Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine III
69 - Parent-reported immunization status and the management of febrile young children in the pediatric emergency department
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 69
Publication Number: 69.105
Publication Number: 69.105
Molly G. Curtis, Indiana University School of Medicine, Indianapolis, IN, United States; Randall Grout, Indiana University School of Medicine, Indianapolis, IN, United States; Jessica Kanis, IU Health, Indianapolis, IN, United States; Brian Wagers, Riley Hospital for Children at Indiana University Health, zionsville, IN, United States; Lane Coffee, Indiana University School of Medicine, Indianapolis, IN, United States; Elisa Sarmiento, Indiana University School of Medicine, Emergency Medicine, Indianapolis, IN, United States; Sarah Grout, Riley Hospital for Children at Indiana University Health, Indianapolis, IN, United States; Olivia Johnson, Indiana University School of Medicine, Indianapolis, IN, United States; Sydney DiGregory, Indiana University School of Medicine, Fishers, IN, United States

Molly G. Curtis, MD
Pediatric Emergency Medicine Fellow
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Widespread H.influenzae and S.pneumoniae immunization decreased occult bacteremia and bacterial meningitis rates. Pediatric emergency medical practice evolved to favor fewer diagnostic tests for and empiric treatment of invasive bacterial infection in children aged 3-36 months. We lack evidence-based guidance on evaluation and management of unimmunized or underimmunized (UI) febrile children; it is unclear if and how vaccination status is considered by PEM providers evaluating and managing this population of patients.
Objective: To determine how parental report of immunization status in febrile pediatric emergency department (PED) patients relates to rates of diagnostic testing, interventions, and hospital admissions.
Design/Methods: Retrospective cohort study with chart review of encounters of febrile children aged 3-36 months presenting to an academic, tertiary-care PED in 2019 using ICD-10 code for fever (R50.9). Inclusion criteria were documented fever ≥38℃ and well-appearance. Encounters were excluded if there was a history of complex chronic illness or documentation of hemodynamic instability. Encounters were grouped by parent-reported vaccination status as documented by providers. Fischer’s Exact Test compared rates of diagnostic testing (serum, urine or CSF laboratory studies and chest radiographs), interventions (IV fluid bolus, IV antibiotic or steroid administration, respiratory support or breathing treatment) and hospital admissions between UI and fully immunized groups.
Results: Of the 1570 encounters reviewed to date representing January-November 2019, 938 (60%; mean age 17 months, SD 9 months) included provider-documented immunization status: 20 (2.1%) unimmunized, 54 (5.8%) underimmunized, and 864 (92.1%) fully immunized. Outcome comparison is in Table 1. UI children experienced significantly higher rates of laboratory evaluation, including CBC and blood culture, and medical intervention while in the PED. No significant differences were observed for rates of chest radiographs, hospital admissions, oral antibiotic prescription upon PED discharge or patient return to PED within 72 hours of discharge.Conclusion(s): Higher rates of laboratory testing and interventions were observed in UI versus fully immunized febrile patients at a large, academic PED, demonstrating a difference in clinical approach across these groups. Given continued vaccine hesitancy and the practice variation demonstrated in this study, further study and national guidelines are needed for the management of febrile, young, UI children presenting for emergency care.
