Neonatal General
Category: Abstract Submission
Neonatology General 4
395 - Owlet Smart Sock 3 Accuracy on Preterm Infants in the NICU
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 395
Publication Number: 395.134
Publication Number: 395.134
Brandon Tomlin, University of Utah School of Medicine, Salt Lake City, UT, United States; Heather S. Day, University of Utah School of Medicine, Cottonwood Heights, UT, United States; Brandy J. Petersen, University of Utah School of Medicine, west jordan, UT, United States; Trisha A. Marchant, University of Utah School of Medicine, Salt Lake City, UT, United States; Cory Jones, Owlet Baby Care, Orem, UT, United States; Micaela L. Thomas, University of Utah, Draper, UT, United States; Baylee D. Mayoh, University of Utah Health, Draper, UT, United States; Belinda Chan, University of Utah, Salt Lake City, UT, United States

Brandon Tomlin, MD (he/him/his)
Physician Fellow, Neonatal-perinatal Medicine
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Continuous pulse oximetry monitoring is vital for the care of preterm infants in the NICU. The current standard pulse oximeter requires a wired system to function, hindering infant movement and care. The recent Owlet Smart Sock 3 (OSS3) wearable monitor introduces wireless connectivity; however, there is no accuracy data for preterm infants.
Objective: To assess the OSS3 agreement of measuring Peripheral Oxygen Saturation (SpO2) and heart rate (HR) compared to the standard pulse oximeter on preterm infants in the NICU.
Design/Methods: This observational study compares the measurements of the OSS3 with Masimo SET on 1.7-2.3 kg infants admitted to the University of Utah NICU who had no significant anomalies, deformities, or medical instability. Pulse oximetry data were collected simultaneously for 60 minutes on quiet infants with one device on each foot. Raw data were aligned by time epoch and filtered for movement artifacts or poor tracings. Agreement of the devices was assessed using average root mean square error (ARMS), Bland-Altman, Prevalence and Bias Adjusted Kappa (PABAK), and Pearson’s correlation coefficient analyses.
Results: The average gestational age and weight of the 28 enrolled infants at the time of study were 36±3 weeks and 2.0±0.2 kg. Over 21 hours of captured comparative data was analyzed after filtration due to excessive motion artifacts or device failures, which occurred equally in both devices. The OSS3’s ARMS was 2.32% for SpO2 in the 70-100% range when compared to the Masimo device. The SpO2 reading bias of the Owlet was positive 0.03% with limits of agreement (LOA) -4.6% to 4.5% (Figure 1). Both devices were highly agreeable in indicating if the SpO2 was either < or > 90% (PABAK = 0.94). The HR reading bias of the Owlet was positive 1.3 beats per minute (LOA -6.1 to 3.4) (Figure 2). The SpO2 and HR were correlated between the two devices (r = 0.71 (95% CI: 0.71 to 0.72) and 0.98 (95% CI: 0.98 to 0.99) respectively). Conclusion(s): The wearable OSS3 provides comparable accuracy to the standard pulse oximeter in preterm infants while eliminating wired connectivity. Both OSS3 and another standard pulse oximeter are equally limited by motion artifact on active infants, and their SpO2 precision decreases as SpO2 decreases. Further research is needed on preterm infants to overcome these challenges.
The study is sponsored by an Owlet investigator-initiated research grant.
Figure 1.png) Bland-Altman plot for SpO2 measurements of Masimo and Owlet devices. LOA -4.6% to 4.5%
Bland-Altman plot for SpO2 measurements of Masimo and Owlet devices. LOA -4.6% to 4.5%
Figure 2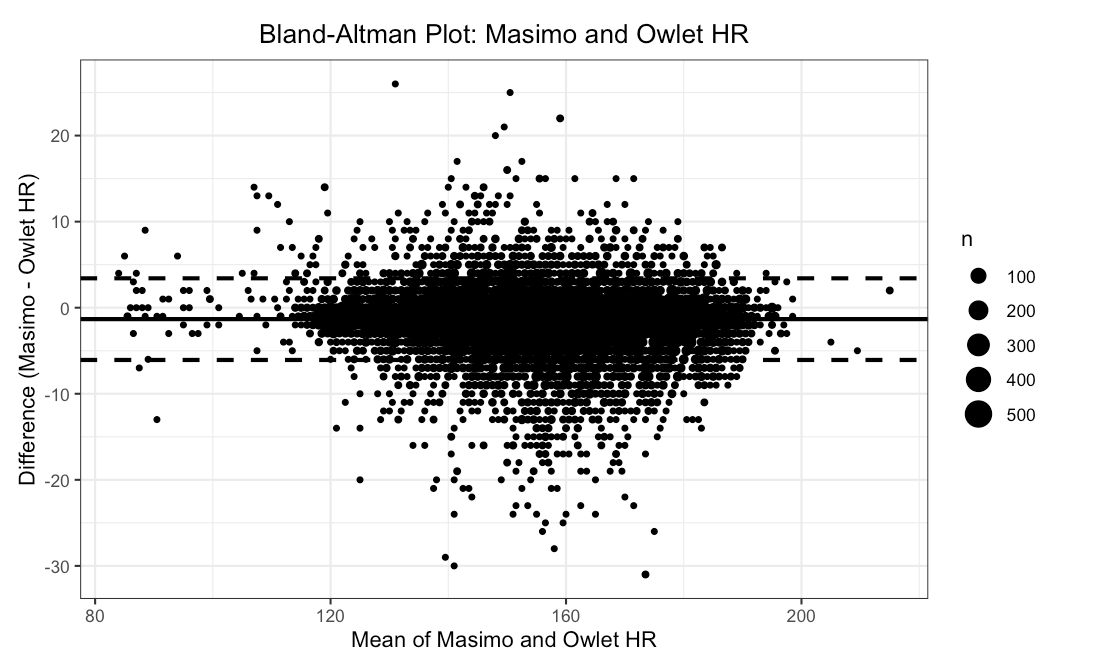 Bland-Altman plot of HR measurements of Masimo and Owlet devices. LOA -6.1 to 3.4 BPM.
