Cardiology
Category: Abstract Submission
Cardiology I
174 - The relationship between placental pathology and neurodevelopment outcomes in patients with complex congenital heart disease
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 174
Publication Number: 174.101
Publication Number: 174.101
David E. Segar, Medical College of Wisconsin, Milwaukee, WI, United States; Susan Cohen, Medical College of Wisconsin, Milwaukee, WI, United States; Jian Zhang, Medical College of Wisconsin, Milwaukee, WI, United States; Ke Yan, Medical College of Wisconsin, Milwaukee, WI, United States
David E. Segar, MD
Pediatric Cardiology Fellow
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Complex congenital heart disease (CCHD) is associated with impaired neurodevelopmental outcomes (NDO). Peri- and post-operative factors are known contributors while the impact of fetal hemodynamics is not yet well delineated. Impaired fetal circulation, seen in transposition of the great arteries (TGA) and univentricular physiology, is associated with placental abnormalities. These abnormalities in turn may be associated with placental insufficiency, a known risk factor for poor NDO.
Objective: We hypothesized there is a correlation between placental pathology and impaired NDO in patients with CCHD.
Design/Methods: We performed a single center retrospective cohort study with CCHD patients born from April 2005 to May 2018 at Children’s Wisconsin. Patient variables including sex, gestational age, weight, cardiac lesion, cardiopulmonary bypass time, and need for ECMO were obtained from the medical record. Bayley Scales of Infant Development Third Edition (Bayley-III) standard scores for cognitive, motor, and language performance were collected from neurodevelopmental follow-up visit documentation. Placenta pathology reports were reviewed with tabulation of pathological characteristics. To compare demographic and clinical information between infants with and without abnormal placentas the Chi-square test or Fisher’s exact test was used for categorical variables; the Mann-Whiney test was used for continuous variables. We used linear mixed models with unstructured covariance structure to model Bayley-III scores over time between placenta groups. P-valve < 0.05 was considered statistically significant.
Results: We identified 79 patients in our cohort and 61 (77.2%) had abnormal placentas based on the identification of fibrin, villous hypoplasia, chorangiosis, infarct, or any other placenta pathological abnormality. There was no significant difference between the two groups in any demographic and clinical variables (Table 1). For cognitive performance infants with placental abnormalities had significantly lower scores compared to infants without (Figure 1, p=0.026). Similarly, for motor performance, infants with placental abnormalities had significantly lower scores