, Birmingham, AL, United States; Misinzo Moono, Centre for Infectious Disease Research in Zambia, Lusaka, Lusaka, Zambia; Waldemar A. Carlo, University of Alabama at Birmingham, Birmingham, AL, United States

Vivek Shukla, MD (he/him/his)
Assistant Professor
University of Alabama at Birmingham
Birmingham, Alabama, United States
Presenting Author(s)
Background: Annual 2.5 million global neonatal deaths contribute to about 45% of under-five mortality. Predicting the risk of neonatal mortality and identifying factors associated with an increase in the risk may help recognize at-risk neonates for targeted interventions.
Objective: To develop predictive models for early (0-6 days) and late (7-27 days) neonatal mortality.
Design/Methods: This analysis was conducted using data from the Preterm Resources, Education, and Effective Management of Infants (PREEMI) study, which collected prospective data on pregnancies and delivery outcomes (n=11,543) up to 42 days post-partum in Lusaka, Zambia. We used advanced and conventional machine learning modelling methods and a stacking ensemble approach the develop the predictive models. We included antenatal and delivery related clinical variables as predictors for early and late neonatal mortality. Variables were grouped into pregnancy outcomes (alive, miscarriage, stillbirth, neonatal death), gestation age (last menstrual period, delivery date, method of determining gestation), confounders (maternal age, years of education, parity, BMI, ANC visits, delivered by, delivery location, mode of delivery, sex, birthweight, multiple birth, and gravida), and neonatal treatment (antibiotics, CPAP, oxygen, dexamethasone, KMC, Chlorhexidine for cord care, bag and mask resuscitation). The top predictors for the models were measured with a permutation-shuffle approach. The data was divided into training (20%) and test (80%) datasets. Machine learning based models were used to predict early and late neonatal mortality.
