Emergency Medicine: All Areas
Category: Abstract Submission
4: Emergency Medicine I
42 - Overlap in medical complexity and mental/behavioral disorders among children presenting to the emergency department
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 42
Publication Number: 42.103
Publication Number: 42.103
Sriram Ramgopal, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Denise M. Goodman, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Tracie L. Smith, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Kristin Kan, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Carolyn C. Foster, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
- SR
Sriram Ramgopal, MD (he/him/his)
Assistant Professor
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Patients with both medical complexity and mental/behavioral health disorder presenting to the emergency department (ED) have complex needs for which the health system may be poorly suited to address.
Objective: To assess the overlap, rate of admission and resource use among children with medical complexity and mental/behavioral health (MBH) disorders presenting to the ED.
Design/Methods: We examined the overlap and medical needs of patients < 21 years with medical complexity and MBH disorders who had an ED encounter in 2018 from the Pediatric Health Information System (PHIS; representing 45 US children’s hospitals) and the Illinois Hospital Association COMP dataset. We used the Complex Chronic Condition (CCC) algorithm and the Child and Adolescent Mental Health Disorders Classification System to characterize CCC and MBH, respectively. We identified the extent of overlap between CCC and MBH. Among patients meeting both CCC and MBH criteria, we identified if a primary discharge diagnosis of an MBH was independently associated with a composite outcome of admission/transfer to another institution using a multivariable linear mixed model adjusting for CCC type, age, and payor status.
