Neonatal General
Category: Abstract Submission
Neonatology General 4
394 - Maternal And Neonatal Risk Stratification For Development Of Neonatal Lenticular Striate Vasculopathy (LSV) Division of Neonatology at Stony Brook Children’s Hospital
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 394
Publication Number: 394.134
Publication Number: 394.134
Russell D. Himmelstein, Stony Brook Children's Hospital, East Setauket, NY, United States; Shanthy Sridhar, Stony Brook Children's Hospital, StonyBrook, NY, United States

Russell D. Himmelstein, MD
Resident
Stony Brook Children's Hospital
East Setauket, New York, United States
Presenting Author(s)
Background: LSV is an echodensity of the lenticulostriate branches of the middle cerebral arteries in the region of the basal ganglia and/or thalamus and a common finding in neonatal ultrasounds performed in the NICU. However, its significance remains unknown. Neonates with this finding often get a congenital work-up done based on HUS findings in the absence of clinical or predisposing factors.
Objective: The aim of the study is to assess risk stratification and compare maternal and neonatal risk factors for neonates with and without LSV.
Design/Methods: This is a retrospective epidemiology study on infants admitted to SBUH NICU from January 2016 through December 2020. All infants who had a head ultrasound done and who had mineralizing vasculopathy reported were included in the study. Each neonate with LSV was then matched by gestational age, weight, and birth year to controls without LSV. Neonatal and maternal risk factors were then evaluated and odds ratio calculated for each risk factor to determine any association with the finding of LSV.