compared to infants without (p=0.045). There was no significant difference in language scores (p=0.12).Conclusion(s): Placental abnormalities are common in patients with CCHD. Our study has shown that placental abnormalities are significantly associated with impaired NDO. These results underscore the complex causal pathways of neurodevelopmental impairment in infants with CCHD, offering opportunities for targeted developmental interventions.
Table 1.png) Description of Study Cohort
Description of Study Cohort
Figure 1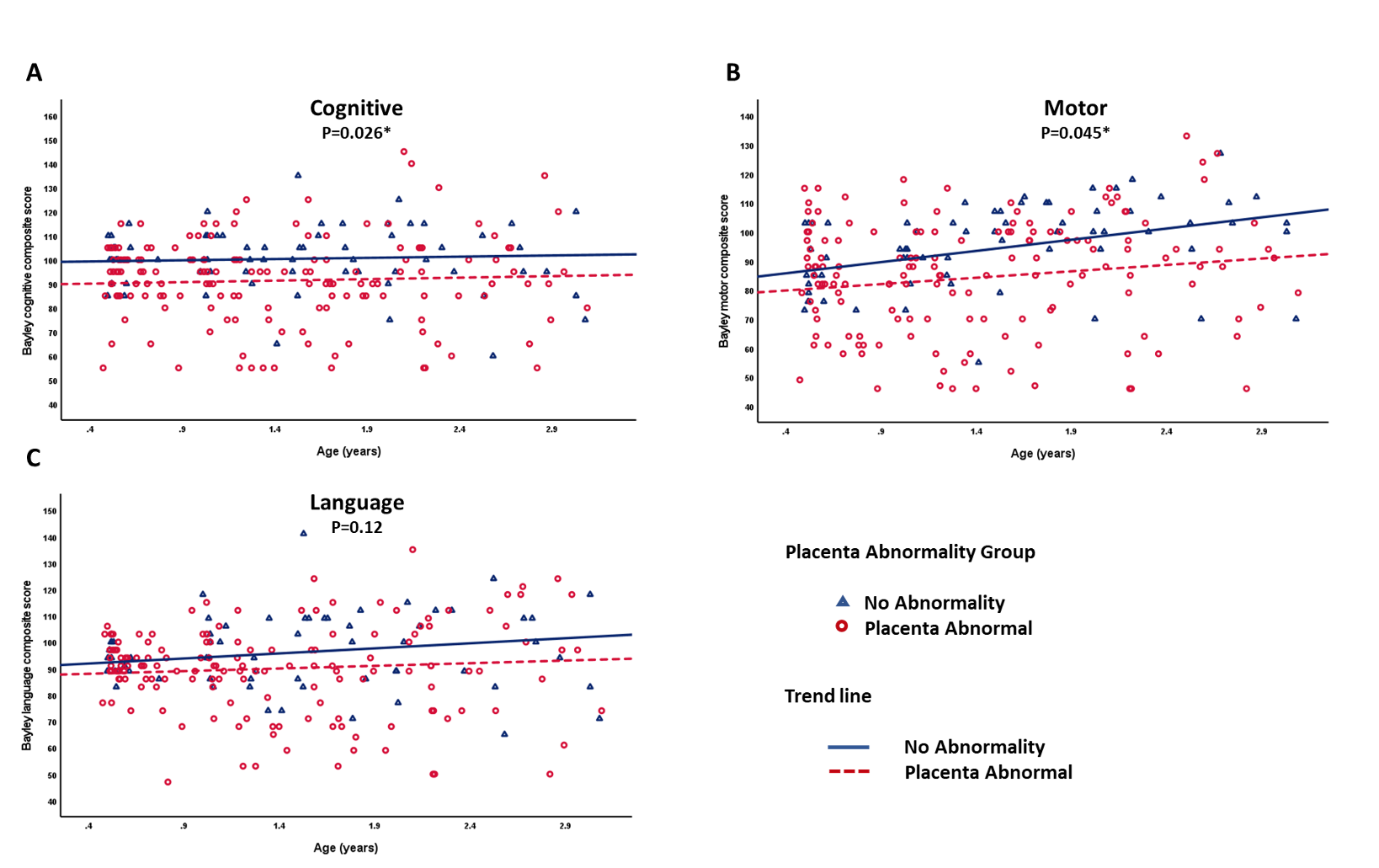 Bayley subscale scores of infants with and without placental abnormalities over time
Bayley subscale scores of infants with and without placental abnormalities over time
Objective: We hypothesized there is a correlation between placental pathology and impaired NDO in patients with CCHD.
Design/Methods: We performed a single center retrospective cohort study with CCHD patients born from April 2005 to May 2018 at Children’s Wisconsin. Patient variables including sex, gestational age, weight, cardiac lesion, cardiopulmonary bypass time, and need for ECMO were obtained from the medical record. Bayley Scales of Infant Development Third Edition (Bayley-III) standard scores for cognitive, motor, and language performance were collected from neurodevelopmental follow-up visit documentation. Placenta pathology reports were reviewed with tabulation of pathological characteristics. To compare demographic and clinical information between infants with and without abnormal placentas the Chi-square test or Fisher’s exact test was used for categorical variables; the Mann-Whiney test was used for continuous variables. We used linear mixed models with unstructured covariance structure to model Bayley-III scores over time between placenta groups. P-valve < 0.05 was considered statistically significant.
Results: We identified 79 patients in our cohort and 61 (77.2%) had abnormal placentas based on the identification of fibrin, villous hypoplasia, chorangiosis, infarct, or any other placenta pathological abnormality. There was no significant difference between the two groups in any demographic and clinical variables (Table 1). For cognitive performance infants with placental abnormalities had significantly lower scores compared to infants without (Figure 1, p=0.026). Similarly, for motor performance, infants with placental abnormalities had significantly lower scores compared to infants without (p=0.045). There was no significant difference in language scores (p=0.12).Conclusion(s): Placental abnormalities are common in patients with CCHD. Our study has shown that placental abnormalities are significantly associated with impaired NDO. These results underscore the complex causal pathways of neurodevelopmental impairment in infants with CCHD, offering opportunities for targeted developmental interventions.
