Nephrology: Basic
Category: Abstract Submission
Nephrology I: Potpourri
102 - The Prevalence and Outcomes of Hyponatremia in Children with COVID-19 and Multisystem Inflammatory Syndrome in Children (MIS-C)
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 102
Publication Number: 102.138
Publication Number: 102.138
Neal P. Dalal, Cohen Children's Medical Center, Princeton, NJ, United States; Mairead R. Pfaff, Cohen Children's Medical Center, Garden City, NY, United States; Layne Silver, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, New Hyde Park, NY, United States; Christine Sethna, Cohen Children's Medical Center, New Hyde Park, NY, United States; Pamela Singer, Long Island Jewish Medical Center, New Hyde Park, NY, United States; Laura Castellanos Reyes, Cohen Children's Medical Center, New Hyde Park, NY, United States; Lily B. Glater, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, New Hyde Park, NY, United States; Abby Basalely, Cohen Children's Medical Center, New Hyde Park, NY, United States

Mairead R. Pfaff, BS
Research Coordinator
Cohen Children's Medical Center
Garden City, New York, United States
Presenting Author(s)
Background: Hyponatremia is an independent risk factor for morbidity and mortality in critically ill adults and children. Adults with COVID-19 often present with hyponatremia, and low serum sodium is associated with mortality. Pediatric data on hyponatremia in critically ill patients is limited.
Objective: We hypothesized that admission hyponatremia would be prevalent in pediatric patients with COVID-19 or MIS-C, and that these patients would have increased: (1) length of stay (LOS), (2) mechanical ventilation rates and (3) admission inflammatory markers.
Design/Methods: A retrospective analysis of patients ages 0-18 years, admitted March 1, 2020 – February 28, 2021 to the Northwell Health System with COVID-19 or MIS-C was performed. Hyponatremia was defined as a serum sodium < 135 meq/L. A Student’s t-test or Mann-Whitney U test was used to compare continuous variables while a Pearson’s chi2 test or Fisher’s exact test was used to compare categorical variables. Linear and logistic regression models were utilized to evaluate the association of hyponatremia with outcomes.