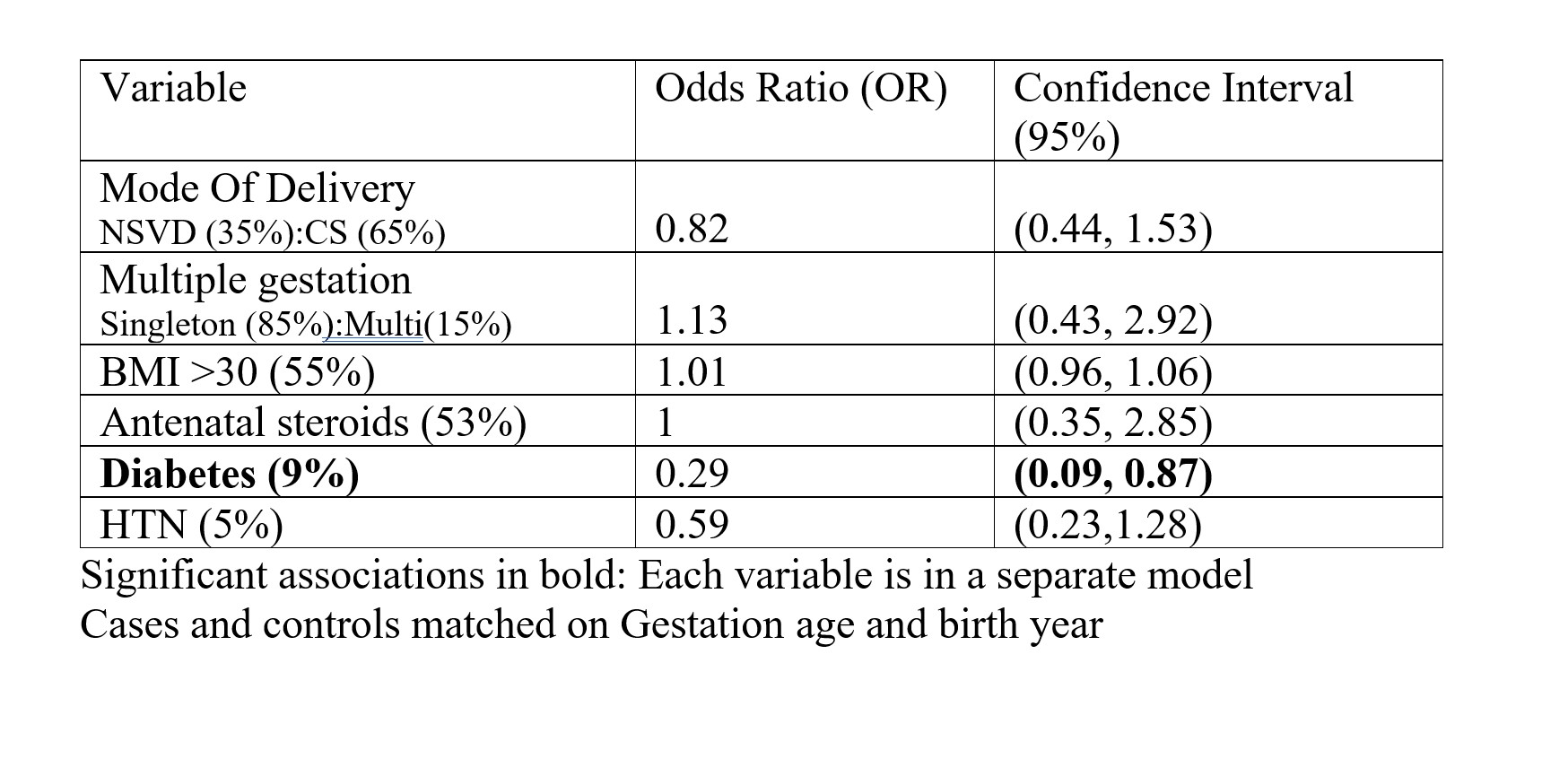
Results: Out of the 76 neonates with LSV, one tested positive for CMV and received antiviral treatment. All infants with LSV tested negative for toxoplasmosis and were without chorioretinitis. Neonatal demographics as listed in Table 1 showed no significant association between infants with or without LSV. Maternal demographics (Table 2) showed an OR 0.29 (CI .09-0.87) for maternal diabetes. The average day of life when LSV was identified ranged from 10-14 days, regardless of gestational age (Table 3). None of the ultrasounds done at birth showed LSV.Conclusion(s): While previously associated with TORCH infections, there seems to be no specific maternal or neonatal risk factors for development of neonatal LSV. This is important as an infectious disease workup including eye exam may not be necessary for these infants. This study is limited in that it was a cohort and relatively small sample size. As LSV developed within the same postnatal time across gestational age, the presence may very well be a normal stage of postnatal brain development. Future work may involve evaluation of the neurodevelopment outcomes in infants with LSV compared to those without, as this has not yet been studied.
CVCV RH.pdf
Table 2. Maternal Demographics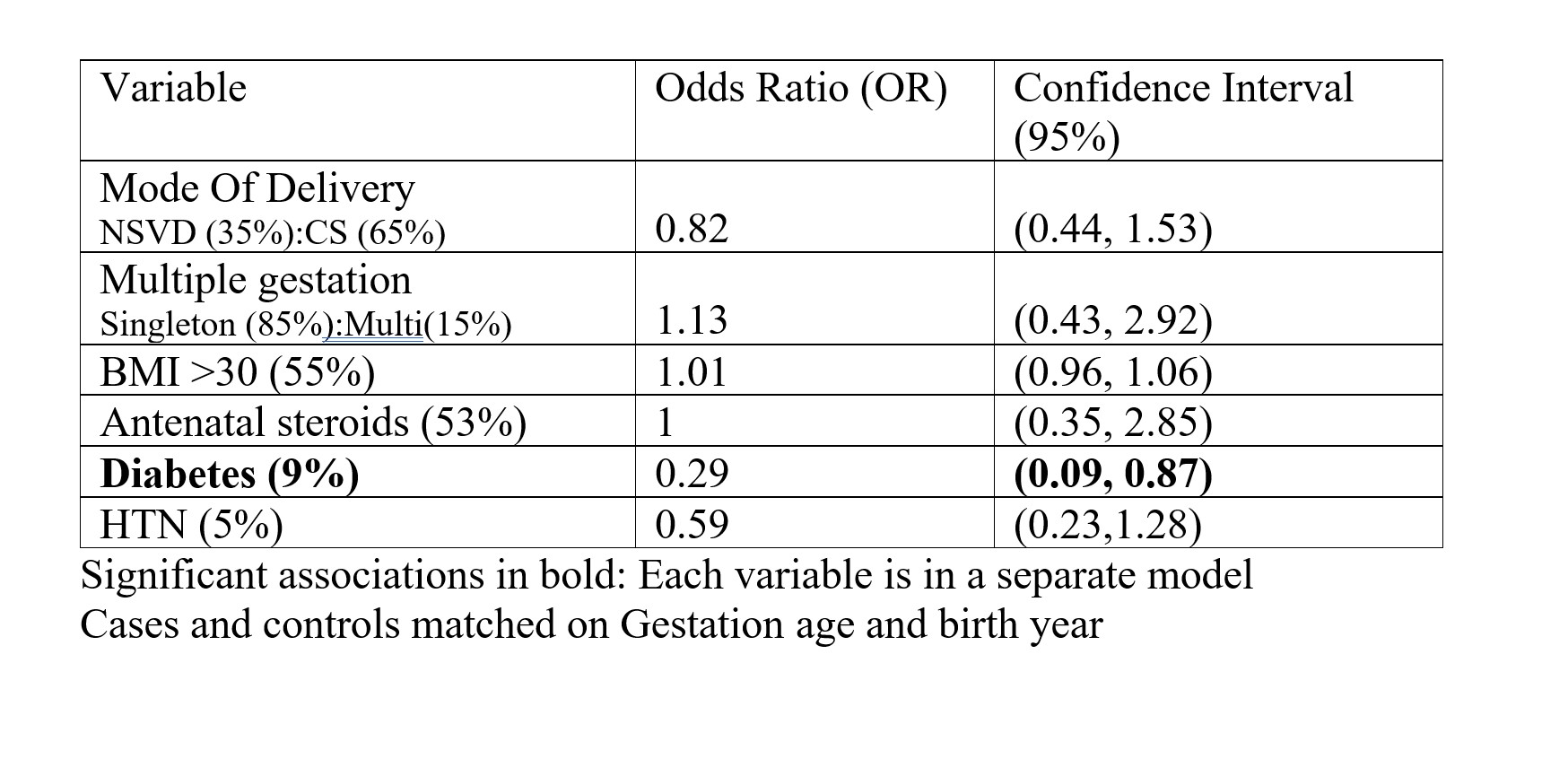
Objective: The aim of the study is to assess risk stratification and compare maternal and neonatal risk factors for neonates with and without LSV.