Bland-Altman plot of HR measurements of Masimo and Owlet devices. LOA -6.1 to 3.4 BPM.
Objective: To assess the OSS3 agreement of measuring Peripheral Oxygen Saturation (SpO2) and heart rate (HR) compared to the standard pulse oximeter on preterm infants in the NICU.
Design/Methods: This observational study compares the measurements of the OSS3 with Masimo SET on 1.7-2.3 kg infants admitted to the University of Utah NICU who had no significant anomalies, deformities, or medical instability. Pulse oximetry data were collected simultaneously for 60 minutes on quiet infants with one device on each foot. Raw data were aligned by time epoch and filtered for movement artifacts or poor tracings. Agreement of the devices was assessed using average root mean square error (ARMS), Bland-Altman, Prevalence and Bias Adjusted Kappa (PABAK), and Pearson’s correlation coefficient analyses.
Results: The average gestational age and weight of the 28 enrolled infants at the time of study were 36±3 weeks and 2.0±0.2 kg. Over 21 hours of captured comparative data was analyzed after filtration due to excessive motion artifacts or device failures, which occurred equally in both devices. The OSS3’s ARMS was 2.32% for SpO2 in the 70-100% range when compared to the Masimo device. The SpO2 reading bias of the Owlet was positive 0.03% with limits of agreement (LOA) -4.6% to 4.5% (Figure 1). Both devices were highly agreeable in indicating if the SpO2 was either < or > 90% (PABAK = 0.94). The HR reading bias of the Owlet was positive 1.3 beats per minute (LOA -6.1 to 3.4) (Figure 2). The SpO2 and HR were correlated between the two devices (r = 0.71 (95% CI: 0.71 to 0.72) and 0.98 (95% CI: 0.98 to 0.99) respectively). Conclusion(s): The wearable OSS3 provides comparable accuracy to the standard pulse oximeter in preterm infants while eliminating wired connectivity. Both OSS3 and another standard pulse oximeter are equally limited by motion artifact on active infants, and their SpO2 precision decreases as SpO2 decreases. Further research is needed on preterm infants to overcome these challenges.
The study is sponsored by an Owlet investigator-initiated research grant.
Figure 1
.png) Bland-Altman plot for SpO2 measurements of Masimo and Owlet devices. LOA -4.6% to 4.5%
Bland-Altman plot for SpO2 measurements of Masimo and Owlet devices. LOA -4.6% to 4.5%Figure 2
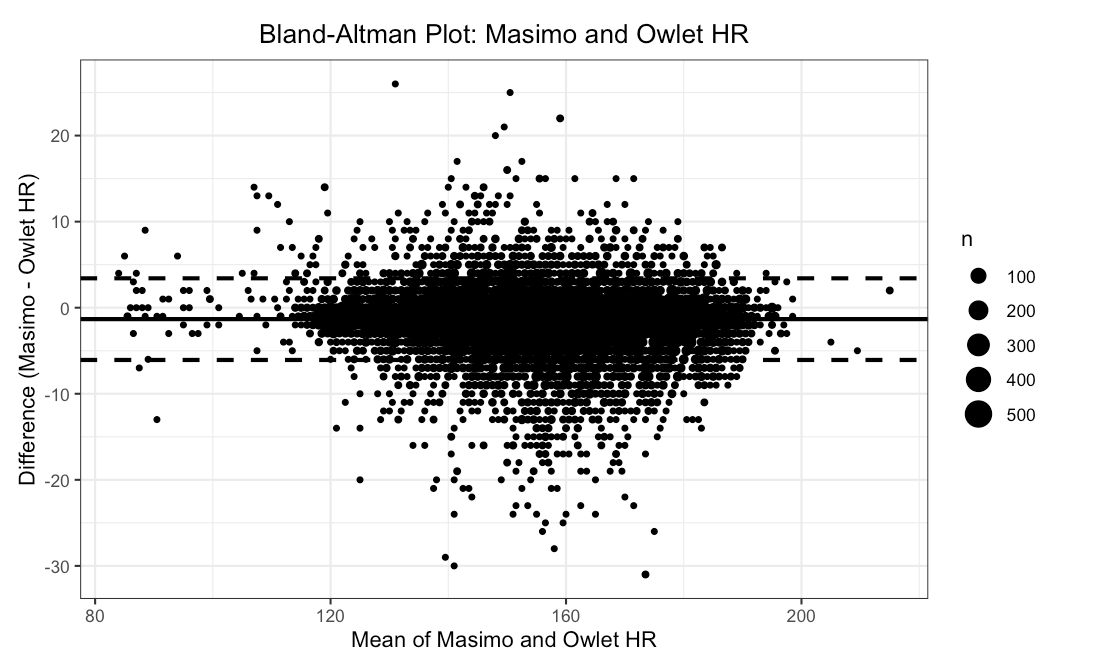 Bland-Altman plot of HR measurements of Masimo and Owlet devices. LOA -6.1 to 3.4 BPM.
Bland-Altman plot of HR measurements of Masimo and Owlet devices. LOA -6.1 to 3.4 BPM.