Neonatal General
Category: Abstract Submission
Neonatology General 4
399 - The Association of Placental Pathology and Lenticulostriate Vasculopathy (LSV) in Preterm Infants
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 399
Publication Number: 399.134
Publication Number: 399.134
Julide Sisman, University of Texas Southwestern Medical Center, DALLAS, TX, United States; Larry S. Brown, Parkland Health & Hospital System, Dallas, TX, United States; Imran N. Mir, University of Texas Southwestern Medical School, Dallas, TX, United States
- JS
Julide Sisman, MD
Associate Professor
University of Texas Southwestern Medical Center
The University of Texas Southwestern Medical Center
DALLAS, Texas, United States
Presenting Author(s)
Background: Studies aimed to study relationship between LSV and chorioamnionitis have failed to demonstrate an association. To date, there are no reports evaluated the frequency and the type of placental abnormalities in neonates with LSV using a standardized placental pathology classification.
Objective: To examine the frequency and the type of placental abnormalities in neonates with LSV.
Design/Methods: We prospectively reviewed 1351 cranial ultrasound scans (cUS) from 407 neonates ≤ 32 weeks of gestation for the presence of LSV at Parkland Hospital Dallas, TX between 2012 and 2014. LSV was diagnosed in 65 neonates. Matched controls (n=70) with normal cUS at discharge were enrolled to the study. A new classification system describing the progression of LSV is developed and validated as followed; 0= no vessels seen 1=lenticulostriate vessels thin and faintly seen, 2= vessels still thin but moderately echogenic, 3= vessels thick and hyperechogenic (i.e., echogenicity similar to Sylvian fissure). We then retrieved placental pathology reports retrospectively and evaluated for placental abnormalities using Amsterdam Placental Workshop Group Consensus Statement. Associations between LSV stages and placental abnormalities were examined using χ2 or Fisher exact test. A 2-tailed significance level of P
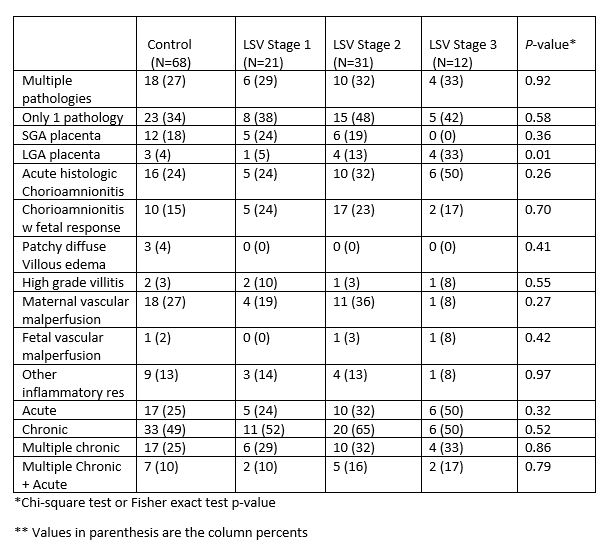
Results: Complete placental pathologic evaluations were available for 64/65 (98%) neonates with LSV and 68/70 (97%) for matched controls. A placental abnormality was detected in 49/64 (77%) in neonates with LSV, and 43/68 (63%) in matched controls (P=0.38). There were no significant differences for any type of placental abnormities between LSV and control groups, but when we examined the association using LSV classification; those infants with Stage 3 LSV were more likely to have large for gestational age (LGA) placentas (P=0.01).Conclusion(s): Placental weight < 10% or >90% for gestational age may be caused by placental malperfusion thus leading to chronic hypoxia in placenta and potentially in the fetus. Therefore, the association between progressive LSV and LGA placenta may suggest that intrauterine chronic hypoxia could be playing a role in etiology and progression of LSV.
Frequency and type of placental abnormalities in preterm infants with LSV and matched controls.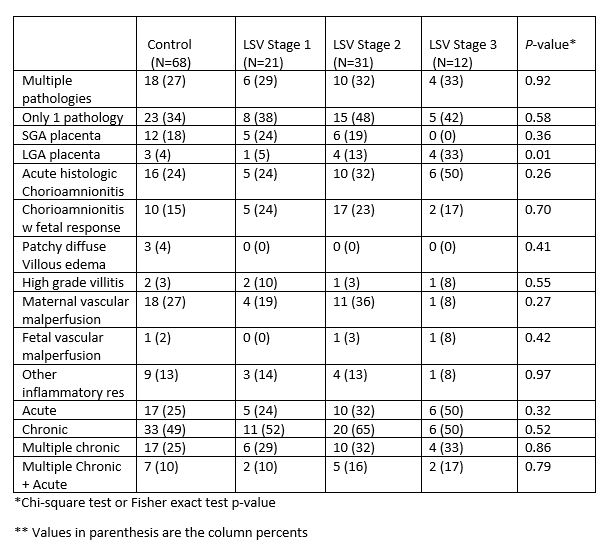
Objective: To examine the frequency and the type of placental abnormalities in neonates with LSV.
Design/Methods: We prospectively reviewed 1351 cranial ultrasound scans (cUS) from 407 neonates ≤ 32 weeks of gestation for the presence of LSV at Parkland Hospital Dallas, TX between 2012 and 2014. LSV was diagnosed in 65 neonates. Matched controls (n=70) with normal cUS at discharge were enrolled to the study. A new classification system describing the progression of LSV is developed and validated as followed; 0= no vessels seen 1=lenticulostriate vessels thin and faintly seen, 2= vessels still thin but moderately echogenic, 3= vessels thick and hyperechogenic (i.e., echogenicity similar to Sylvian fissure). We then retrieved placental pathology reports retrospectively and evaluated for placental abnormalities using Amsterdam Placental Workshop Group Consensus Statement. Associations between LSV stages and placental abnormalities were examined using χ2 or Fisher exact test. A 2-tailed significance level of P
Results: Complete placental pathologic evaluations were available for 64/65 (98%) neonates with LSV and 68/70 (97%) for matched controls. A placental abnormality was detected in 49/64 (77%) in neonates with LSV, and 43/68 (63%) in matched controls (P=0.38). There were no significant differences for any type of placental abnormities between LSV and control groups, but when we examined the association using LSV classification; those infants with Stage 3 LSV were more likely to have large for gestational age (LGA) placentas (P=0.01).Conclusion(s): Placental weight < 10% or >90% for gestational age may be caused by placental malperfusion thus leading to chronic hypoxia in placenta and potentially in the fetus. Therefore, the association between progressive LSV and LGA placenta may suggest that intrauterine chronic hypoxia could be playing a role in etiology and progression of LSV.
Frequency and type of placental abnormalities in preterm infants with LSV and matched controls.