Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up I
451 - Maternal overweight and obesity’s impact on long-term neurodevelopmental outcomes in premature infants (<29 weeks) at 18-24 months corrected age
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 451
Publication Number: 451.121
Publication Number: 451.121
Marina Journault, University of Calgary, CALGARY, AB, Canada; Prashanth Murthy, Murthy Medicine Professional Corporation, Calgary Zone, AB, Canada; Neha Bansal, University of Calgary, Calgary, AB, Canada; Selphee Tang, Alberta Health Services, Calgary, AB, Canada; Essa Al Awad, University of Calgary, Calgary, AB, Canada; Dianne Creighton, University of Ca=ary Cumming School of Medicine, Calgary, AB, Canada; Susan Crawford, University of Ca=ary Cumming School of Medicine, calgary, AB, Canada; Abhay K. Lodha, University of Calgary, Calgary, AB, Canada

Marina Journault, MD, FRCPC
Neonatal Perinatal Medicine Fellow
University of Calgary
CALGARY, Alberta, Canada
Presenting Author(s)
Background: Increasing rates of obesity are of growing concern to maternal and child health as mothers with obesity are at risk of pregnancy complications. Infants of mothers with overweight/obese pre-pregnancy body mass index (BMI) may also be at risk of significant neurodevelopmental disorders. The relationship between maternal pre-pregnancy BMI and neurodevelopmental outcomes in preterm infants is not yet clearly defined.
Objective: To determine the association of pre-pregnancy BMI of mothers of infants born < 29 weeks gestational age (GA) and neurodevelopmental impairment (NDI) at 18-24 months corrected age (CA).
Design/Methods: Preterm infants born < 29 weeks GA between January 2005 and December 2015 evaluated in the neonatal follow-up clinic at 18-24 months CA were included. Demographic characteristics as well as neurodevelopmental status including Bayley-III cognitive, language, and motor scores and sensory impairments were compared between three groups based on maternal pre-pregnancy BMI (BMI1 [18.5-24.9 kg/m2] vs. BMI2 [25-29.9 kg/m2] vs. BMI3 [≥30 kg/m2]) using univariate and multivariable regression models. The primary outcome was a composite of death or NDI.
NDI was defined as the presence of Bayley-III < 85 on one or more of the cognitive, motor, or language composite scores, any cerebral palsy (GMFCS ≥1), sensorineural or mixed hearing impairment, or unilateral or bilateral visual impairment.
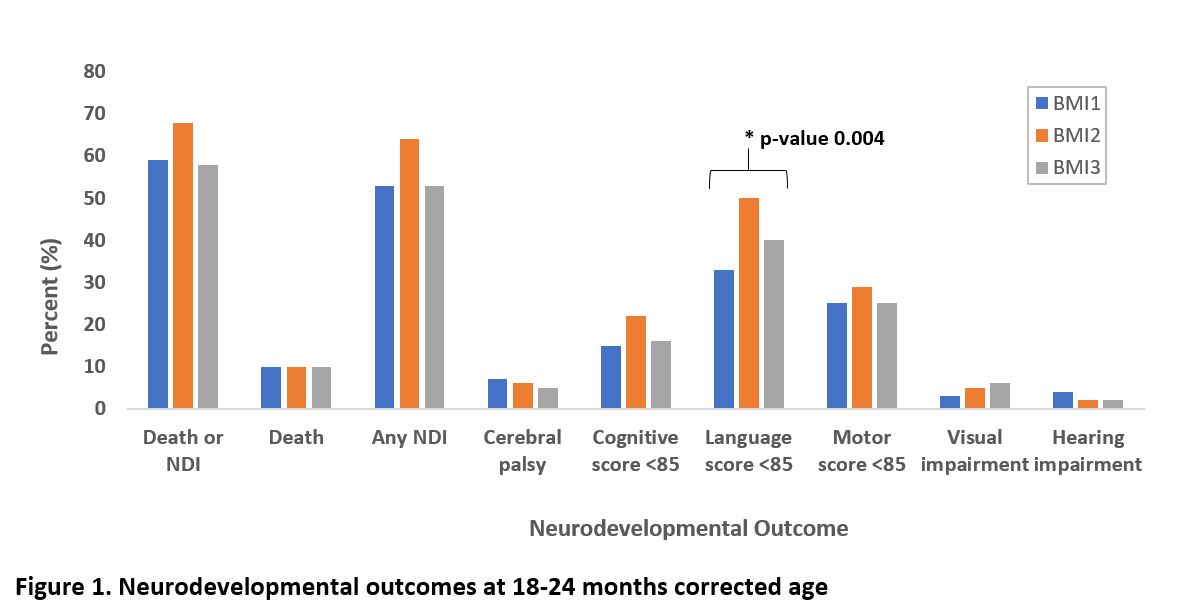
Results: Of 771 eligible infants, 53 not seen in the follow-up clinic and 21 born to mothers with BMI < 18.5 kg/m2 were excluded. Of the remaining 697 participants, 315 (45%) infants were in BMI1, 235 (34%) in BMI2, and 147 (21%) in BMI3 groups. Infants in BMI1, BMI2, and BMI3 groups had mean (SD) birth weight of 897 (231), 854 (208), and 867 (234) grams and median GA (IQR) of 27 (3), 26 (2), and 27 (3) weeks respectively (Table 1). Rates of associated impairments are shown in Figure 1. The odds of a composite of death or NDI in BMI2 vs. BMI1 and BMI3 vs BMI1 groups were 1.33 (95%CI 0.86-2.06) and 0.76 (95%CI 0.47-1.22) respectively (Table 2). Infants born to mothers in the BMI2 group had twice the odds of scoring < 85 on the Bayley-III language composite than those in BMI1 (adjusted odds ratio 2.06 [95% CI; 1.28-3.32]).Conclusion(s): Pre-pregnancy body mass index was not associated with death or neurodevelopmental impairment in very preterm infants at 18-24 months corrected age. However, infants born to mothers who were overweight were more likely to have lower language scores.