Results: 2,356,185 encounters were identified in the PHIS dataset, of which 132,853 (5.6%) had a CCC only, 31,872 (1.4%) had an MBH only, and 7,586 (0.3%) had both (Figure). From the COMP dataset, 5,681,503 encounters were identified, of which 175,946 (3.1%) had a CCC, 95,501 (1.7%) had an MBH, and 9,788 (0.2%) had both. The most common types of CCCs among patients who had both a CCC and MBH were neuromuscular, technology dependence, metabolic, and cardiovascular disease. The most common MBH disorders were anxiety disorder, depressive disorders, and ADHD (Table 1). For patients with an overlapping MBH and CCC a higher proportion of these patients (87.0% PHIS, 61.7% COMP) were admitted/transferred compared to other groups (Table 2). Among patients with an MBH and CCC, the presence of a MBH as the principal discharge diagnosis was independently associated with admission/transfer (adjusted odds ratio [aOR] 1.31, 95% confidence interval [CI] 1.09-1.18 for PHIS; aOR 3.80, 95% CI 3.39-4.26 for COMP).Conclusion(s): MBH occur in approximately 5% of patients with a CCC who presented to the ED. These resource-intensive patients have a higher need for admission/transfer relative to even other patients with CCC, particularly when they are presenting primarily for an MBH-related issue.
Figure. Overlap of mental/behavioral health disorder and complex chronic conditions in the two study cohorts using the a) Pediatric Health Information System and b) COMP datasets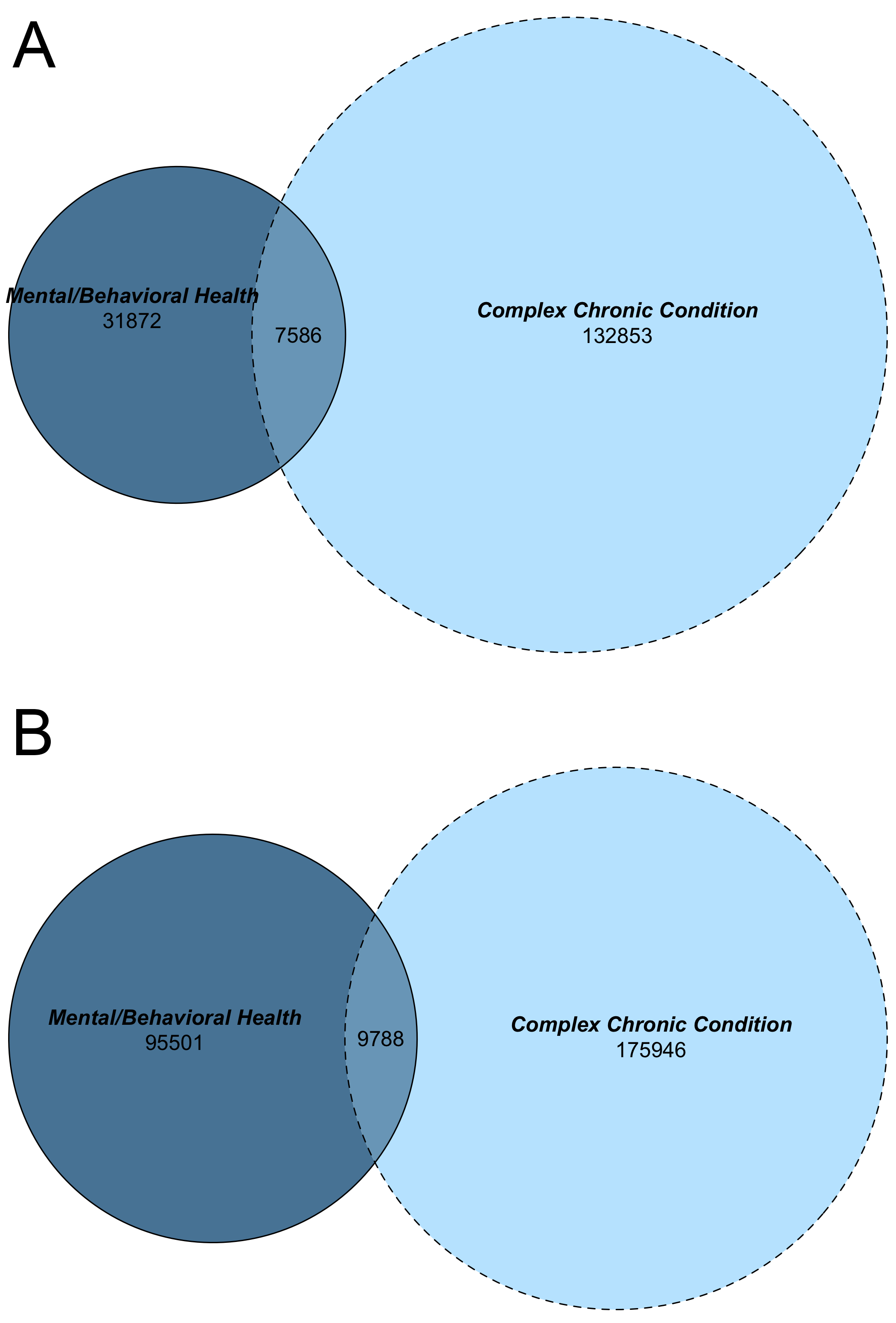
Table 1. Outcomes among patients in both cohorts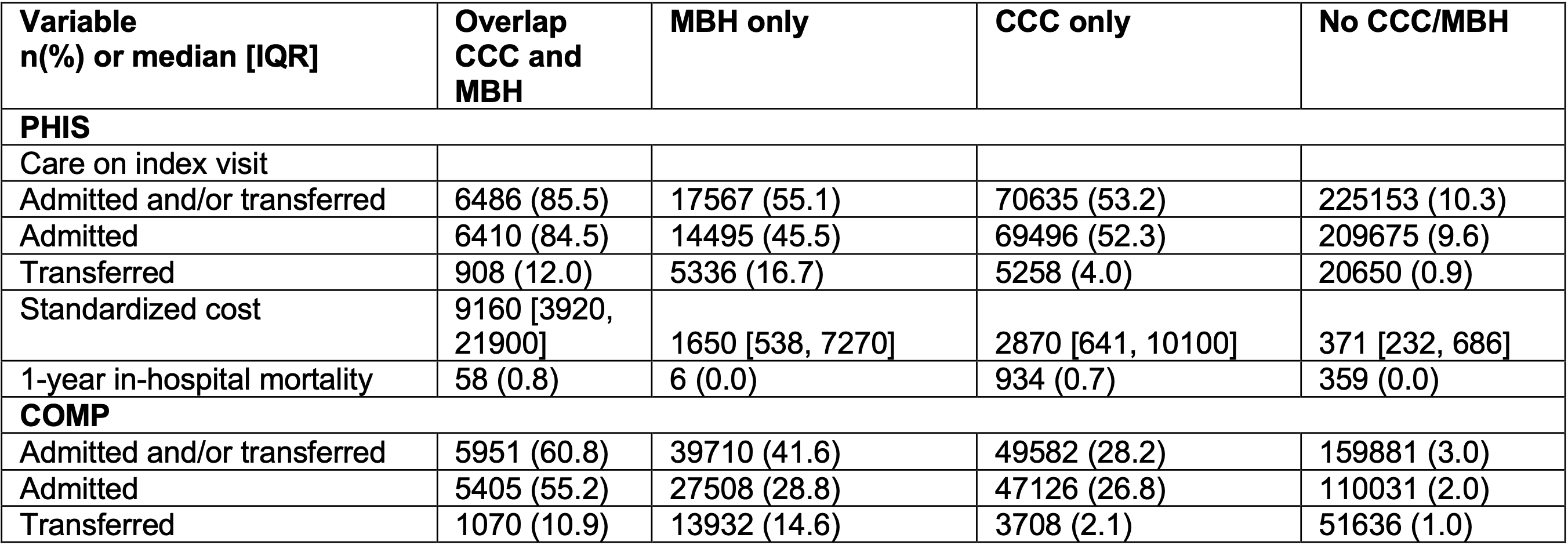 CCC, complex chronic condition; MBH, mental behavioral health; PHIS, Pediatric Health Information System; disorder.