Design/Methods: This is a retrospective epidemiology study on infants admitted to SBUH NICU from January 2016 through December 2020. All infants who had a head ultrasound done and who had mineralizing vasculopathy reported were included in the study. Each neonate with LSV was then matched by gestational age, weight, and birth year to controls without LSV. Neonatal and maternal risk factors were then evaluated and odds ratio calculated for each risk factor to determine any association with the finding of LSV.
Results: Out of the 76 neonates with LSV, one tested positive for CMV and received antiviral treatment. All infants with LSV tested negative for toxoplasmosis and were without chorioretinitis. Neonatal demographics as listed in Table 1 showed no significant association between infants with or without LSV. Maternal demographics (Table 2) showed an OR 0.29 (CI .09-0.87) for maternal diabetes. The average day of life when LSV was identified ranged from 10-14 days, regardless of gestational age (Table 3). None of the ultrasounds done at birth showed LSV.Conclusion(s): While previously associated with TORCH infections, there seems to be no specific maternal or neonatal risk factors for development of neonatal LSV. This is important as an infectious disease workup including eye exam may not be necessary for these infants. This study is limited in that it was a cohort and relatively small sample size. As LSV developed within the same postnatal time across gestational age, the presence may very well be a normal stage of postnatal brain development. Future work may involve evaluation of the neurodevelopment outcomes in infants with LSV compared to those without, as this has not yet been studied.
CVCV RH.pdf
Table 2. Maternal Demographics