Neonatal General
Category: Abstract Submission
Neonatology General 3
382 - The Value of DNR Orders in the NICU: The Medical Staff Perspective
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 382
Publication Number: 382.133
Publication Number: 382.133
Katherine M. Redford, The Warren Alpert Medical School of Brown University, Providence, RI, United States; Randall Li, New York University Grossman School of Medicine, New York, NY, United States; Ana Malfa, The Warren Alpert Medical School of Brown University, Providence, RI, United States; Beatrice Lechner, Women & Infants Hospital of Rhode Island, Providence, RI, United States

Katherine M. Redford, DO
Neonatal-Perinatal Fellow
The Warren Alpert Medical School of Brown University
Providence, Rhode Island, United States
Presenting Author(s)
Background: In adults, code status and DNR orders have been established as an explicit guideline and are considered a component of the standard of care in the provision of quality end-of-life care. As most neonatal deaths occur after withdrawal of life-sustaining technology, DNR orders might not be as useful in the NICU population. It is unclear whether the presence of a DNR order impacts the quality of care provided at the end of life in the NICU and whether it impacts the experience of provision of care for NICU staff.
Objective: The aim of this study was to elucidate NICU staff perceptions of the value of the DNR order and their perception of the quality of care provided at the end of life.
Design/Methods: This study employed an online survey completed by neonatologists, neonatology fellows, and bedside nurses who cared for infants who died during their admission to the NICU at our single center. Results were analyzed using either the two-tailed t-test (when comparing continuous variables between two groups) or one-way ANOVA (when comparing continuous variables between three or more groups).
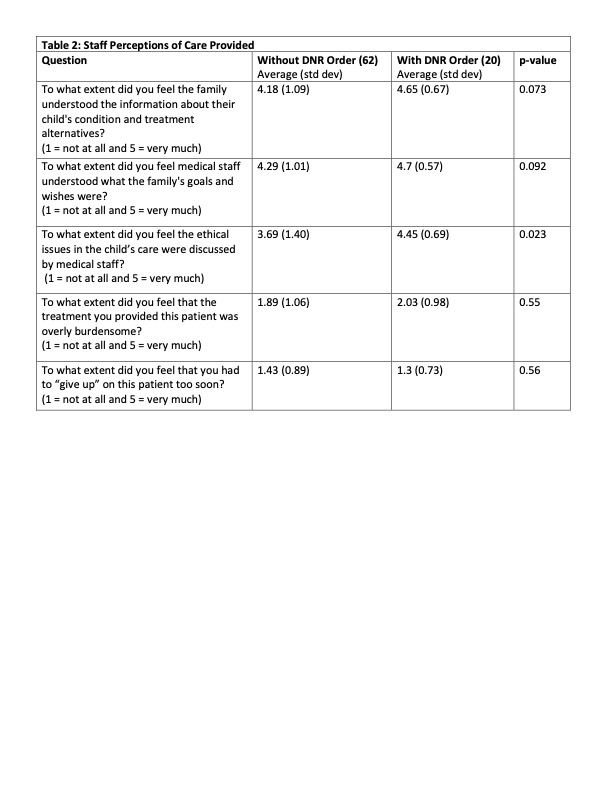
Results: 27 infants died during the study period. 85 participants who cared for these infants at the end of their life responded to the survey. Bedside nurses were significantly more likely than neonatologists or fellows to think that families would benefit from a DNR order (Table 1). Whether or not a provider believed the family would benefit from a DNR order was unrelated to their age or years in practice (Table 1). For infants who died with a DNR order versus those who died without a DNR order, there was no difference in staff perception of parent understanding of the clinical situation, of the medical staff’s understanding of the parents’ wishes, the level of burden unto the patient, or the sense of “giving up” on the patient too soon (Table 2). When caring for an infant with a DNR order, staff were more likely to state that there was sufficient discussion of the ethics surrounding the case (Table 2).Conclusion(s): Our results suggest that the presence of a DNR order does not affect the perception of quality of care an infant receives at the end of life in the NICU and that the perceived benefit of a DNR order varies based on role in the NICU.
