Cardiology
Category: Abstract Submission
Cardiology I
170 - Placental Vascular Malperfusion Lesions in Fetal Congenital Heart Disease
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 170
Rachel L. Leon, University of Texas Southwestern Medical School, Dallas, TX, United States; Kavita Sharma, University of Texas Southwestern Medical School, Dallas, TX, United States; Imran N. Mir, University of Texas Southwestern Medical School, Dallas, TX, United States; Lina Chalak, UT Southwestern, DALLAS, TX, United States

Rachel L. Leon, MD, PhD (she/her/hers)
Assistant Professor
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Fetuses with congenital heart disease (CHD) are at increased risk of perinatal morbidity and mortality, which is highly influenced by their prenatal health. Placental function is the key organ responsible for the health of the prenatal environment and is known to have high rates of pathologic lesions in pregnancies complicated by fetal CHD.
Objective: To determine the prevalence of both gross and histologic placental pathologies in a cohort of pregnancies complicated by CHD compared to healthy controls. Secondarily, we sought to determine the relative burden of placental pathologies in specific subgroups of CHD.
Design/Methods: This single center retrospective cohort study included placental examinations from pregnancies diagnosed prenatally with fetal CHD between 2010 and 2019, while Control placentas were collected from pregnancies without maternal or fetal complications. Placentas were sampled and evaluated according to the Amsterdam Placental Workshop Group Consensus Statement and gross and histopathologic diagnoses determined.
