Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement II: Neurology and Infection
229 - Successful containment of a methicillin resistant staphylococcus aureus outbreak in the neonatal intensive care unit: Response to quality improvement measures
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 229
Publication Number: 229.127
Publication Number: 229.127
Abhijeet Namjoshi, Phoenix Children's Hospital, Phoenix, AZ, United States; Soumini Chintala, Phoenix Children's Hospital, Phoenix, AZ, United States; Zoe R. Coleman, Dignity Health - St. Joseph's Hospital and Medical Center, Phoenix, AZ, United States; Maria Cecilia K. Mercado, Nationwide Children's Hospital, Powell, OH, United States; Andrea Hassler, St. Joseph's Hospital and Medical Center, Phoenix, AZ, United States; Hemananda K. Muniraman, Phoenix Children's Hospital, PHOENIX, AZ, United States

Abhijeet S. Namjoshi, MD (he/him/his)
Pediatric Chief Resident
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: In September 2020, during the coronavirus disease 2019 (COVID-19) pandemic, our neonatal intensive care unit (NICU) experienced a methicillin resistant staphylococcus aureus (MRSA) outbreak affecting 4 infants (1 bacteremia, 2 tracheitis and 1 conjunctivitis). In response, a comprehensive quality improvement (QI) process involving a multidisciplinary team was established with goal of reducing MRSA colonization and infection rates in the NICU by 50% in 4 months. Key drivers and process changes were identified for reducing MRSA infection and transmission in the NICU by cohorting and decolonization of colonized infants and reducing transmission by improving hand hygiene, mask hygiene and disinfectant practices (Figures 1 and 2).
Objective: To reduce MRSA colonization and infection rates in the NICU by 50% in 4 months.
Design/Methods: Prospective collection of data on MRSA colonization and infection rates over period of 4-month QI process in a 65-bed tertiary level NICU.
Results: The QI process included over 5400 inpatient days involving 170 infants over a 4-month period between 1st October 2020 and 31st January 2021. Initial MRSA screening showed colonization rate of 16% (6/38). With cohorting and decolonization, the rate of colonization decreased to 5% (2/40) by week 3 and ranged between 0 and around 2% (1 infant) until week 13 (figure 3). No new colonization was reported from week 