Emergency Medicine: All Areas
Category: Abstract Submission
4: Emergency Medicine I
48 - Trends in EMS and police utilization for transportation of pediatric patients with acute mental health needs to a pediatric emergency department
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 48
Publication Number: 48.103
Publication Number: 48.103
Alexandra Cheetham, Children's Cincinnati, Cincinnati, OH, United States; Rachel Bensman, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Victoria Hartwell, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Lauren C. Riney, Pediatric Emergency Medicine, Cincinnati, OH, United States; Sang Hoon Lee, University of Cincinnati College of Medicine, Cincinnati, OH, United States; Lynn Babcock, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Wendy Pomerantz, Cincinnati Children's Hospital, Cincinnati, OH, United States

Alexandra Cheetham, MD
Fellow
Cincinnati Children's Hospital
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Pediatric mental health (MH) visits historically account for 2-3% of pediatric emergency department (ED) visits, but numbers have been increasing in recent years. A significant portion of these patients arrive via Emergency Medical Services (EMS) and police, but there are few studies evaluating the impact of these patient encounters on EMS and police resource utilization.
Objective: To compare the epidemiology and trends in utilization for pediatric patients with acute MH needs transported to the ED by EMS or police with patients who self-transport.
Design/Methods: A retrospective cohort of patients 5-18 years old was assembled from patients presenting to a free-standing children’s hospital ED and its satellite ED with a MH chief complaint from January 1, 2012 to December 31, 2020. Data was obtained electronically from the hospital medical record. Patients with MH complaints were compared based on mode of arrival to the ED (EMS and police vs self-transport). Descriptive statistics were calculated and comparisons were made using Chi-square analysis for categorical variables and student’s t-test for continuous variables.