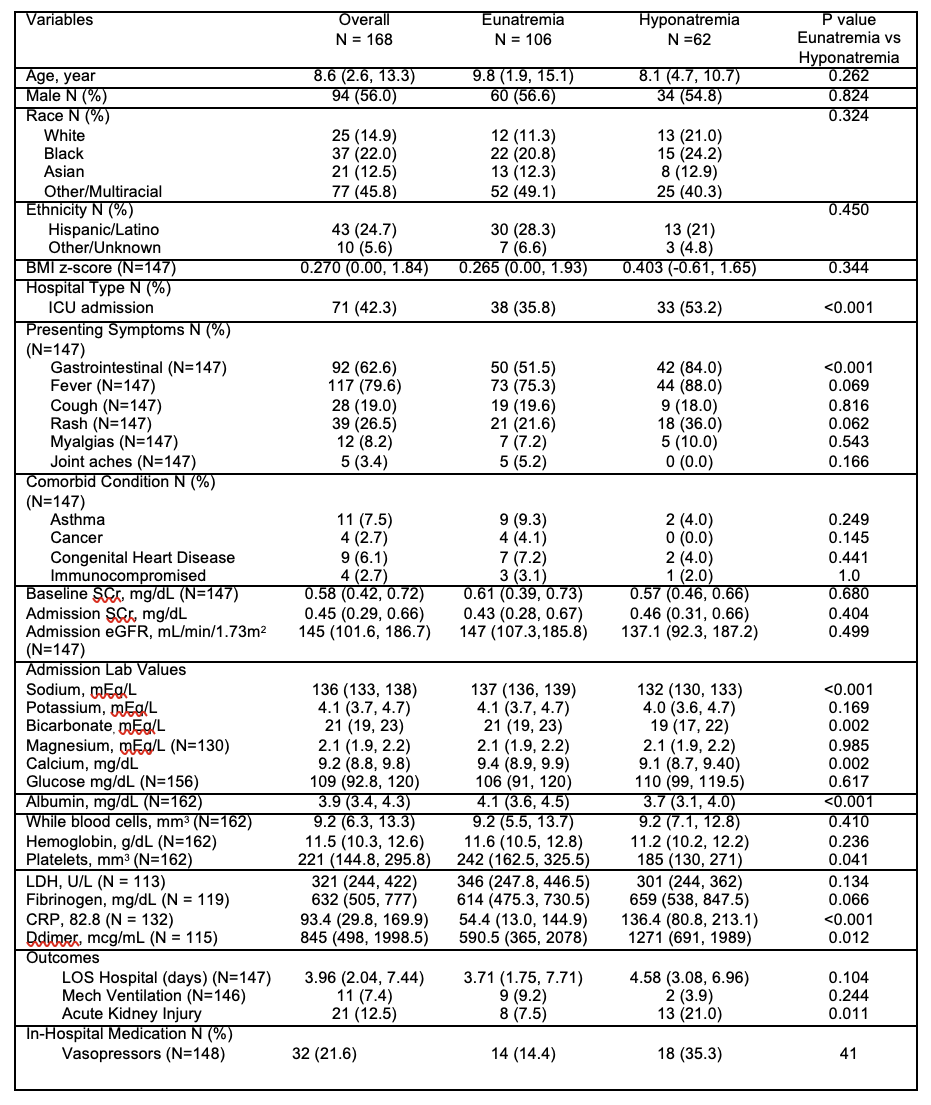
Results: Of the 168 children in the cohort, 95 (56%) had COVID-19 and 73 (43.5%) had MIS-C. Overall, 62 (36.9%) patients presented with hyponatremia. Patients with hyponatremia (33/62, 53.2%) were more likely to be admitted to the intensive care unit (ICU) when compared to eunatremic patients (38/106, 35.8%), p < 0.001. There were no differences between presenting symptoms or comorbid conditions between these populations. In regression models, hyponatremia was not significantly associated with increased LOS or need for mechanical ventilation. At time of admission, hyponatremic patients had lower bicarbonate levels (p=0.002), elevated CRP levels (p < 0.001), and lower albumin levels (p < 0.001) as compared to eunatremic patients (Table 1). Interestingly, after adjustment for confounders, hyponatremia remained associated with an increased square root CRP (β=2.68: 95% CI 1.1-4.2) and a lower albumin (β=-0.5: 95% CI -0.6-0.9), as compared to those with eunatremia. Conclusion(s): This study is, to our knowledge, the first to look at hyponatremia in COVID-19 and MIS-C in a pediatric population. While hyponatremia was common in the cohort, contrary to our hypothesis, it was not associated with greater LOS or need for mechanical ventilation. Of note, hyponatremic children had lower albumin levels and higher CRP levels than their eunatremic counterparts, suggesting that hyponatremia may reflect a state of increased inflammation.
Comparison of eunatremic patient population to hyponatremic patient population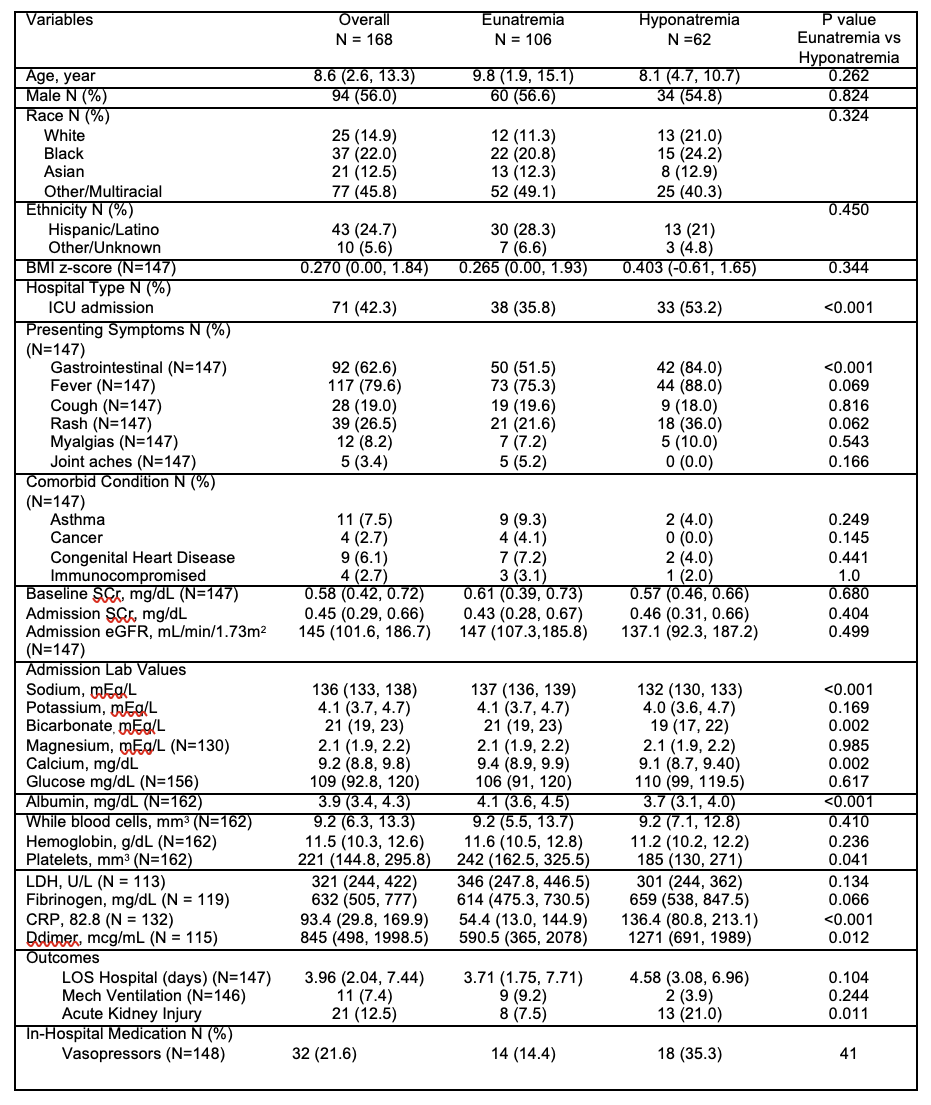
Objective: We hypothesized that admission hyponatremia would be prevalent in pediatric patients with COVID-19 or MIS-C, and that these patients would have increased: (1) length of stay (LOS), (2) mechanical ventilation rates and (3) admission inflammatory markers.