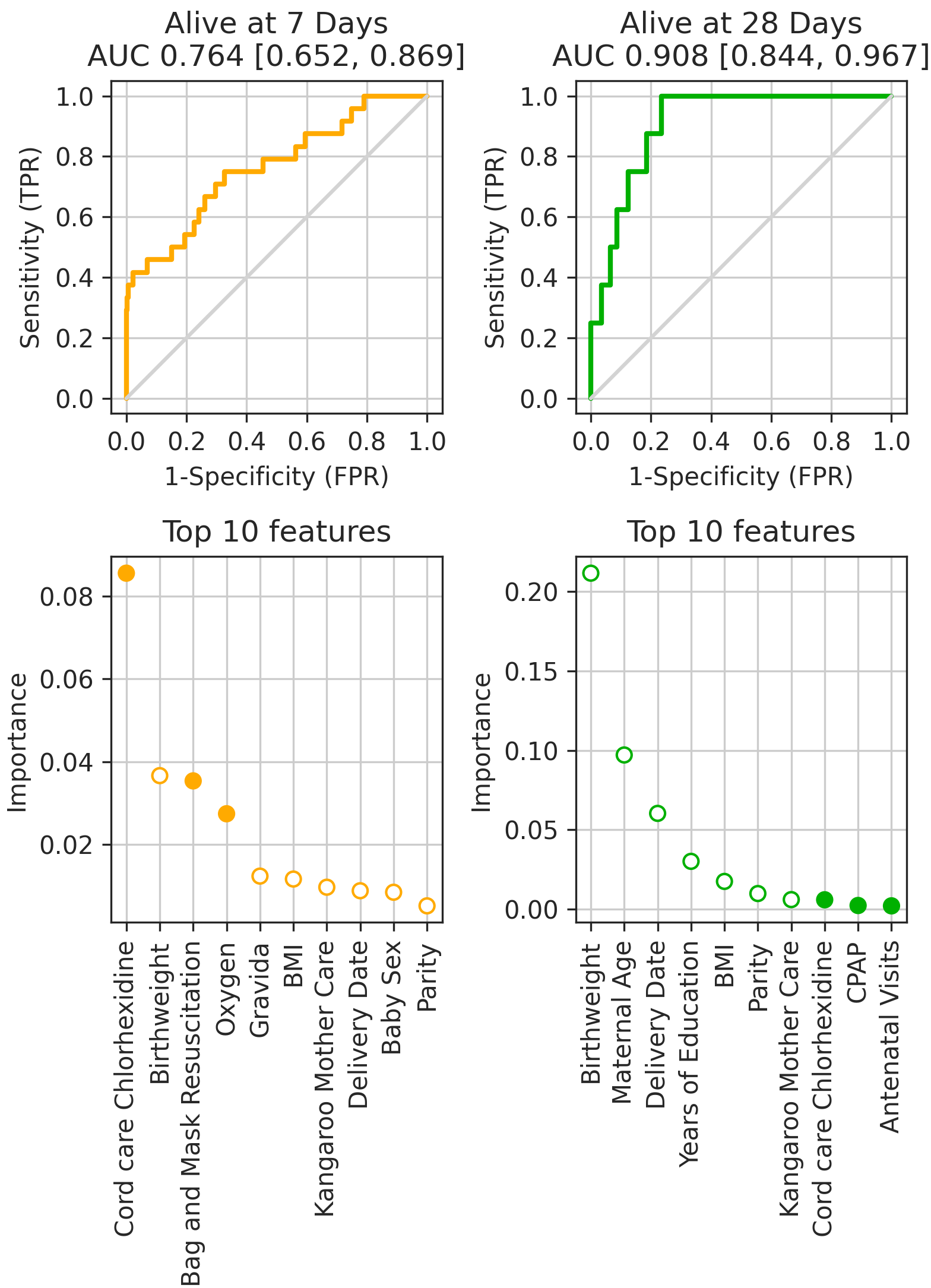
Results: The models had good predictive accuracy for both early and late neonatal mortality with AUC values of 0.76 and 0.90 respectively (Table 1). The first row shows the performance of the classifiers on a hold-out test set corresponding to the latest 20% of collected data, thus simulating a prospective prediction scenario. The second row identifies the most important features for the classifiers. Filled dots indicate modifiable or actionable features. The top three predictors for early neonatal mortality were chlorhexidine for cord care, birthweight, and bag and mask resuscitation. The top three predictors for late neonatal mortality were birthweight, maternal age, and delivery date (corresponding to improved clinical practice).Conclusion(s): Predictive models based on delivery data had very good predictive accuracy for early and late neonatal mortality.
Predictors for neonatal outcomes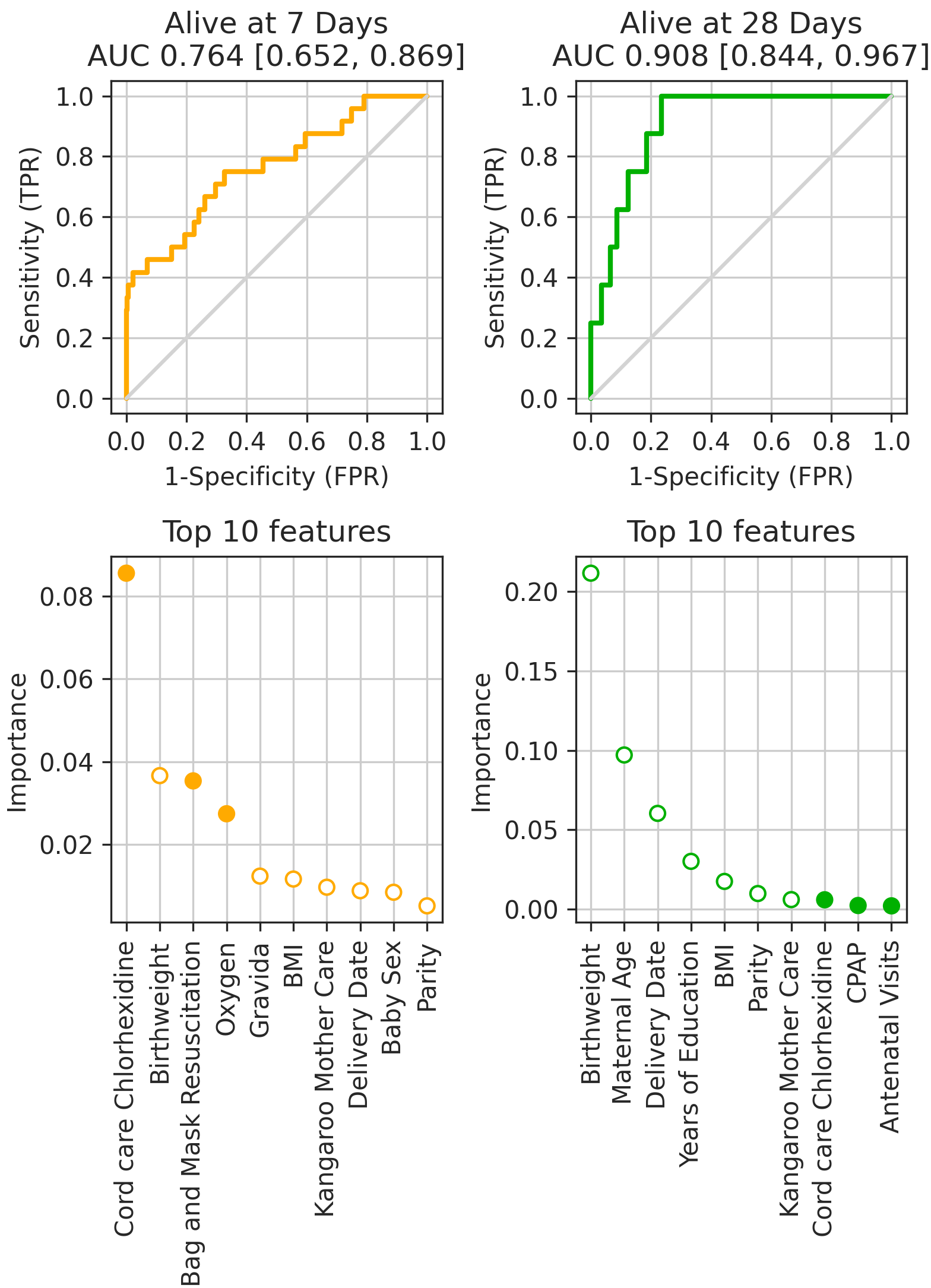 Predictors for neonatal outcomes
Predictors for neonatal outcomes
Objective: To develop predictive models for early (0-6 days) and late (7-27 days) neonatal mortality.
Design/Methods: This analysis was conducted using data from the Preterm Resources, Education, and Effective Management of Infants (PREEMI) study, which collected prospective data on pregnancies and delivery outcomes (n=11,543) up to 42 days post-partum in Lusaka, Zambia. We used advanced and conventional machine learning modelling methods and a stacking ensemble approach the develop the predictive models. We included antenatal and