14 until week 18 after which routine screening was discontinued. One MRSA skin infection was reported on week 1 and no other infections occurred during the rest of the 4 month period. Post QI process, surveillance was continued for MRSA infections and no new infections were reported over the next 12 months.Conclusion(s): We report successful containment of MRSA outbreak with a comprehensive multi-disciplinary quality improvement process focusing on reducing MRSA colonization, infection, and transmission in the neonatal unit with reduction of colonization rates by 90% and no new cases of MRSA infection after the first week of MRSA reduction program for over 12 month period.
Figure 1.png) Key drivers and process changes identified to reduce MRSA colonization and infection
Key drivers and process changes identified to reduce MRSA colonization and infection
Figure 2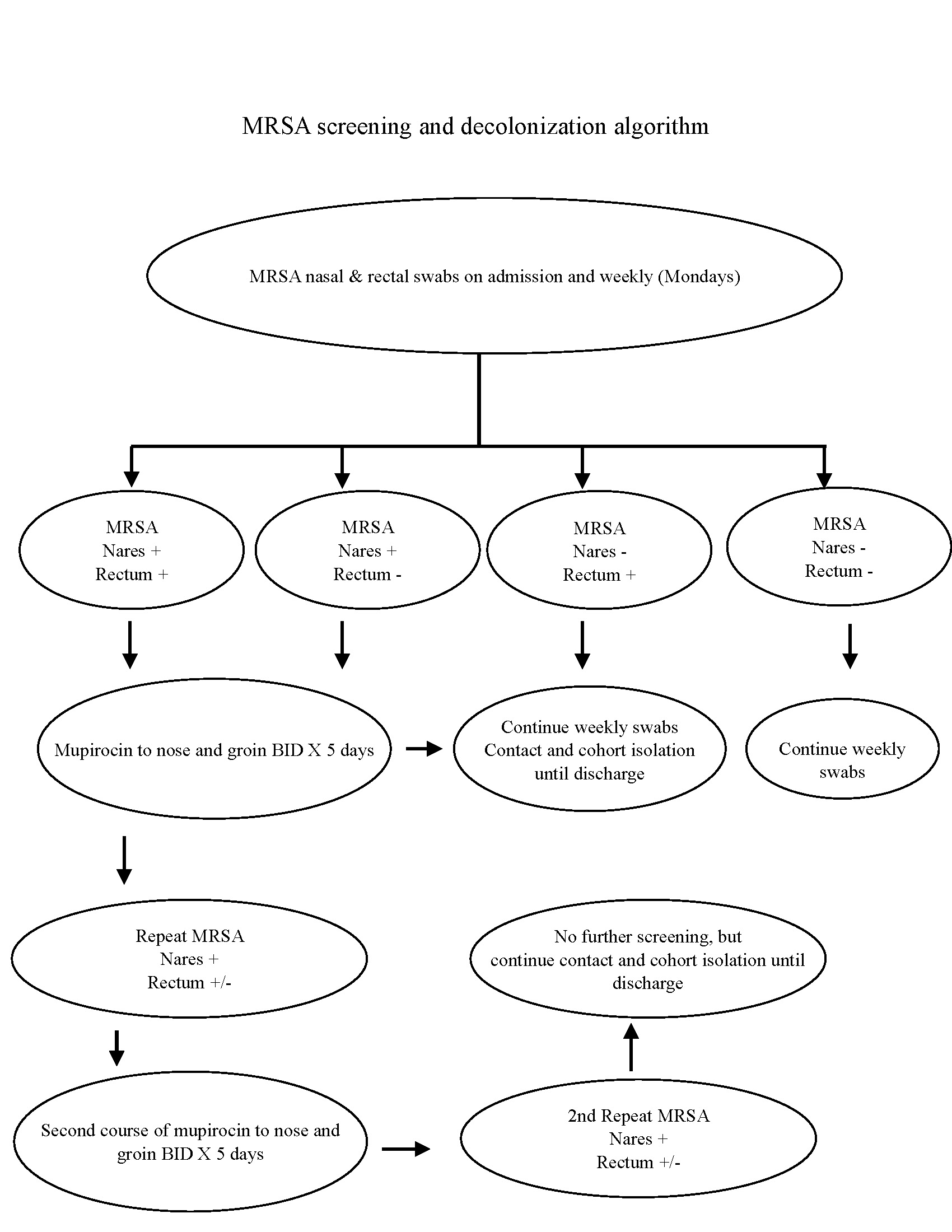 Algorithm for cohorting and decolonization of neonates with MRSA
Algorithm for cohorting and decolonization of neonates with MRSA
Objective: To reduce MRSA colonization and infection rates in the NICU by 50% in 4 months.
Design/Methods: Prospective collection of data on MRSA colonization and infection rates over period of 4-month QI process in a 65-bed tertiary level NICU.
Results: The QI process included over 5400 inpatient days involving 170 infants over a 4-month period between 1st October 2020 and 31st January 2021. Initial MRSA screening showed colonization rate of 16% (6/38). With cohorting and decolonization, the rate of colonization decreased to 5% (2/40) by week 3 and ranged between 0 and around 2% (1 infant) until week 13 (figure 3). No new colonization was reported from week 14 until week 18 after which routine screening was discontinued. One MRSA skin infection was reported on week 1 and no other infections occurred during the rest of the 4 month period. Post QI process, surveillance was continued for MRSA infections and no new infections were reported over the next 12 months.Conclusion(s): We report successful containment of MRSA outbreak with a comprehensive multi-disciplinary quality improvement process focusing on reducing MRSA colonization, infection, and transmission in the neonatal unit with reduction of colonization rates by 90% and no new cases of MRSA infection after the first week of MRSA reduction program for over 12 month period.