Results: Approximately 80% of fetuses diagnosed with CHD had placental examination (n=305) for comparison with healthy Controls (n=40). Gestational age was similar between groups and birthweight z-score did not differ between CHD and Controls. Birth head circumference was 1.5 cm less in CHD patients with a significantly lower z-score (-0.52 +/- 1.22 vs. 0.06 +/- 0.69; p< 0.01). A total of 78% of CHD placentas had gross or histologic pathology. One-third of CHD placentas met criteria for SGA and 48% had one or more chronic lesion(s) including maternal vascular malperfusion (MVM; 23% vs. 0%, p< 0.01), villitis of unknown etiology (VUE; 22% vs. 0%, p< 0.01), fetal vascular malperfusion (FVM; 20% vs. 0%, p< 0.01), and other chronic lesions (16% vs. 0%, p< 0.01). Acute inflammation was equally present in both CHD and Control groups (28% vs. 28%, p=1.00). In subgroup analyses, there was a non-significant increased rate of MVM lesions in those with single-ventricle with right-sided obstructive defects.Conclusion(s): Vascular malperfusion lesions and chronic forms of inflammation occur at significantly higher rates in the fetal CHD placenta, which may contribute to decreased head circumference at birth. Further work is needed to delineate the etiology of placental lesions in pregnancies complicated by fetal CHD and their impact on clinical outcomes.
Table 1. Maternal and Infant Patient Characteristics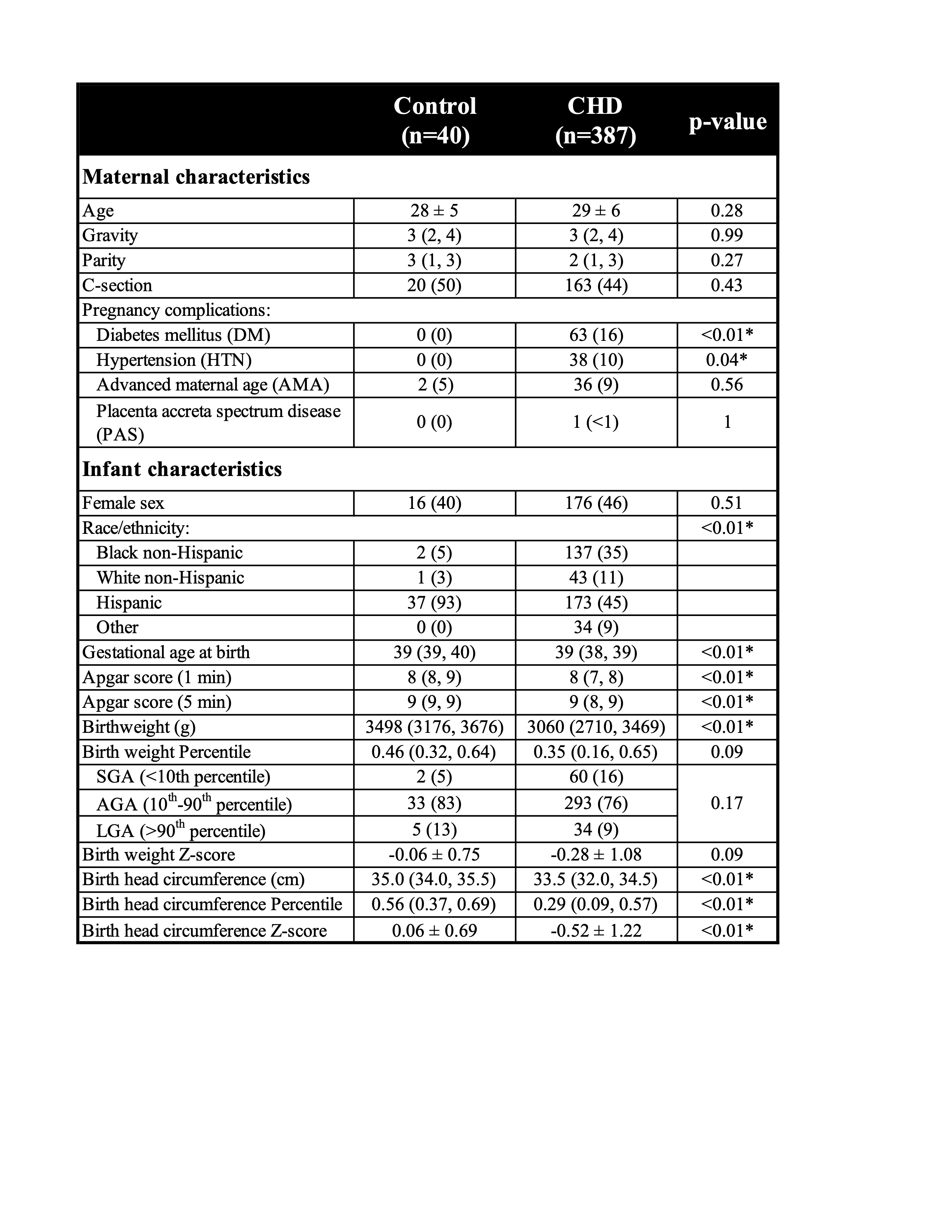 n (%) compared using Chi-square or Fisher Exact test; Mean ± standard deviation compared using T-test; Median (25th, 75th) compared using Mann-Whitney U-test; *indicates statistically significant result at p < 0.05
n (%) compared using Chi-square or Fisher Exact test; Mean ± standard deviation compared using T-test; Median (25th, 75th) compared using Mann-Whitney U-test; *indicates statistically significant result at p < 0.05
Table 2. Gross Placental Pathologies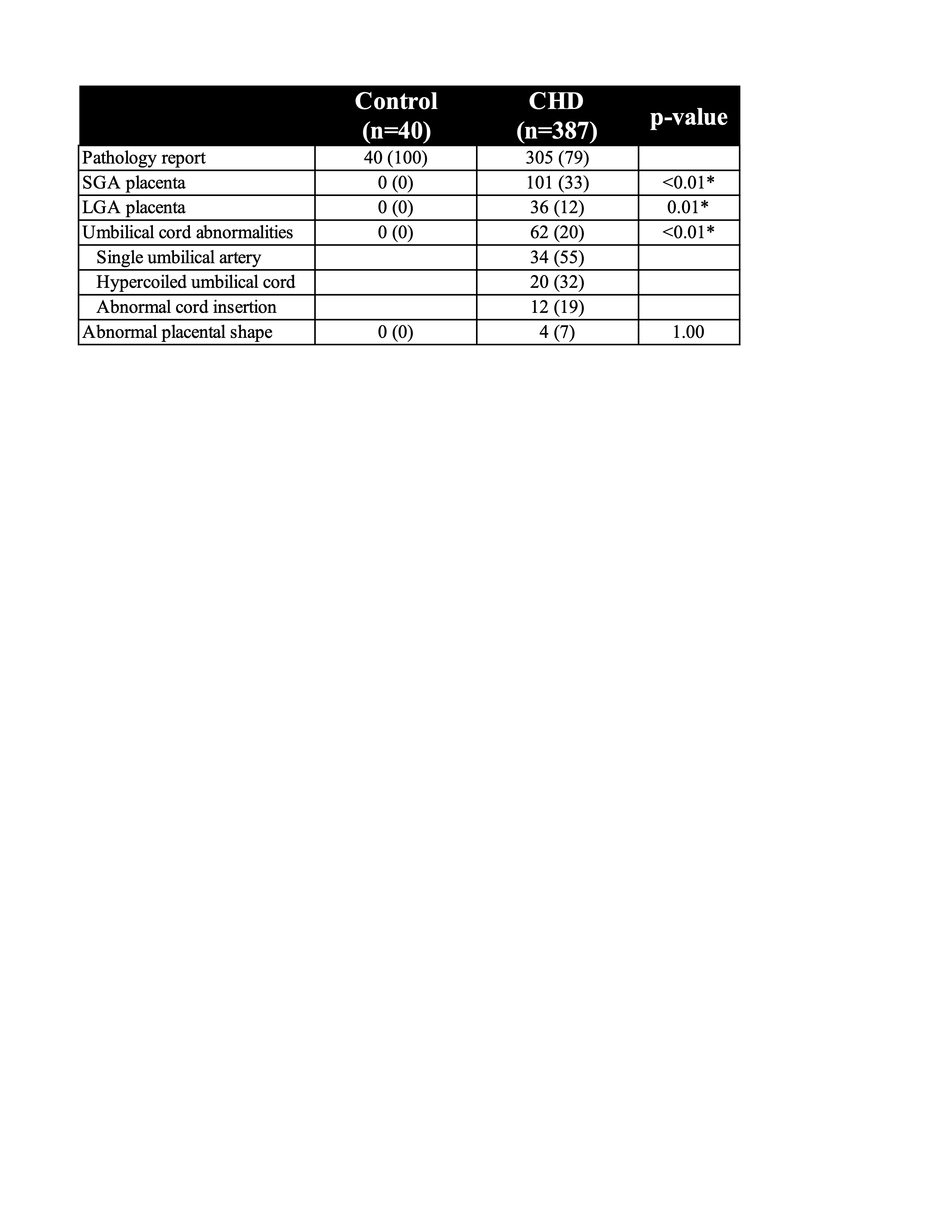 n (%) compared using Chi-square or Fisher Exact test; *indicates statistically significant result at p < 0.05
n (%) compared using Chi-square or Fisher Exact test; *indicates statistically significant result at p < 0.05