Results: During the study period 471,509 patients 5-18 years old presented to the ED; 70,557 (15%) had a MH chief complaint. Of all MH patients, 56,104 (79.5%) self-transported, 10,299 (14.6%) were transported by EMS, and 4,154 (5.9%) were transported by police. Between 2012 and 2020, visits for a MH complaint increased (figure). The proportion of these patients transported by EMS or police increased from 17.6% in 2012 to 20.1% in 2020, with a peak of 22% in 2018. As shown in table 1, patients transported by EMS were significantly older, more likely non-white, non-English speaking, and more likely to have public insurance than those who self-transported. Those transported by police were significantly older, more likely male, non-white, and more likely to have public insurance compared to patients who self-transported (table 2).Conclusion(s): EMS and police transports of patients with MH concerns are increasing. MH patients transported by EMS and police were older, non-white, and had public insurance. Targeted educational interventions and resources should address the specific needs of this population.
Figure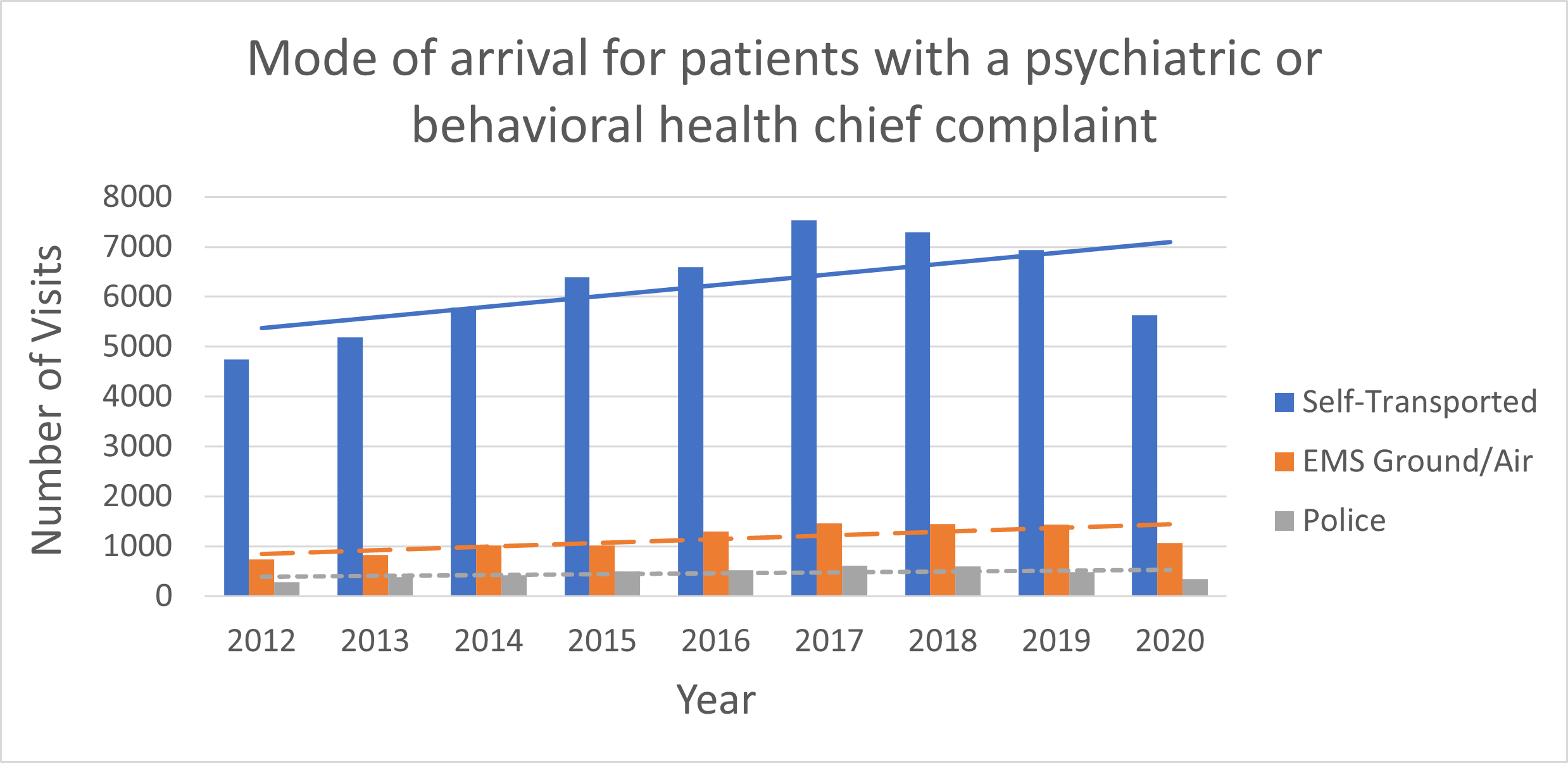 Yearly mode of arrival and trends over time of patients presenting with acute mental health needs
Yearly mode of arrival and trends over time of patients presenting with acute mental health needs
Table 1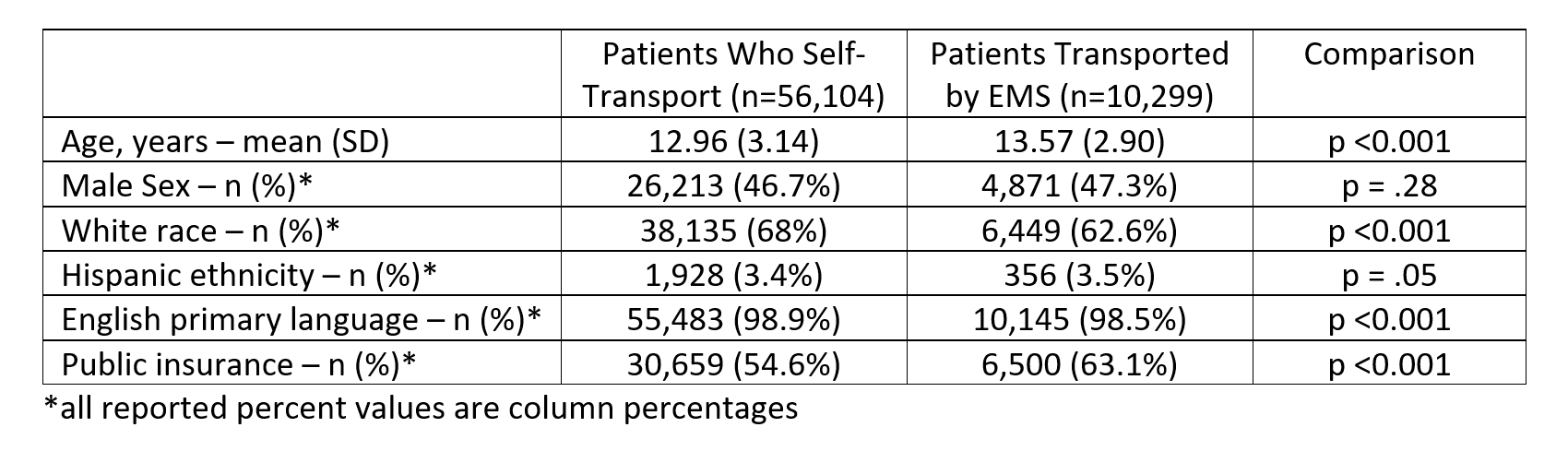 Demographics of mental health patients who self-transported compared to patients transported by EMS
Demographics of mental health patients who self-transported compared to patients transported by EMS
Objective: To compare the epidemiology and trends in utilization for pediatric patients with acute MH needs transported to the ED by EMS or police with patients who self-transport.