CCC, complex chronic condition; MBH, mental behavioral health; PHIS, Pediatric Health Information System; disorder.
Objective: To assess the overlap, rate of admission and resource use among children with medical complexity and mental/behavioral health (MBH) disorders presenting to the ED.
Design/Methods: We examined the overlap and medical needs of patients < 21 years with medical complexity and MBH disorders who had an ED encounter in 2018 from the Pediatric Health Information System (PHIS; representing 45 US children’s hospitals) and the Illinois Hospital Association COMP dataset. We used the Complex Chronic Condition (CCC) algorithm and the Child and Adolescent Mental Health Disorders Classification System to characterize CCC and MBH, respectively. We identified the extent of overlap between CCC and MBH. Among patients meeting both CCC and MBH criteria, we identified if a primary discharge diagnosis of an MBH was independently associated with a composite outcome of admission/transfer to another institution using a multivariable linear mixed model adjusting for CCC type, age, and payor status.
Results: 2,356,185 encounters were identified in the PHIS dataset, of which 132,853 (5.6%) had a CCC only, 31,872 (1.4%) had an MBH only, and 7,586 (0.3%) had both (Figure). From the COMP dataset, 5,681,503 encounters were identified, of which 175,946 (3.1%) had a CCC, 95,501 (1.7%) had an MBH, and 9,788 (0.2%) had both. The most common types of CCCs among