Table 1. Differences in Management Between Groups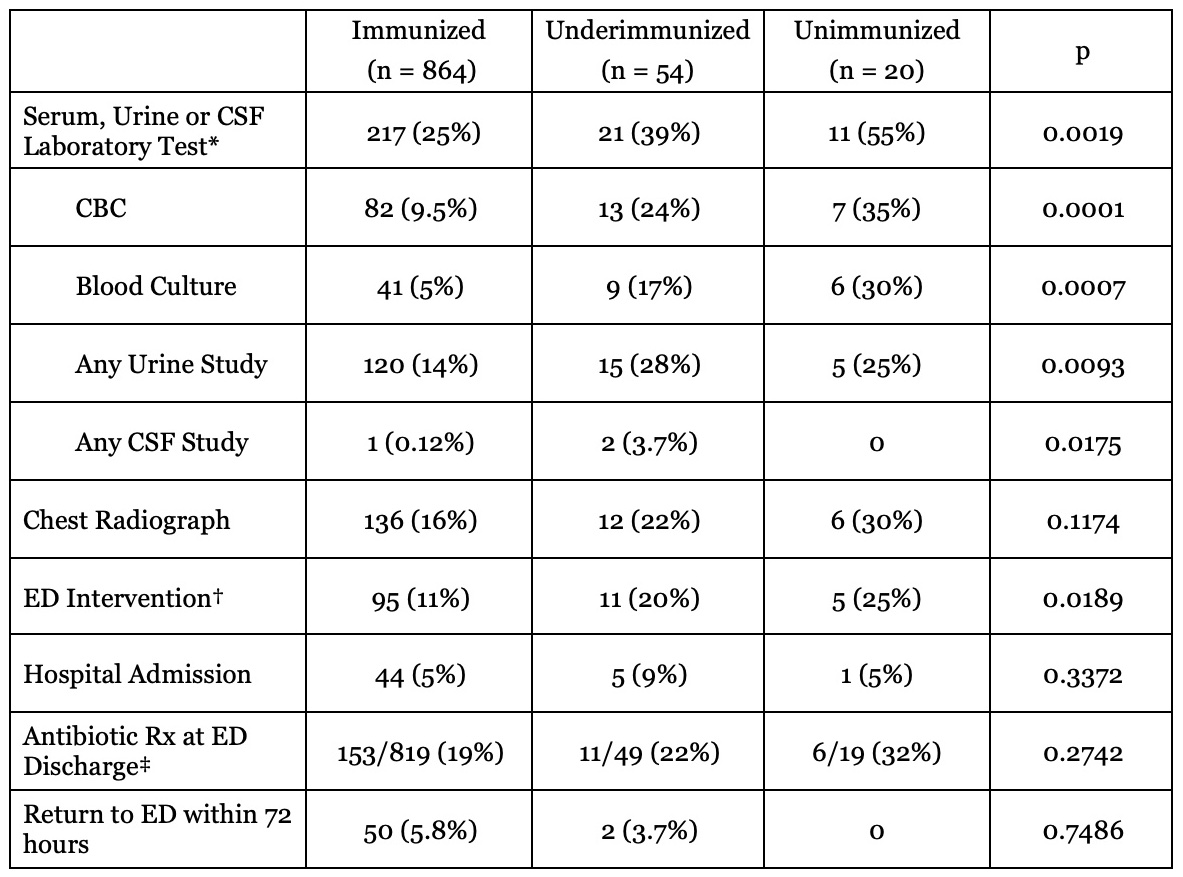 * BMP, LFT, CBC, urinalysis, urine culture, urine dip, CRP, ESR, procalcitonin, CSF studies (culture, gram stain, protein, glucose, viral studies), blood culture or other
* BMP, LFT, CBC, urinalysis, urine culture, urine dip, CRP, ESR, procalcitonin, CSF studies (culture, gram stain, protein, glucose, viral studies), blood culture or other
† IV fluid bolus, IV antibiotics, respiratory support, steroids, breathing treatment or other
‡ 50 patients admitted to hospital and 1 incomplete record not included
Objective: To determine how parental report of immunization status in febrile pediatric emergency department (PED) patients relates to rates of diagnostic testing, interventions, and hospital admissions.
Design/Methods: Retrospective cohort study with chart review of encounters of febrile children aged 3-36 months presenting to an academic, tertiary-care PED in 2019 using ICD-10 code for fever (R50.9). Inclusion criteria were documented fever ≥38℃ and well-appearance. Encounters were excluded if there was a history of complex chronic illness or documentation of hemodynamic instability. Encounters were grouped by parent-reported vaccination status as documented by providers. Fischer’s Exact Test compared rates of diagnostic testing (serum, urine or CSF laboratory studies and chest radiographs), interventions (IV fluid bolus, IV antibiotic or steroid administration, respiratory support or breathing treatment) and hospital admissions between UI and fully immunized groups.
Results: Of the 1570 encounters reviewed to date representing January-November 2019, 938 (60%; mean age 17 months, SD 9 months) included provider-documented immunization status: 20 (2.1%) unimmunized, 54 (5.8%) underimmunized, and 864 (92.1%) fully immunized. Outcome comparison is in Table 1. UI children experienced significantly higher rates of laboratory evaluation, including CBC and blood culture, and medical intervention while in the PED. No significant differences were observed for rates of chest radiographs, hospital admissions, oral antibiotic prescription upon PED discharge or patient return to PED within 72 hours of discharge.Conclusion(s): Higher rates of laboratory testing and interventions were observed in UI versus fully immunized febrile patients at a large, academic PED, demonstrating a difference in clinical approach across these groups. Given continued vaccine hesitancy and the practice variation demonstrated in this study, further study and national guidelines are needed for the management of febrile, young, UI children presenting for emergency care.