Objective: To determine the prevalence of both gross and histologic placental pathologies in a cohort of pregnancies complicated by CHD compared to healthy controls. Secondarily, we sought to determine the relative burden of placental pathologies in specific subgroups of CHD.
Design/Methods: This single center retrospective cohort study included placental examinations from pregnancies diagnosed prenatally with fetal CHD between 2010 and 2019, while Control placentas were collected from pregnancies without maternal or fetal complications. Placentas were sampled and evaluated according to the Amsterdam Placental Workshop Group Consensus Statement and gross and histopathologic diagnoses determined.
Results: Approximately 80% of fetuses diagnosed with CHD had placental examination (n=305) for comparison with healthy Controls (n=40). Gestational age was similar between groups and birthweight z-score did not differ between CHD and Controls. Birth head circumference was 1.5 cm less in CHD patients with a significantly lower z-score (-0.52 +/- 1.22 vs. 0.06 +/- 0.69; p< 0.01). A total of 78% of CHD placentas had gross or histologic pathology. One-third of CHD placentas met criteria for SGA and 48% had one or more chronic lesion(s) including maternal vascular malperfusion (MVM; 23% vs. 0%, p< 0.01), villitis of unknown etiology (VUE; 22% vs. 0%, p< 0.01), fetal vascular malperfusion (FVM; 20% vs. 0%, p< 0.01), and other chronic lesions (16% vs. 0%, p< 0.01). Acute inflammation was equally present in both CHD and Control groups (28% vs. 28%, p=1.00). In subgroup analyses, there was a non-significant increased rate of MVM lesions in those with single-ventricle with right-sided obstructive defects.Conclusion(s): Vascular malperfusion lesions and chronic forms of inflammation occur at significantly higher rates in the fetal CHD placenta, which may contribute to decreased head circumference at birth. Further work is needed to delineate the etiology of placental lesions in pregnancies complicated by fetal CHD and their impact on clinical outcomes.