Design/Methods: A retrospective analysis of patients ages 0-18 years, admitted March 1, 2020 – February 28, 2021 to the Northwell Health System with COVID-19 or MIS-C was performed. Hyponatremia was defined as a serum sodium < 135 meq/L. A Student’s t-test or Mann-Whitney U test was used to compare continuous variables while a Pearson’s chi2 test or Fisher’s exact test was used to compare categorical variables. Linear and logistic regression models were utilized to evaluate the association of hyponatremia with outcomes.
Results: Of the 168 children in the cohort, 95 (56%) had COVID-19 and 73 (43.5%) had MIS-C. Overall, 62 (36.9%) patients presented with hyponatremia. Patients with hyponatremia (33/62, 53.2%) were more likely to be admitted to the intensive care unit (ICU) when compared to eunatremic patients (38/106, 35.8%), p < 0.001. There were no differences between presenting symptoms or comorbid conditions between these populations. In regression models, hyponatremia was not significantly associated with increased LOS or need for mechanical ventilation. At time of admission, hyponatremic patients had lower bicarbonate levels (p=0.002), elevated CRP levels (p < 0.001), and lower albumin levels (p < 0.001) as compared to eunatremic patients (Table 1). Interestingly, after adjustment for confounders, hyponatremia remained associated with an increased square root CRP (β=2.68: 95% CI 1.1-4.2) and a lower albumin (β=-0.5: 95% CI -0.6-0.9), as compared to those with eunatremia. Conclusion(s): This study is, to our knowledge, the first to look at hyponatremia in COVID-19 and MIS-C in a pediatric population. While hyponatremia was common in the cohort, contrary to our hypothesis, it was not associated with greater LOS or need for mechanical ventilation. Of note, hyponatremic children had lower albumin levels and higher CRP levels than their eunatremic counterparts, suggesting that hyponatremia may reflect a state of increased inflammation.
Comparison of eunatremic patient population to hyponatremic patient population