CV-MJournaultCV - MJournault.pdf
Figure 1. Neurodevelopmental outcomes at 18-24 months corrected age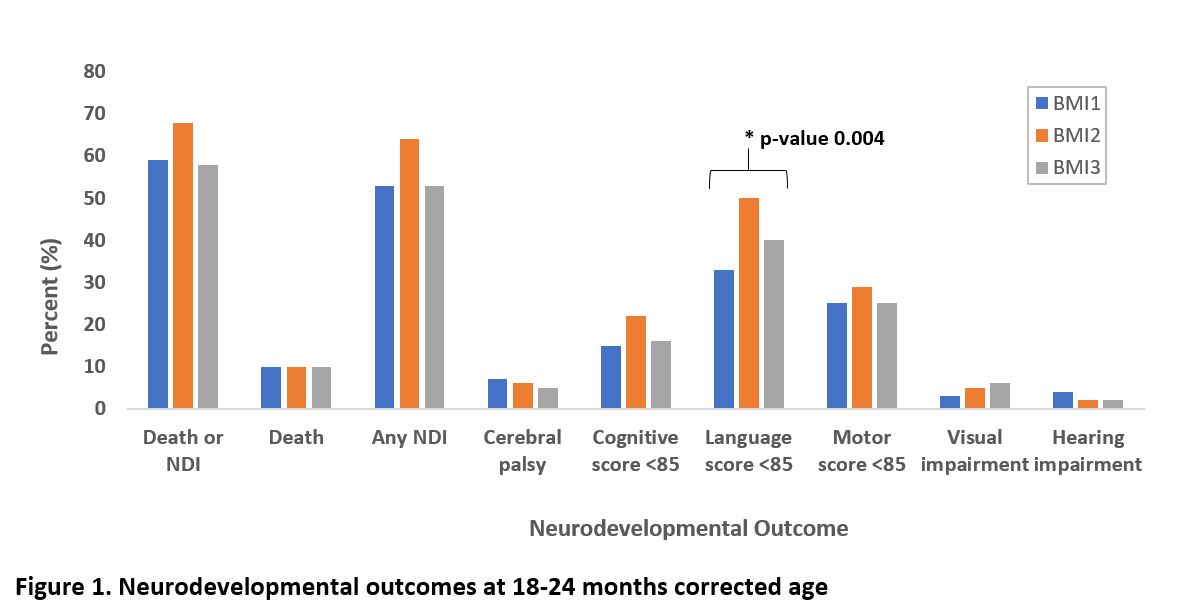
Objective: To determine the association of pre-pregnancy BMI of mothers of infants born < 29 weeks gestational age (GA) and neurodevelopmental impairment (NDI) at 18-24 months corrected age (CA).
Design/Methods: Preterm infants born < 29 weeks GA between January 2005 and December 2015 evaluated in the neonatal follow-up clinic at 18-24 months CA were included. Demographic characteristics as well as neurodevelopmental status including Bayley-III cognitive, language, and motor scores and sensory impairments were compared between three groups based on maternal pre-pregnancy BMI (BMI1 [18.5-24.9 kg/m2] vs. BMI2 [25-29.9 kg/m2] vs. BMI3 [≥30 kg/m2]) using univariate and multivariable regression models. The primary outcome was a composite of death or NDI.
NDI was defined as the presence of Bayley-III < 85 on one or more of the cognitive, motor, or language composite scores, any cerebral palsy (GMFCS ≥1), sensorineural or mixed hearing impairment, or unilateral or bilateral visual impairment.
Results: Of 771 eligible infants, 53 not seen in the follow-up clinic and 21 born to mothers with BMI < 18.5 kg/m2 were excluded. Of the remaining 697 participants, 315 (45%) infants were in BMI1, 235 (34%) in BMI2, and 147 (21%) in BMI3 groups. Infants in BMI1, BMI2, and BMI3 groups had mean (SD) birth weight of 897 (231), 854 (208), and 867 (234) grams and median GA (IQR) of 27 (3), 26 (2), and 27 (3) weeks respectively (Table 1). Rates of associated impairments are shown in Figure 1. The odds of a composite of death or NDI in BMI2 vs. BMI1 and BMI3 vs BMI1 groups were 1.33 (95%CI 0.86-2.06) and 0.76 (95%CI 0.47-1.22) respectively (Table 2). Infants born to mothers in the BMI2 group had twice the odds of scoring < 85 on the Bayley-III language composite than those in BMI1 (adjusted odds ratio 2.06 [95% CI; 1.28-3.32]).Conclusion(s): Pre-pregnancy body mass index was not associated with death or neurodevelopmental impairment in very preterm infants at 18-24 months corrected age. However, infants born to mothers who were overweight were more likely to have lower language scores.
CV-MJournaultCV - MJournault.pdf
Figure 1. Neurodevelopmental outcomes at 18-24 months corrected age