delivery related clinical variables as predictors for early and late neonatal mortality. Variables were grouped into pregnancy outcomes (alive, miscarriage, stillbirth, neonatal death), gestation age (last menstrual period, delivery date, method of determining gestation), confounders (maternal age, years of education, parity, BMI, ANC visits, delivered by, delivery location, mode of delivery, sex, birthweight, multiple birth, and gravida), and neonatal treatment (antibiotics, CPAP, oxygen, dexamethasone, KMC, Chlorhexidine for cord care, bag and mask resuscitation). The top predictors for the models were measured with a permutation-shuffle approach. The data was divided into training (20%) and test (80%) datasets. Machine learning based models were used to predict early and late neonatal mortality.
Results: The models had good predictive accuracy for both early and late neonatal mortality with AUC values of 0.76 and 0.90 respectively (Table 1). The first row shows the performance of the classifiers on a hold-out test set corresponding to the latest 20% of collected data, thus simulating a prospective prediction scenario. The second row identifies the most important features for the classifiers. Filled dots indicate modifiable or actionable features. The top three predictors for early neonatal mortality were chlorhexidine for cord care, birthweight, and bag and mask resuscitation. The top three predictors for late neonatal mortality were birthweight, maternal age, and delivery date (corresponding to improved clinical practice).Conclusion(s): Predictive models based on delivery data had very good predictive accuracy for early and late neonatal mortality.
Predictors for neonatal outcomes
 Predictors for neonatal outcomes
Predictors for neonatal outcomes