Figure 1
.png) Key drivers and process changes identified to reduce MRSA colonization and infection
Key drivers and process changes identified to reduce MRSA colonization and infectionFigure 2
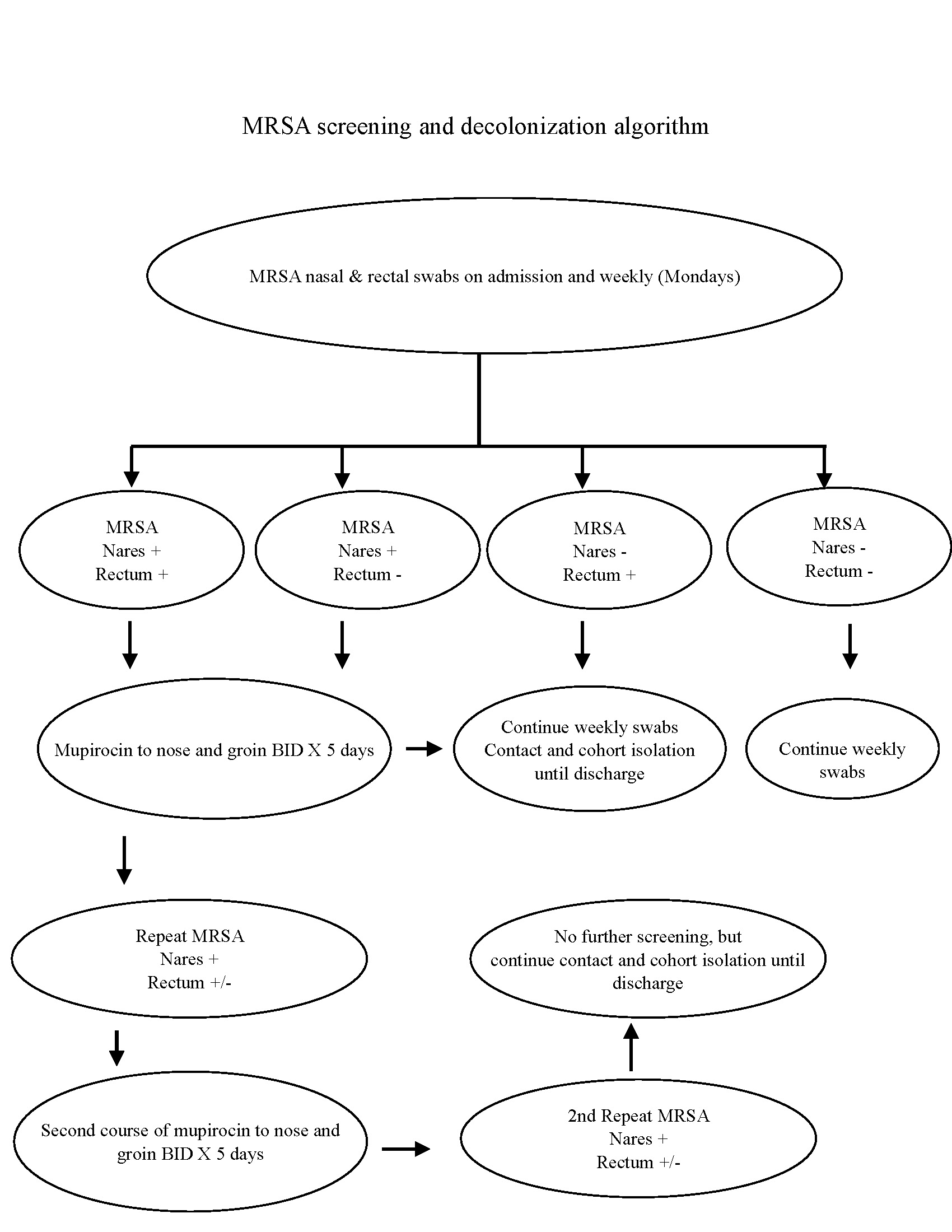 Algorithm for cohorting and decolonization of neonates with MRSA
Algorithm for cohorting and decolonization of neonates with MRSA