Table 1. Maternal and Infant Patient Characteristics
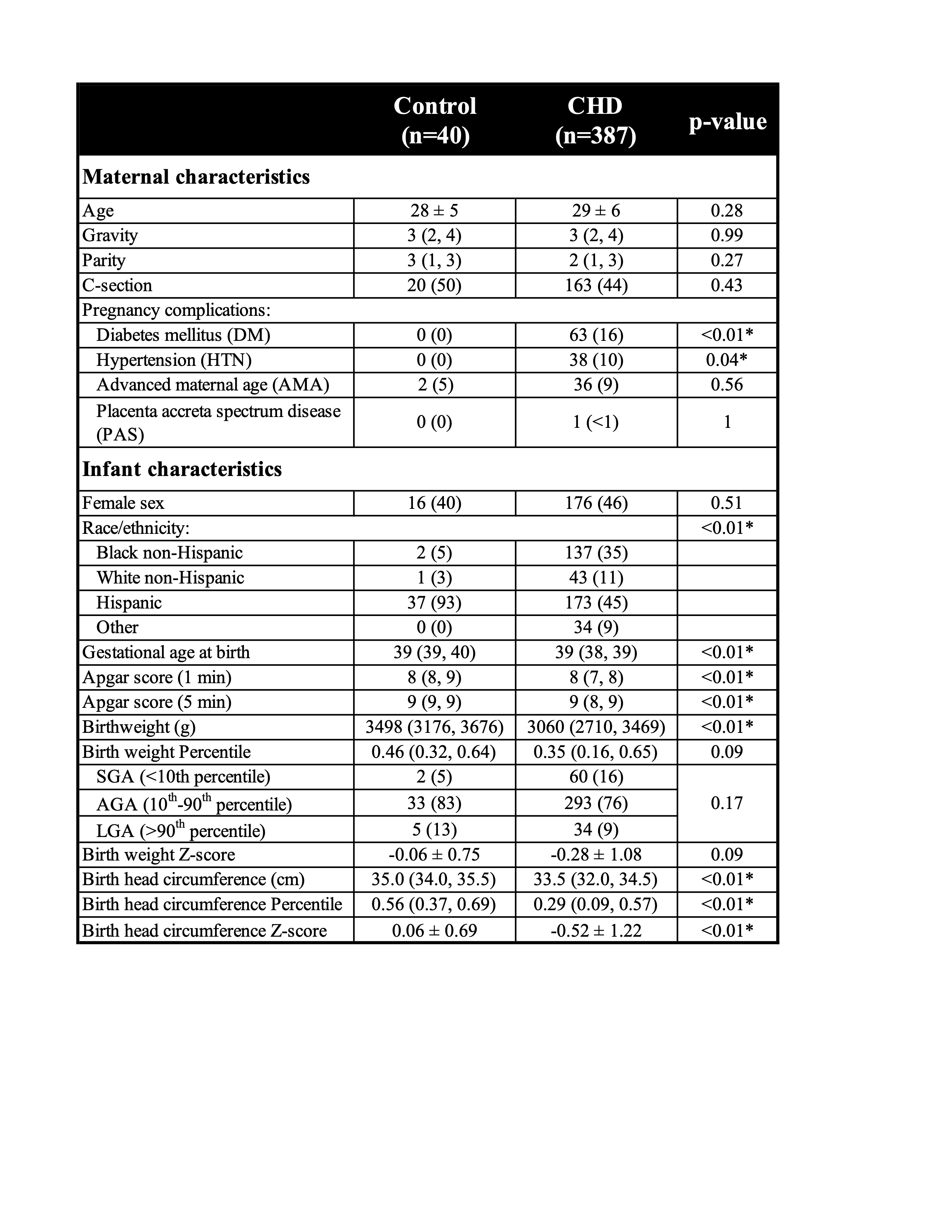 n (%) compared using Chi-square or Fisher Exact test; Mean ± standard deviation compared using T-test; Median (25th, 75th) compared using Mann-Whitney U-test; *indicates statistically significant result at p < 0.05
n (%) compared using Chi-square or Fisher Exact test; Mean ± standard deviation compared using