patients who had both a CCC and MBH were neuromuscular, technology dependence, metabolic, and cardiovascular disease. The most common MBH disorders were anxiety disorder, depressive disorders, and ADHD (Table 1). For patients with an overlapping MBH and CCC a higher proportion of these patients (87.0% PHIS, 61.7% COMP) were admitted/transferred compared to other groups (Table 2). Among patients with an MBH and CCC, the presence of a MBH as the principal discharge diagnosis was independently associated with admission/transfer (adjusted odds ratio [aOR] 1.31, 95% confidence interval [CI] 1.09-1.18 for PHIS; aOR 3.80, 95% CI 3.39-4.26 for COMP).Conclusion(s): MBH occur in approximately 5% of patients with a CCC who presented to the ED. These resource-intensive patients have a higher need for admission/transfer relative to even other patients with CCC, particularly when they are presenting primarily for an MBH-related issue.
Figure. Overlap of mental/behavioral health disorder and complex chronic conditions in the two study cohorts using the a) Pediatric Health Information System and b) COMP datasets
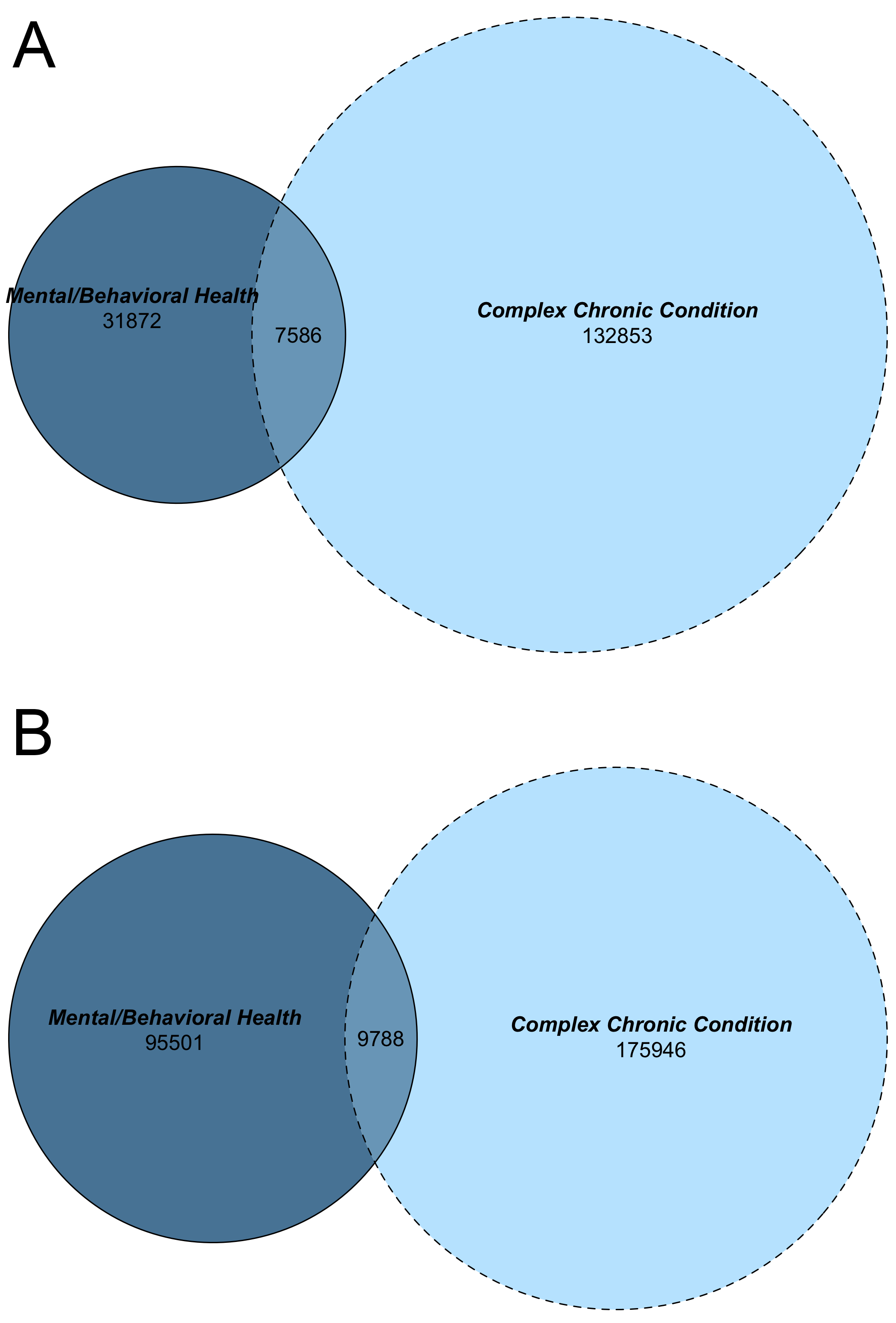
Table 1. Outcomes among patients in both cohorts
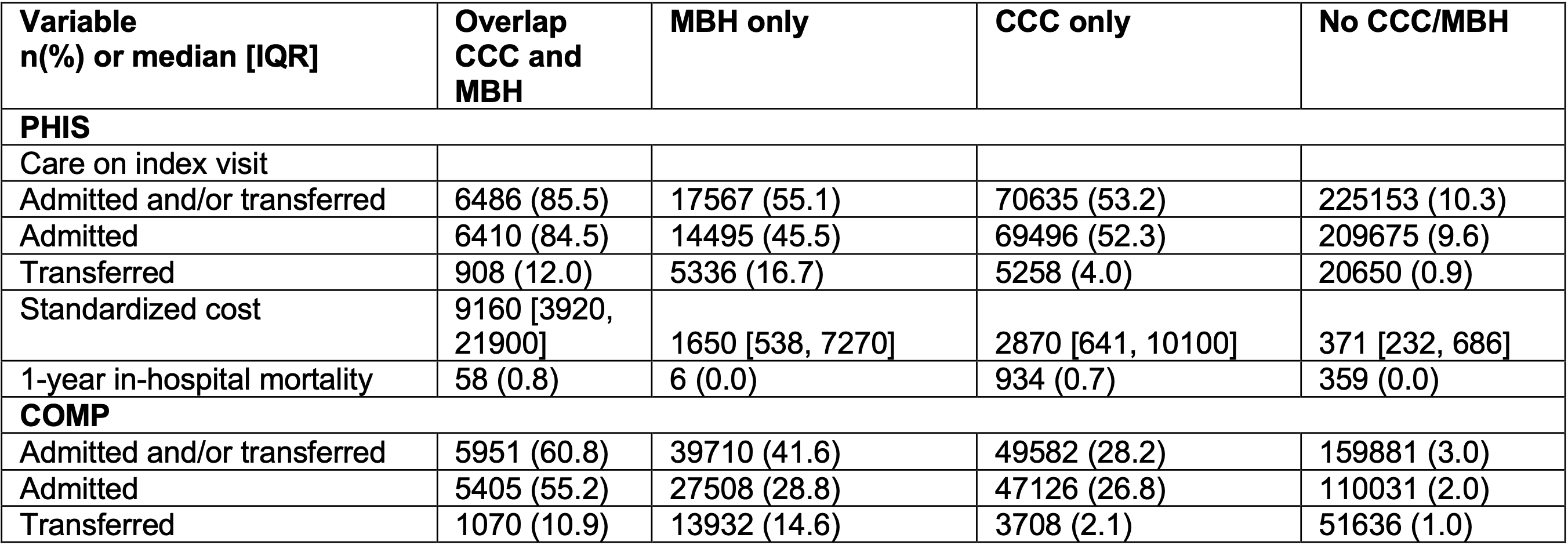 CCC, complex chronic condition; MBH, mental behavioral health; PHIS, Pediatric Health Information System; disorder.
CCC, complex chronic condition; MBH, mental behavioral health; PHIS, Pediatric Health Information System; disorder.