Emergency Medicine: All Areas
Category: Abstract Submission
4: Emergency Medicine I
47 - The pediatric mental health crisis: an increasing challenge for prehospital care providers
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 47
Publication Number: 47.103
Publication Number: 47.103
Victoria Hartwell, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Lauren C. Riney, Pediatric Emergency Medicine, Cincinnati, OH, United States; Alexandra Cheetham, Children's Cincinnati, Cincinnati, OH, United States; Rachel Bensman, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Sang Hoon Lee, University of Cincinnati College of Medicine, Cincinnati, OH, United States; Lynn Babcock, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Wendy Pomerantz, Cincinnati Children's Hospital, Cincinnati, OH, United States

Victoria Hartwell, MD
Clinical Fellow, Division of Emergency Medicine
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Pediatric mental health (MH) emergencies are increasing, with pediatric emergency departments (PEDs) seeing increases in MH patient volumes compared to all PED visit types over recent years. Many arrive via Emergency Medical Services (EMS), however little is known regarding the burden of pediatric MH calls on the EMS system.
Objective: To compare the epidemiology, trends in utilization, and ED outcomes of pediatric patients with acute MH complaints to those with non-MH complaints transported to two PEDs by EMS.
Design/Methods: This was a retrospective cohort study of patients aged 5 to 18 years who were transported via EMS to two PEDs affiliated with a large children’s hospital from 1 January 2012 to 31 December 2020. Data was abstracted from electronic hospital records. Descriptive statistics were used to compare children transported by EMS to the PED with MH complaints to those with non-MH complaints. MH was defined by a combination of diagnostic codes and chief complaints. We also evaluated trends in EMS transports over time comparing numbers of MH patients to those with non-MH complaints.
Results: During the 9-year study period, 36,534 patients were transported to the PED by EMS; 10,264 (28.1%) of these patients had MH complaints. The proportion of patients who were transported by EMS for MH visits increased by 57.9% over the study period compared to all patients transported by EMS (Figure). As shown in the table, MH patients transported by EMS were more likely (all p < 0.01) to be older (13.6 vs 11.4 years), female (52.7 vs 45.5%), white (62.2 vs 55.2%), have public health insurance (63.1% vs 55.8%), require mechanical or physical restraints in PED (6.6 vs 0.1%), and require chemical restraint medications (e.g. antipsychotics/benzodiazepines) in PED (8.7 vs 4.6%); and less likely to be Hispanic (3.5 vs 4.1%). MH patients also had higher rates of hospital admission (54.0 vs 20.4%).Conclusion(s): For EMS, the proportion of children transported for an acute MH emergency is sizeable and increasing substantially. Children transported by EMS with acute MH emergencies represent a demographically distinct and more agitated EMS population. These data emphasizes the urgent need for distinct EMS guidance to care for children with mental health emergencies.