T-test; Median (25th, 75th) compared using Mann-Whitney U-test; *indicates statistically significant result at p < 0.05Table 2. Gross Placental Pathologies
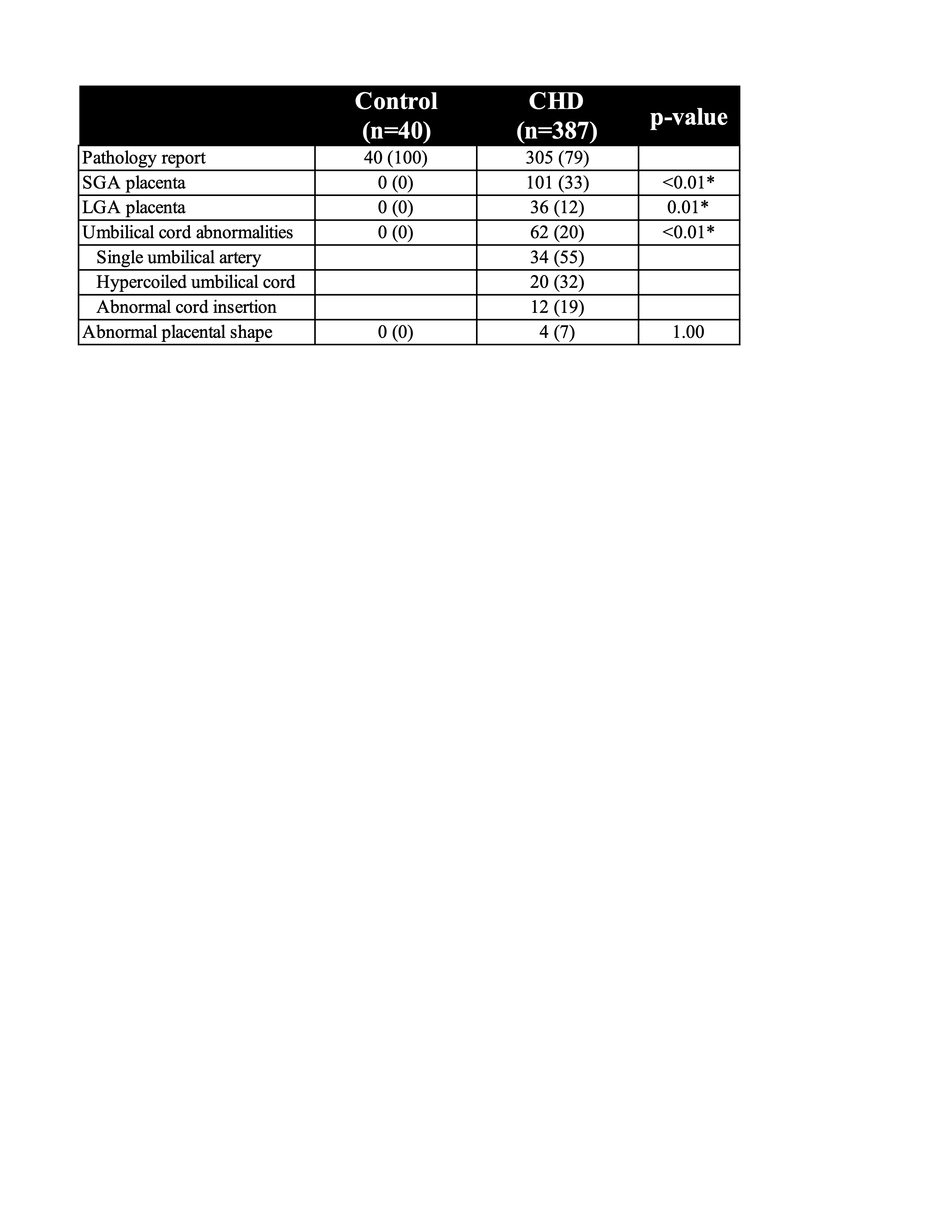 n (%) compared using Chi-square or Fisher Exact test; *indicates statistically significant result at p < 0.05
n (%) compared using Chi-square or Fisher Exact test; *indicates statistically significant result at p < 0.05