Table 1: Staff Perceptions of Benefit of DNR Order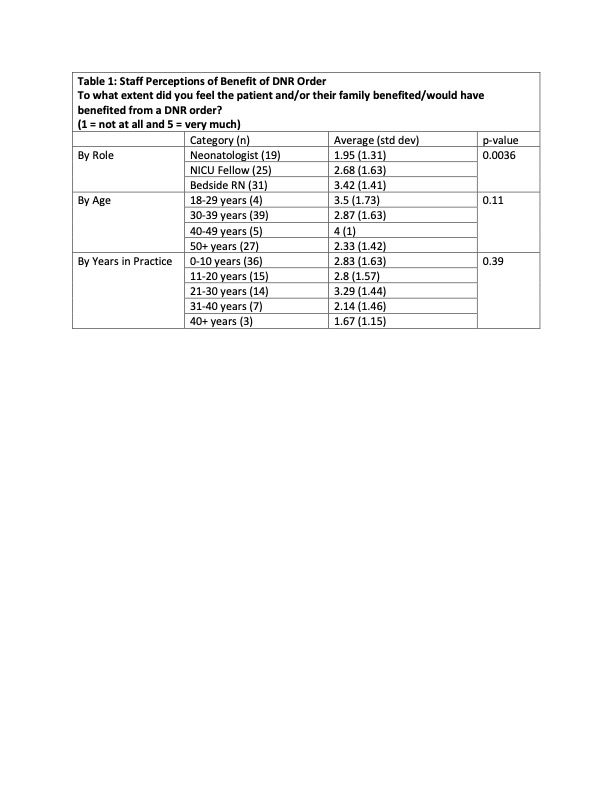
Table 2: Staff Perceptions of Care Provided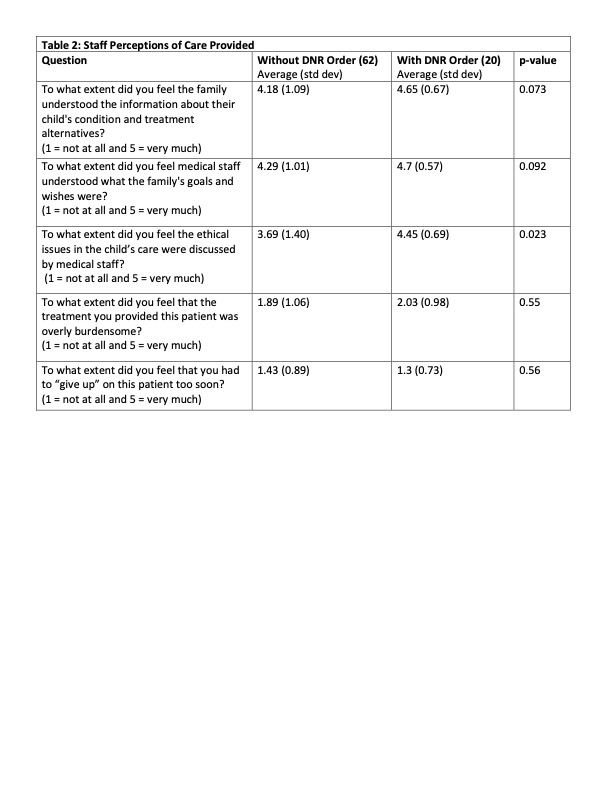
Objective: The aim of this study was to elucidate NICU staff perceptions of the value of the DNR order and their perception of the quality of care provided at the end of life.
Design/Methods: This study employed an online survey completed by neonatologists, neonatology fellows, and bedside nurses who cared for infants who died during their admission to the NICU at our single center. Results were analyzed using either the two-tailed t-test (when comparing continuous variables between two groups) or one-way ANOVA (when comparing continuous variables between three or more groups).
Results: 27 infants died during the study period. 85 participants who cared for these infants at the end of their life responded to the survey. Bedside nurses were significantly more likely than neonatologists or fellows to think that families would benefit from a DNR order (Table 1). Whether or not a provider believed the family would benefit from a DNR order was unrelated to their age or years in practice (Table 1). For infants who died with a DNR order versus those who died without a DNR order, there was no difference in staff perception of parent understanding of the clinical situation, of the medical staff’s understanding of the parents’ wishes, the level of burden unto the patient, or the sense of “giving up” on the patient too soon (Table 2). When caring for an infant with a DNR order, staff were more likely to state that there was sufficient discussion of the ethics surrounding the case (Table 2).Conclusion(s): Our results suggest that the presence of a DNR order does not affect the perception of quality of care an infant receives at the end of life in the NICU and that the perceived benefit of a DNR order varies based on role in the NICU.
Table 1: Staff Perceptions of Benefit of DNR Order
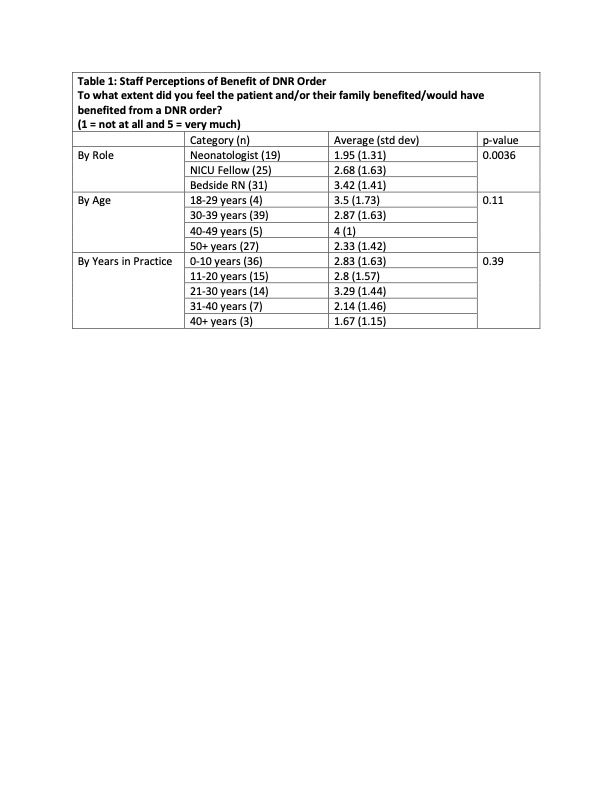
Table 2: Staff Perceptions of Care Provided