Table 1. Differences in Management Between Groups
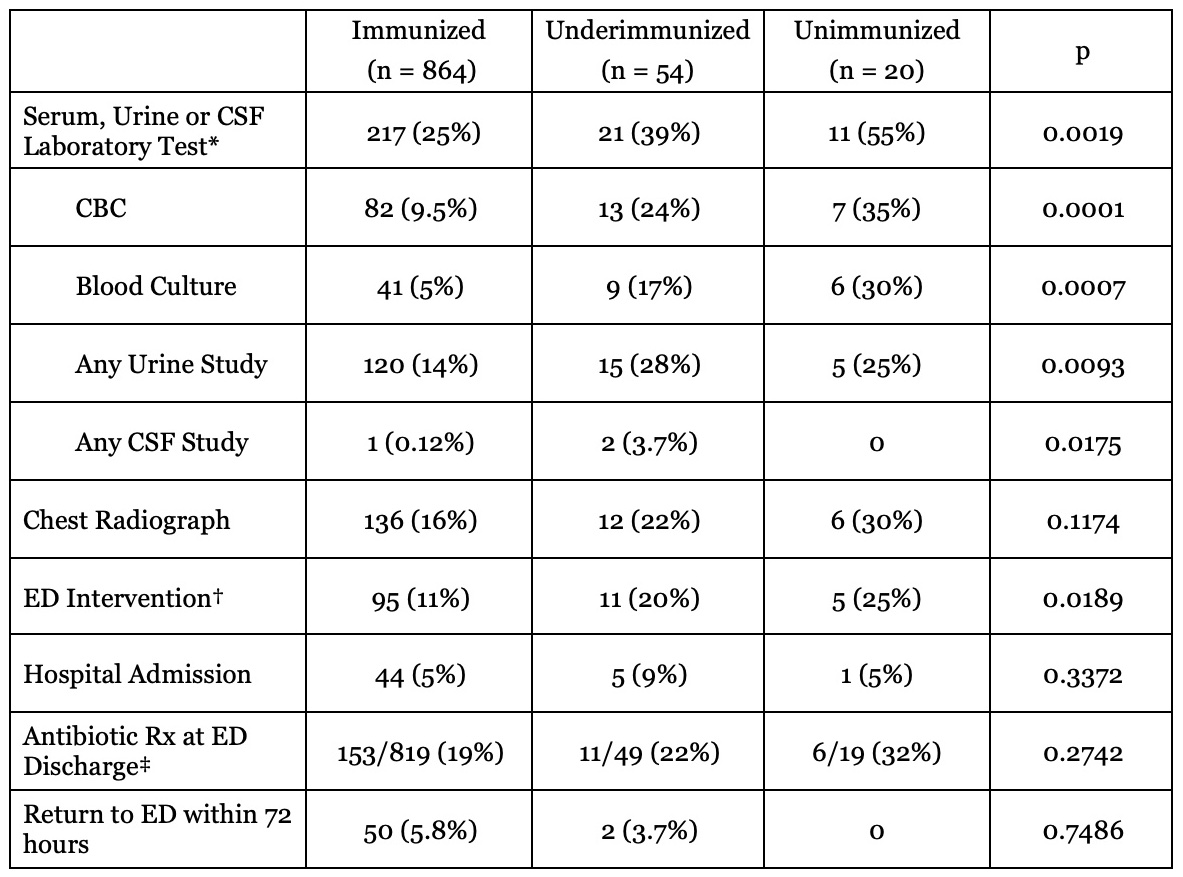 * BMP, LFT, CBC, urinalysis, urine culture, urine dip, CRP, ESR, procalcitonin, CSF studies (culture, gram stain, protein, glucose, viral studies), blood culture or other
* BMP, LFT, CBC, urinalysis, urine culture, urine dip, CRP, ESR, procalcitonin, CSF studies (culture, gram stain, protein, glucose, viral studies), blood culture or other† IV fluid bolus, IV antibiotics, respiratory support, steroids, breathing treatment or other
‡ 50 patients admitted to hospital and 1 incomplete record not included