Figure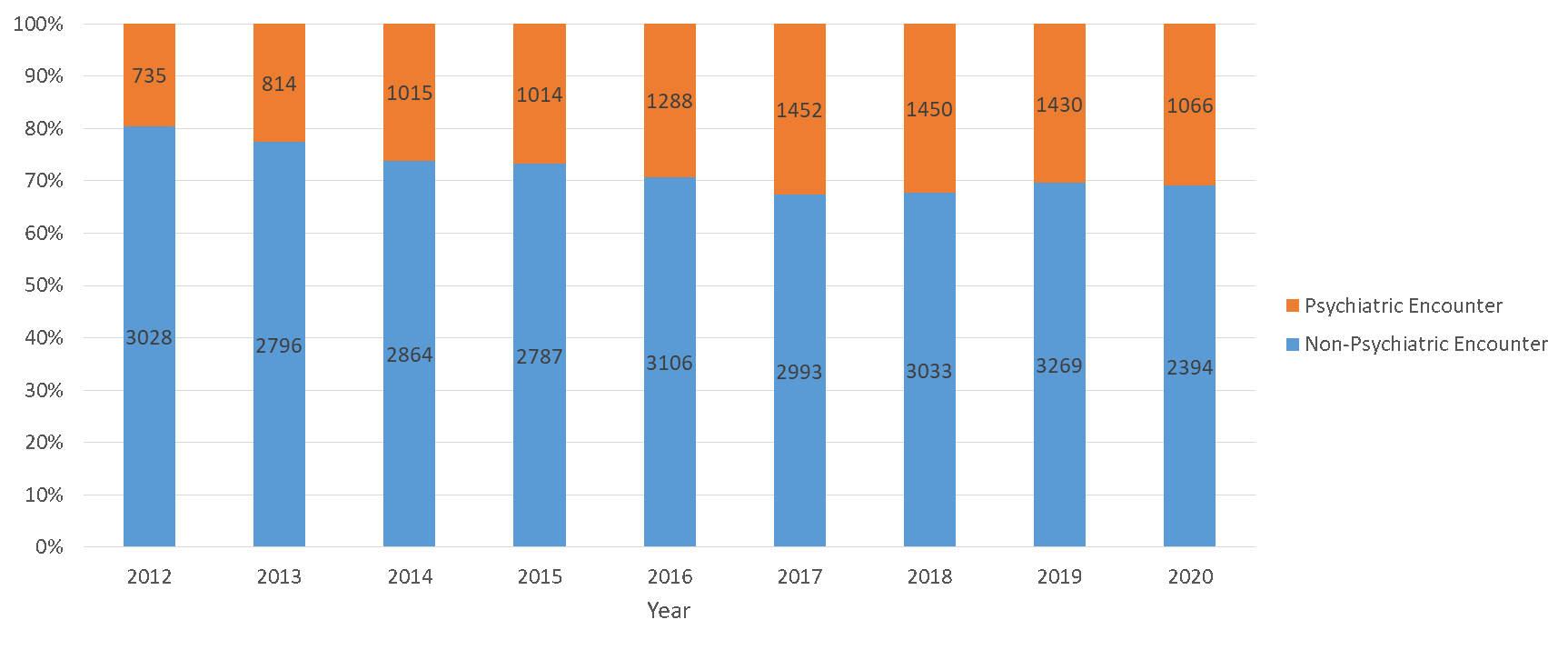 Proportion of patients transported by EMS for mental health visits by year
Proportion of patients transported by EMS for mental health visits by year
Table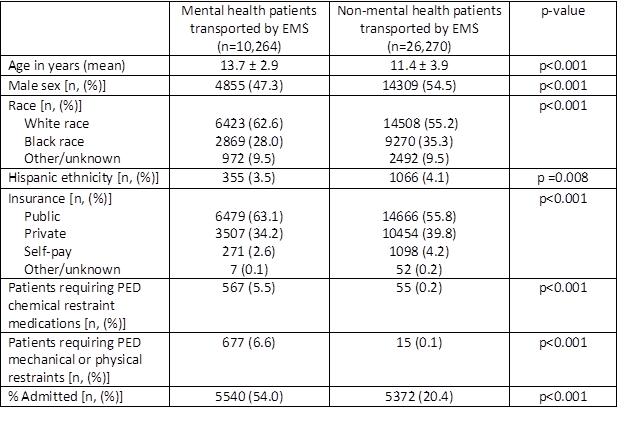 Demographics of mental health patients transported by EMS compared to non-mental health patients
Demographics of mental health patients transported by EMS compared to non-mental health patients
Objective: To compare the epidemiology, trends in utilization, and ED outcomes of pediatric patients with acute MH complaints to those with non-MH complaints transported to two PEDs by EMS.
Design/Methods: This was a retrospective cohort study of patients aged 5 to 18 years who were transported via EMS to two PEDs affiliated with a large children’s hospital from 1 January 2012 to 31 December 2020. Data was abstracted from electronic hospital records. Descriptive statistics were used to compare children transported by EMS to the PED with MH complaints to those with non-MH complaints. MH was defined by a combination of diagnostic codes and chief complaints. We also evaluated trends in EMS transports over time comparing numbers of MH patients to those with non-MH complaints.
Results: During the 9-year study period, 36,534 patients were transported to the PED by EMS; 10,264 (28.1%) of these patients had MH complaints. The proportion of patients who were transported by EMS for MH visits increased by 57.9% over the study period compared to all patients transported by EMS (Figure). As shown in the table, MH patients transported by EMS were more likely (all p < 0.01) to be older (13.6 vs 11.4 years), female (52.7 vs 45.5%), white (62.2 vs 55.2%), have public health insurance (63.1% vs 55.8%), require mechanical or physical restraints in PED (6.6 vs 0.1%), and require chemical restraint medications (e.g. antipsychotics/benzodiazepines) in PED (8.7 vs 4.6%); and less likely to be Hispanic (3.5 vs 4.1%). MH patients also had higher rates of hospital admission (54.0 vs 20.4%).Conclusion(s): For EMS, the proportion of children transported for an acute MH emergency is sizeable and increasing substantially. Children transported by EMS with acute MH emergencies represent a demographically distinct and more agitated EMS population. These data emphasizes the urgent need for distinct EMS guidance to care for children with mental health emergencies.