Design/Methods: A retrospective cohort of patients 5-18 years old was assembled from patients presenting to a free-standing children’s hospital ED and its satellite ED with a MH chief complaint from January 1, 2012 to December 31, 2020. Data was obtained electronically from the hospital medical record. Patients with MH complaints were compared based on mode of arrival to the ED (EMS and police vs self-transport). Descriptive statistics were calculated and comparisons were made using Chi-square analysis for categorical variables and student’s t-test for continuous variables.
Results: During the study period 471,509 patients 5-18 years old presented to the ED; 70,557 (15%) had a MH chief complaint. Of all MH patients, 56,104 (79.5%) self-transported, 10,299 (14.6%) were transported by EMS, and 4,154 (5.9%) were transported by police. Between 2012 and 2020, visits for a MH complaint increased (figure). The proportion of these patients transported by EMS or police increased from 17.6% in 2012 to 20.1% in 2020, with a peak of 22% in 2018. As shown in table 1, patients transported by EMS were significantly older, more likely non-white, non-English speaking, and more likely to have public insurance than those who self-transported. Those transported by police were significantly older, more likely male, non-white, and more likely to have public insurance compared to patients who self-transported (table 2).Conclusion(s): EMS and police transports of patients with MH concerns are increasing. MH patients transported by EMS and police were older, non-white, and had public insurance. Targeted educational interventions and resources should address the specific needs of this population.
Figure
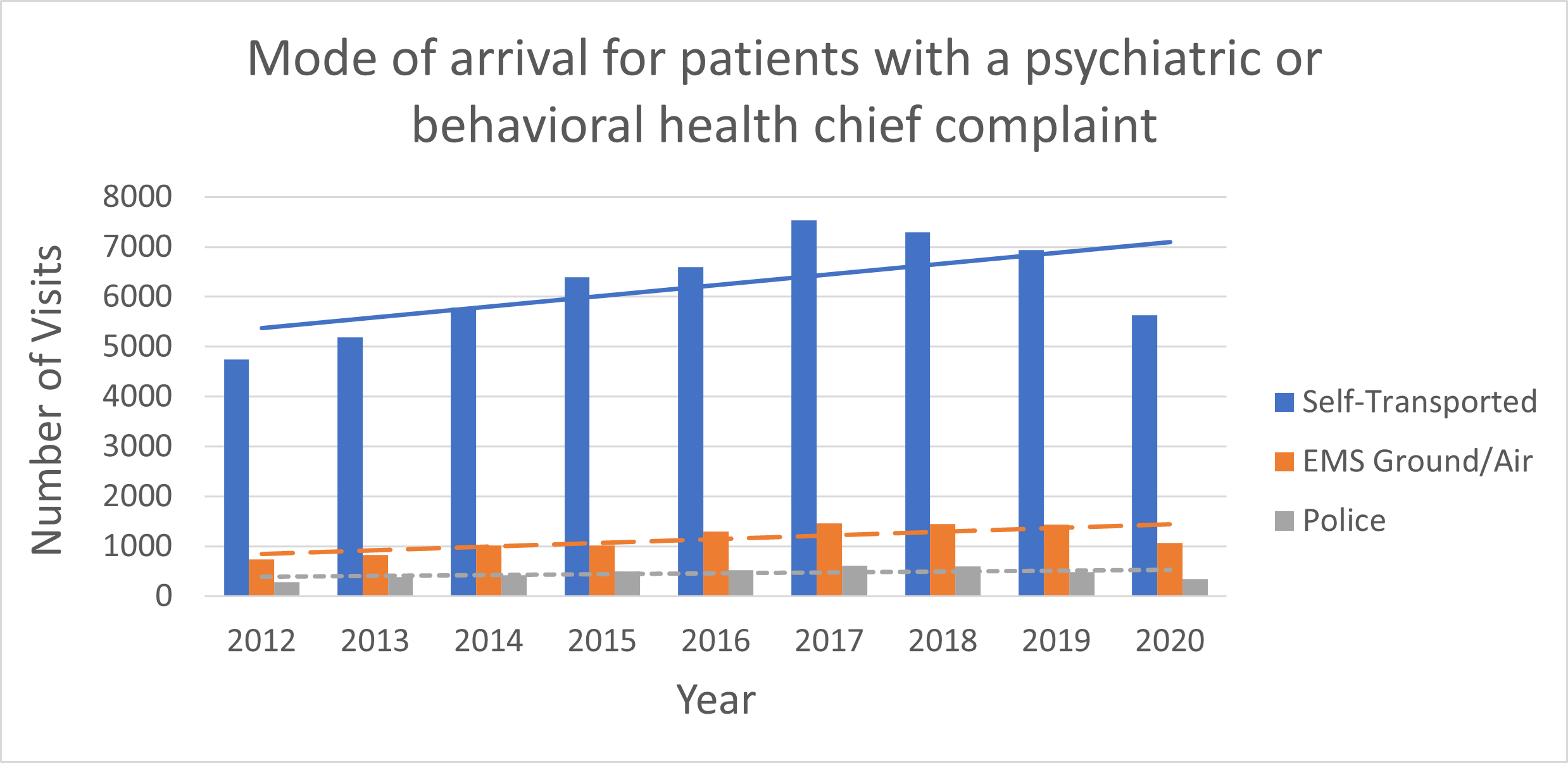 Yearly mode of arrival and trends over time of patients presenting with acute mental health needs
Yearly mode of arrival and trends over time of patients presenting with acute mental health needsTable 1
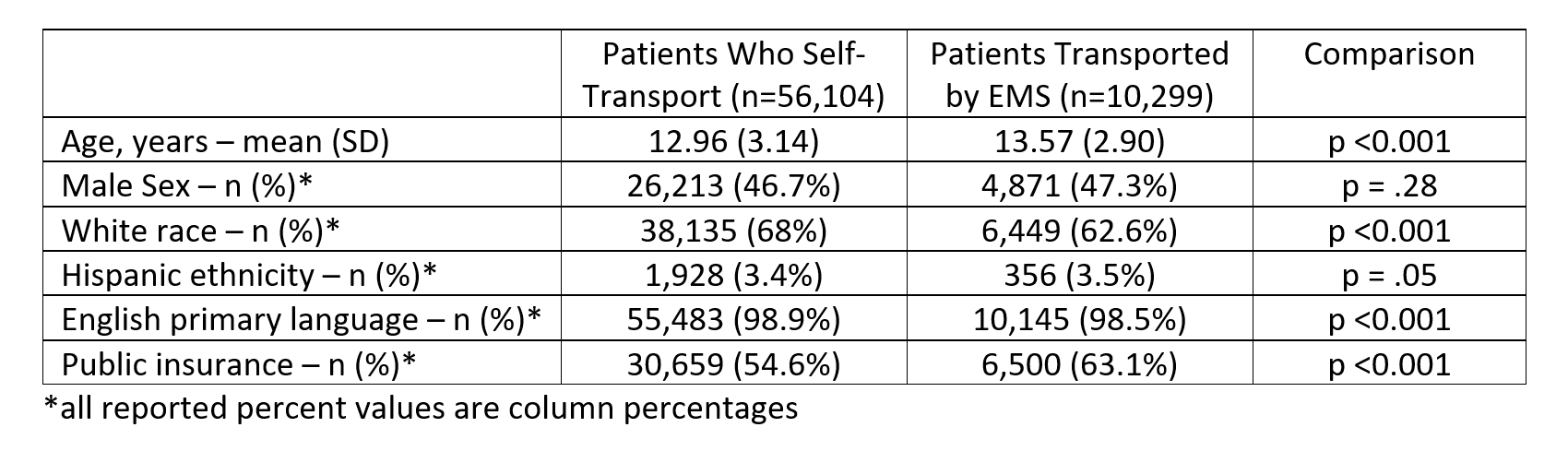 Demographics of mental health patients who self-transported compared to patients transported by EMS
Demographics of mental health patients who self-transported compared to patients transported by EMS