Table 1
.png) Description of Study Cohort
Description of Study CohortFigure 1
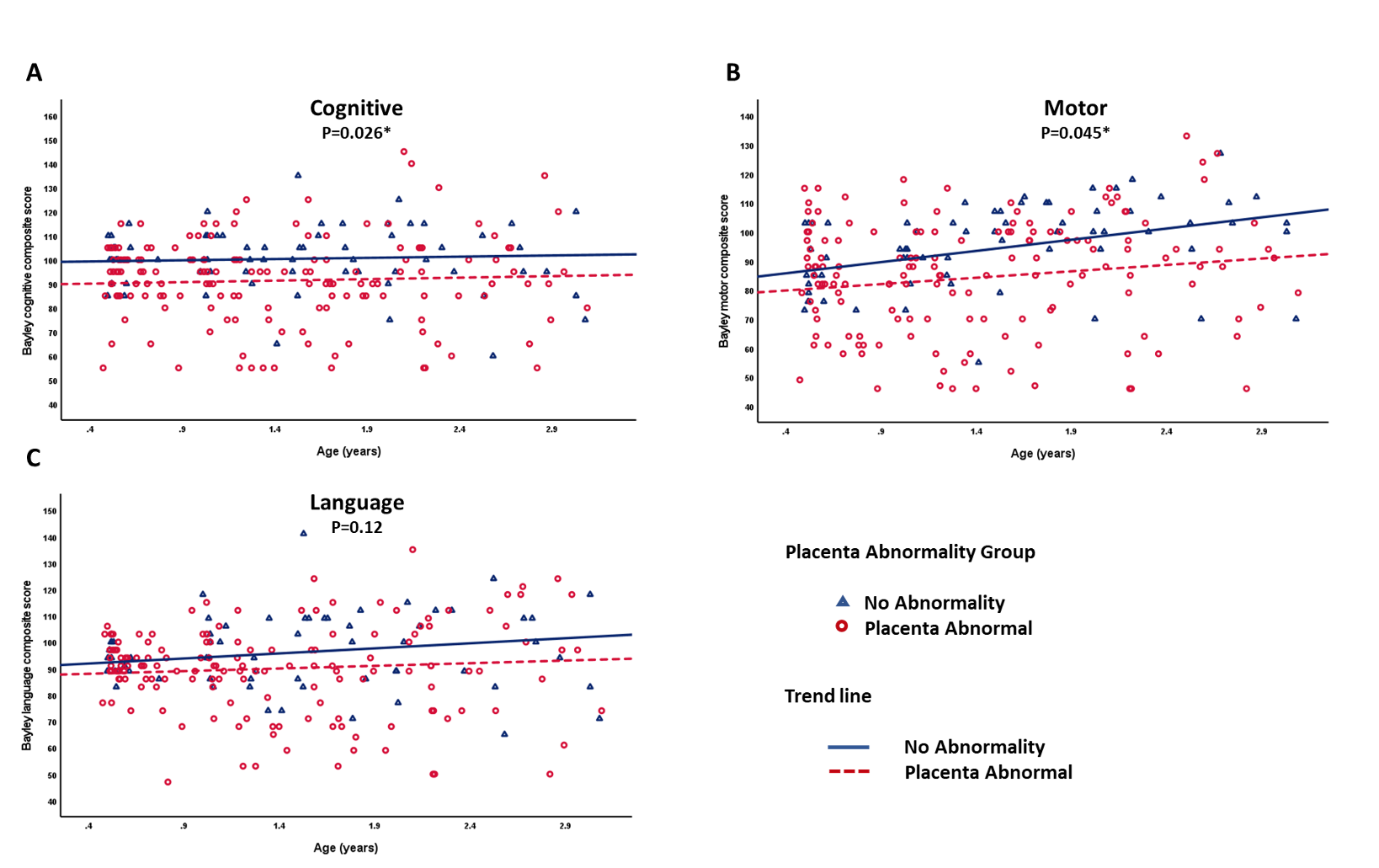 Bayley subscale scores of infants with and without placental abnormalities over time
Bayley subscale scores of infants with and without placental abnormalities over time