Figure
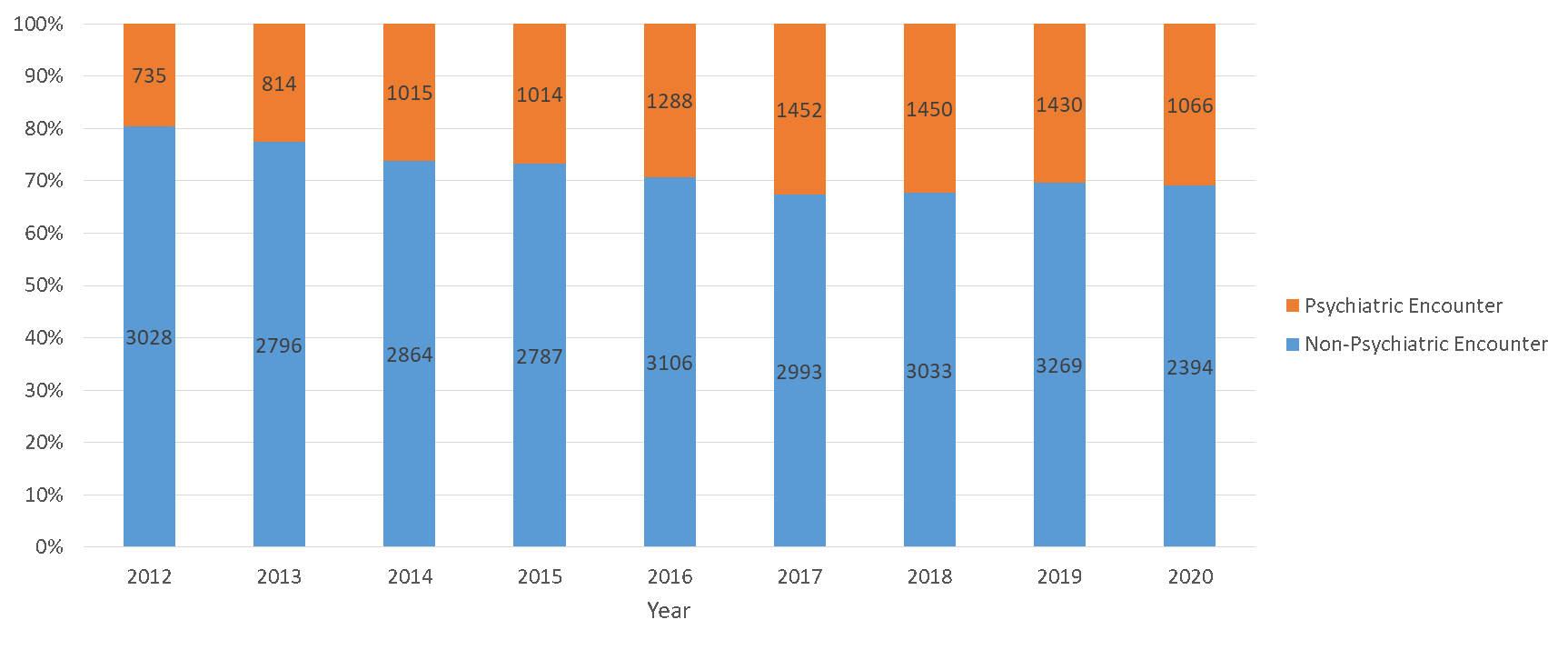 Proportion of patients transported by EMS for mental health visits by year
Proportion of patients transported by EMS for mental health visits by yearTable
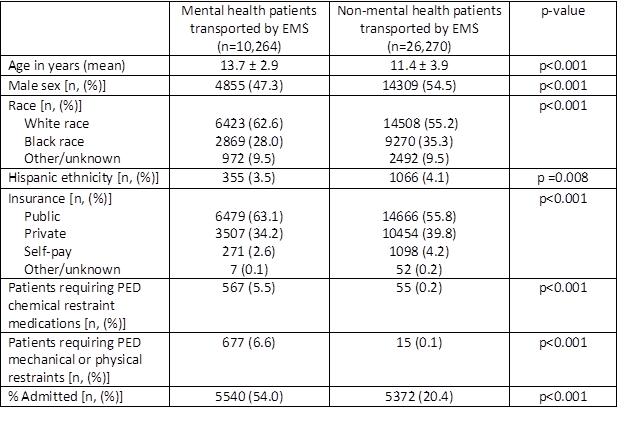 Demographics of mental health patients transported by EMS compared to non-mental health patients
Demographics of mental health patients transported by EMS compared to non-mental health patients